Retinal vasculopathy with cerebral leukoencephalopathy and systemic manifestations (RVCL-S) is an autosomal dominant microvasculopathy of the brain, retina, and other organ systems.
On this page:
Terminology
RVCL-S encompasses several previously described conditions 1,2, including cerebroretinal vasculopathy (CRV), hereditary vascular retinopathy (HVR), hereditary systemic angiopathy (HAS), hereditary endotheliopathy, retinopathy, nephropathy and stroke (HERNS), and retinal vasculopathy with cerebral leukodystrophy (RVCL) 3-6.
Epidemiology
RVCL-S is very are, and less than 50 families have been reported as being affected in the literature 11. However, the condition may be under-diagnosed 11.
Clinical presentation
Symptoms generally manifest between ages 30 and 50 years 1,2, and the most commonly reported clinical features helpfully appear in the condition's name:
retinal features: retinal hemorrhages and cotton wool spots may be seen on fundoscopy in the early stages before neovascularization and visual impairment (including eventual blindness) 1-6
CNS features: most commonly focal neurological deficits, but cognitive impairment and psychiatric disease are also common, and seizures and migraine with or without aura may also uncommonly occur 1,2,4-6
-
systemic features:
liver disease: due to microvascular liver disease 1,2,5
chronic kidney disease: due to arterio- or arteriolonephrosclerosis 1,2,4,5
hypertension 1,2
gastrointestinal bleeding: often microscopic due to angiodysplasia 1,2
anemia: due to gastrointestinal blood loss or secondary to inflammation 1,2
subclinical hypothyroidism 11
Pathology
Genetics
RVCL-S is an autosomal dominant disorder caused by C-terminal frameshift mutations in the three prime repair exonuclease 1 (TREX1) gene, located on the short arm of chromosome 3 1,2,6,7. The TREX1 gene normally encodes for a DNA exonuclease that is involved in removing unnecessary nucleotides from DNA 1,2,6,7. Furthermore, the TREX1 gene also plays a role in protein glycosylation 9. It is unclear which of these functions (or perhaps both) is important to lose in the development of RVCL-S.
Importantly, these mutations in TREX1 are distinct from those in the same gene that cause Aicardi-Goutiéres syndrome and some cases of hereditary systemic lupus erythematosus 8.
Microscopic appearance
Affected tissue, such as cerebral white matter, demonstrate ischemia, necrosis, and dystrophic calcifications, with accompanying vasculopathy 1,7. This vasculopathy, affecting primarily small to medium sized vessels, manifests as fibrinoid vascular necrosis or thickened hyalinised vessels, notably without evidence of vasculitis 1,7. In the brain, the leptomeninges, extraparenchymal vasculature, and the cortical grey matter vessels are typically spared 1,7.
Radiographic features
Neuroimaging features have been most commonly described 1,2,6,11.
CT
CT is non-specific, but approximately half of all patients demonstrate multiple intracerebral calcifications in the cerebral white matter 1,2,5,6,11.
MRI
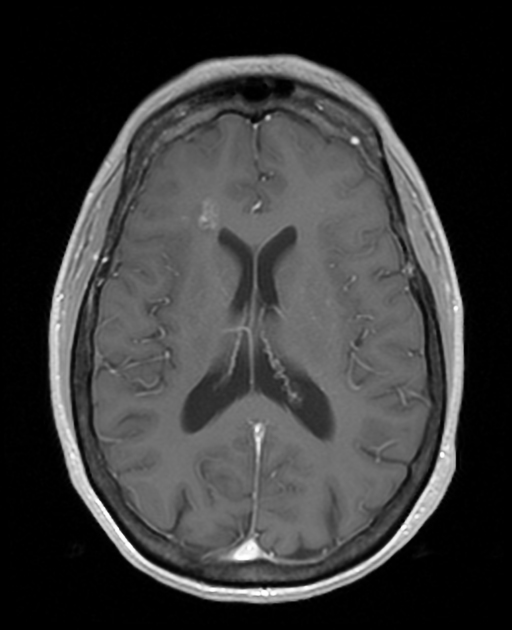
Characteristic white matter lesions have been described:
-
punctate supratentorial white matter lesions that spare the grey matter and subcortical U-fibers, and are incompatible for age 1,2,6
T2/FLAIR: hyperintense
-
DWI: may or may not have high diffusion signal
some of these lesions are small ischemic strokes
T1 C+ (Gd): may or may not have nodular or rim enhancement
-
larger white matter mass-like ('pseudotumor') lesions that have perilesional edema and exhibit mass effect, which may progressively increase in size and number over time, some of these may develop from the aforementioned punctate white matter lesions 1,2,6,10-12
T2/FLAIR: hyperintense
DWI: may not demonstrate high diffusion signal
GRE/SWI: may have associated punctate regions of susceptibility artifact, which may represent cerebral microhemorrhages or calcifications
-
T1 C+ (Gd): typically demonstrate ring enhancement
initially non-enhancing lesions can progress to enhancing or rim-enhancing lesions
As the disease progresses, similar punctate lesions may be seen within the cerebellum, although mass-like lesions are very rare 11.
Treatment and prognosis
There is no disease-modifying therapy available 11. Immunosuppressive strategies have been trialed without definite benefit 11. Typically, the disease has a progressive course leading to death between ages 50 and 60, which corresponds to approximately a decade after symptom onset 1,2,6.
History and etymology
RVCL-S was coined by Anine H Stam and colleagues in their 2016 seminal paper 1, thereby uniting multiple previously separate pathologies.
Differential diagnosis
General imaging differential considerations include:




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.