Spondylodiscitis, (rare plural: spondylodiscitides) also referred to as discitis-osteomyelitis, is characterized by infection involving the intervertebral disc and adjacent vertebrae.
On this page:
Terminology
In adults, the use of the term discitis is generally discouraged as isolated infection of the spinal disc is a rare phenomenon. In general, the vertebral endplate is infected first with secondary involvement of the disc. For this reason terms such as spondylodiscitis or vertebral osteomyelitis are preferred due to their greater accuracy 18. If Mycobacterium tuberculosis is the causative organism of the spinal infection then it is also known as Pott disease 21.
Epidemiology
Spondylodiscitis has a bimodal age distribution, which many authors consider to be separate entities:
pediatric
older population ~50 years
Risk factors
remote infection (present in ~25%)
ascending infection, e.g. from urogenital tract instrumentation
spinal instrumentation or trauma
long term systemic administration of steroids
advanced age
organ transplantation
malnutrition
Clinical presentation
The typical presentation is back pain (over 90% of patients) and less common fever (under 20% of patients). Patients are often bacteremic from sources such as endocarditis and intravenous drug use (IVDU).
Biochemical markers
Elevated serum C-reactive protein and/or erythrocyte sedimentation rate.
Pathology
In the pediatric age group infection often starts in the intervertebral disc itself (direct blood supply still present) whereas in adults, infection is thought to begin at the vertebral body endplate, extending into the intervertebral disc space and then into the adjacent vertebral body endplate.
Etiology
Staphylococcus aureus (most common; 60%)
Streptococcus viridans (IVDU, immunocompromised)
gram-negative organisms, e.g. Enterobacter spp., E. coli
Mycobacterium tuberculosis (Pott disease) 21,22
-
less common organisms
-
fungal
Cryptococcus neoformans
Candida spp.
Histoplasma capsulatum
Coccidioides immitis
Burkholderia pseudomallei (i.e. melioidosis): diabetic patients from northern Australia and parts of Southeast Asia
Brucella spp.
-
-
in patients with sickle cell disease consider Salmonella spp.
although other organisms may also cause
Location
can occur anywhere in the vertebral column but more commonly involves lumbar spine
single level involvement (65%)
multiple contiguous levels (20%)
multiple non-contiguous levels (10%)
Radiographic features
Plain radiograph
Plain radiography is insensitive to the early changes of spondylodiscitis, with normal appearances being maintained for up to 2-4 weeks. Thereafter disc space narrowing and irregularity or ill definition of the vertebral endplates can be seen. In untreated cases, bony sclerosis may begin to appear in 10-12 weeks.
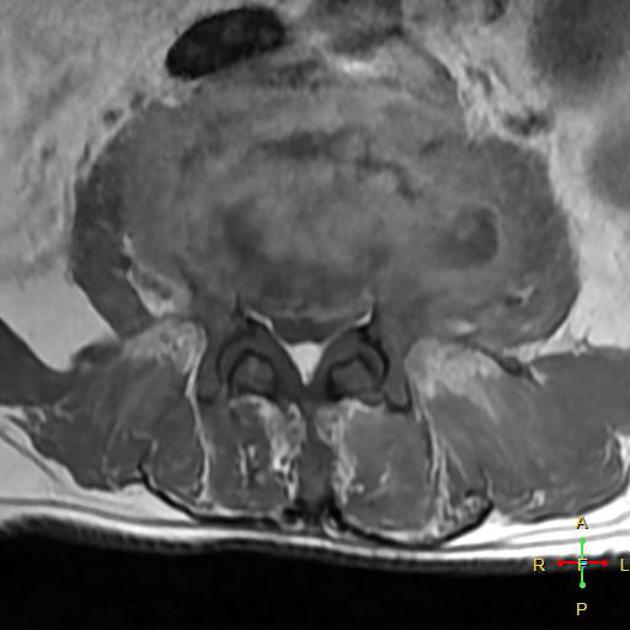
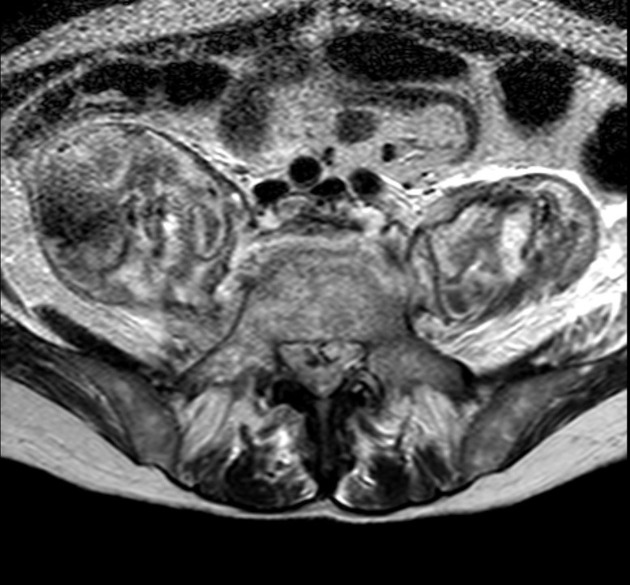
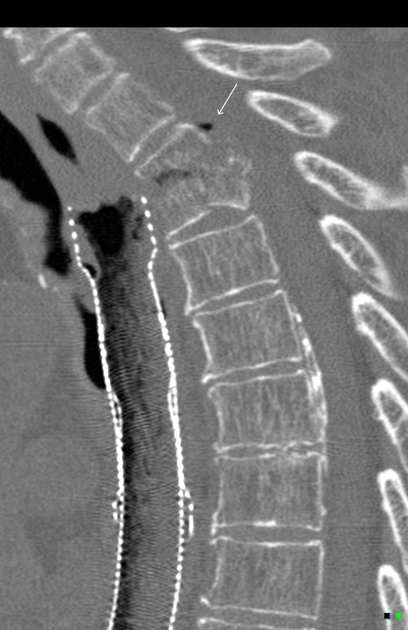
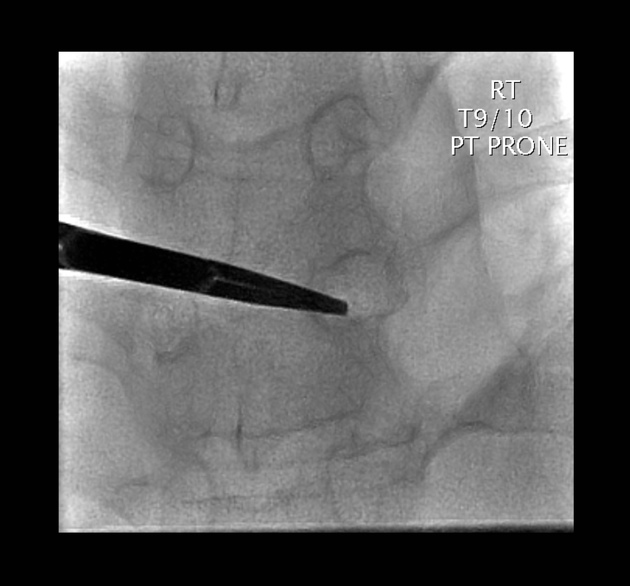
CT
CT findings are similar to plain film but are more sensitive to earlier changes. Additionally, surrounding soft tissue swelling, intervertebral disc enhancement with contrast, collections (e.g. paraspinal and psoas muscle abscesses), and even epidural abscesses may be evident.
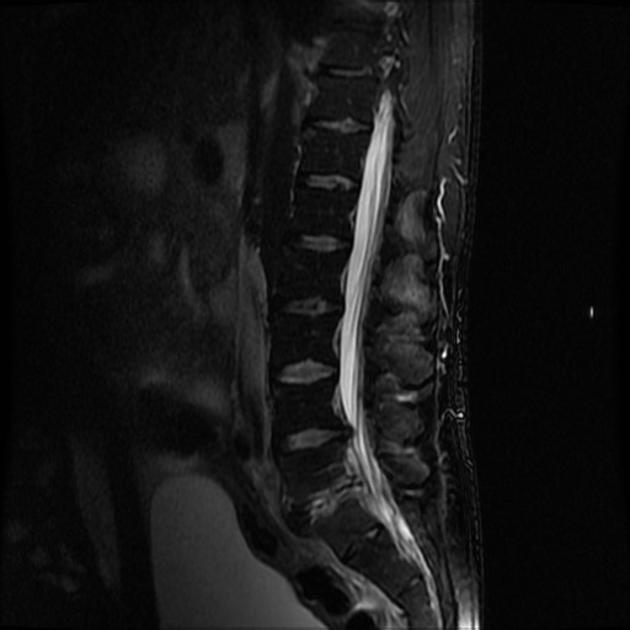
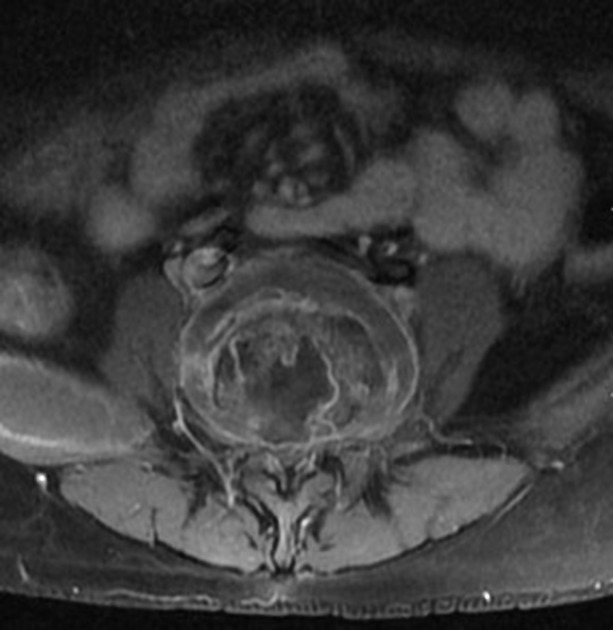
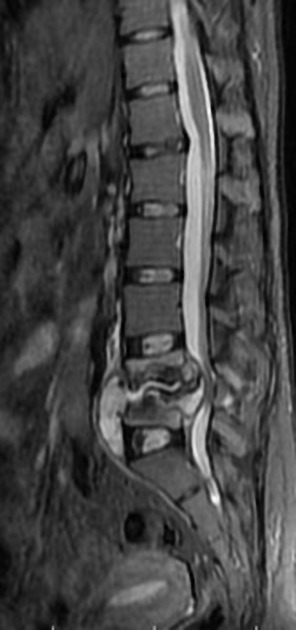
MRI
MRI is the imaging modality of choice due to its very high sensitivity and specificity. It is also useful in differentiating between pyogenic, tuberculous, and fungal infections, and a neoplastic process.
Signal characteristics include:
-
T1
low signal in disc space (fluid)
low signal in adjacent endplates (bone marrow edema)
-
T2: (fat saturated or STIR especially useful)
high signal in disc space (fluid)
high signal in adjacent endplates (bone marrow edema)
loss of low signal cortex at endplates
high signal in paravertebral soft tissues
hyperintensity within the psoas muscle (imaging psoas sign): this finding is ~92% sensitive and ~92% specific for spondylodiscitis
-
T1 C+ (Gd)
peripheral enhancement around fluid collection(s)
enhancement of vertebral endplates
enhancement of paravertebral soft tissues
enhancement around low-density center indicates abscess formation (hard to distinguish inflammatory phlegmon from abscess without contrast)
-
DWI
hyperintense in the acute stage
hypointense in the chronic stage
The DWI sequence can help to distinguish between the acute and chronic stages of the disease 7.
Nuclear medicine
A bone scan and white cell (WBC) scan may be used to demonstrate increased uptake at the site of infection, and are more sensitive than plain film and CT, but lack specificity. Not infrequently, a WBC scan demonstrates cold spots, a non-specific finding. The classic appearance on multiphase bone scans is increased blood flow and pool activity and associated increased uptake on the standard delayed static images 15. Gallium-67 citrate has been used with some success but is hampered by higher dosages and inferior imaging characteristics (high effective dose, long half-life time, poor spatial resolution) 14,15.
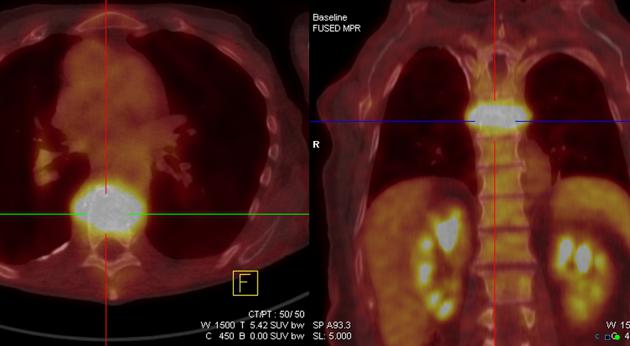
PET
F-18-FDG PET has been demonstrated to possess high sensitivity in detecting spondylodiscitis. As such, infectious spondylodiscitis can virtually be excluded by a negative scan. Dual imaging with PET-CT may thus become the imaging modality of choice, especially in patients with prior surgery and/or implants, where MRI is contraindicated or hampered by artifact 8-11. Specificity is not as high 10,16, but monitoring of treatment results is possible 9.
Non-FDG PET-CT with Ga-68 citrate (an emerging, generator-based tracer) has shown promising results in pilot studies/small series 12,13.
PET-MRI has shown promise for indeterminate cases of spondylodiscitis 20.
Differential diagnosis
Possible imaging differential considerations include 19:






















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.