Superior mesenteric artery (SMA) syndrome, also known as Wilkie syndrome, cast syndrome or aortomesenteric duodenal compression syndrome, is a rare acquired vascular compression disorder in which acute angulation of the superior mesenteric artery (SMA) results in compression of the third part of the duodenum, leading to obstruction.
On this page:
Terminology
Superior mesenteric artery syndrome should not be confused with nutcracker syndrome (which can be an association), also a superior mesenteric artery compression disorder, where the superior mesenteric artery compresses the left renal vein, although some authors use the terms interchangeably.
Epidemiology
It is an uncommon but a well-recognized clinical entity. About 400 cases have been described in the English literature. It is seen more commonly in females than in males and usually occurs in older children and adolescents.
Clinical presentation
Patients with superior mesenteric artery syndrome may present acutely, with chronic insidious symptomatology, or with an acute exacerbation of chronic symptoms:
acute presentation is usually characterized by signs and symptoms of duodenal obstruction
chronic cases may present with long-standing vague abdominal symptoms, early satiety and anorexia, or recurrent episodes of abdominal pain, associated with vomiting
Pathology
Fat and lymphatic tissues around the superior mesenteric artery provide protection to the duodenum against compression. Under conditions of severe weight loss, this cushion around the superior mesenteric artery is diminished, causing angulation and reduction in the distance between the aorta and the superior mesenteric artery. This is usually associated with conditions causing significant weight loss such as:
malabsorption
hypercatabolic states (burns, major surgery, malignancy)
severe congestive heart failure causing cachexia
Other conditions may also precipitate this syndrome:
increased spinal lordosis
application of a body cast
short ligament of Treitz
multiple attachments of the ligament of Treitz to the duodenum
high fixation of the duodenum by the ligament of Treitz
unusually low origin of superior mesenteric artery
an anomalous superior mesenteric artery crossing directly over the aorta
associated with diabetes mellitus and blunt abdominal trauma
Radiographic features
The diagnosis of superior mesenteric artery syndrome is based on clinical symptoms and radiologic evidence of obstruction.
Plain radiograph
The stomach and proximal duodenum are dilated, and filled with gas and/or fluid.
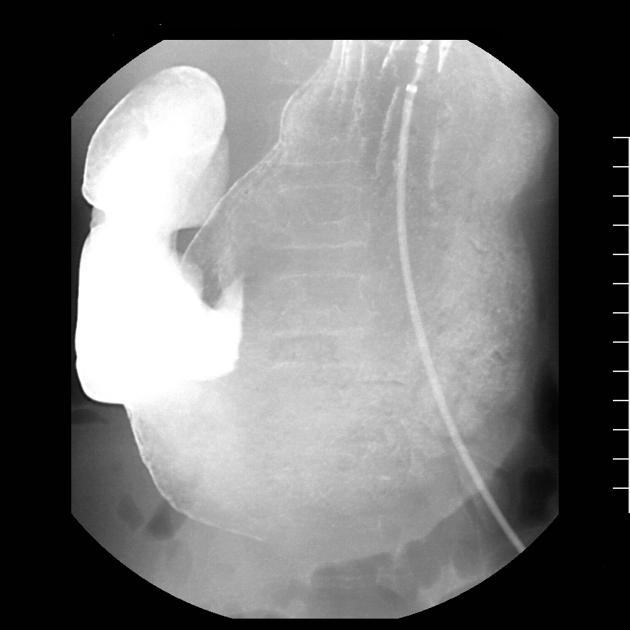
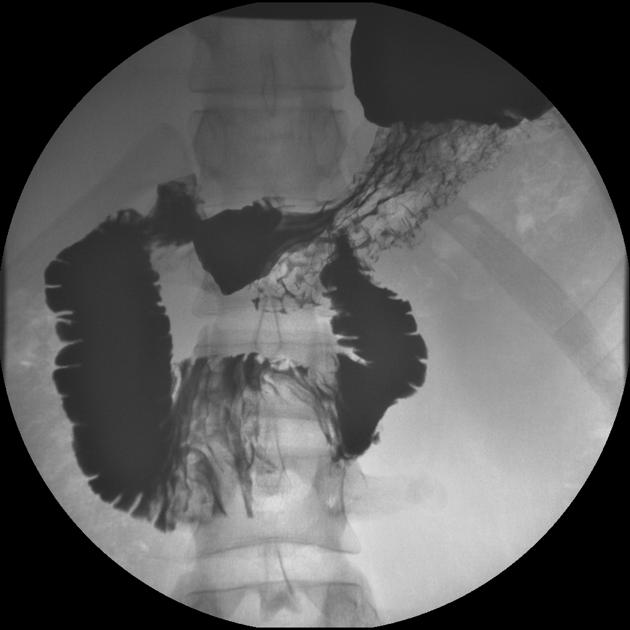
Fluoroscopy
Upper GI fluoroscopy can demonstrate dilatation of the first and second part of the duodenum, extrinsic compression of the third part, and a collapsed small bowel distal to the crossing of the superior mesenteric artery.
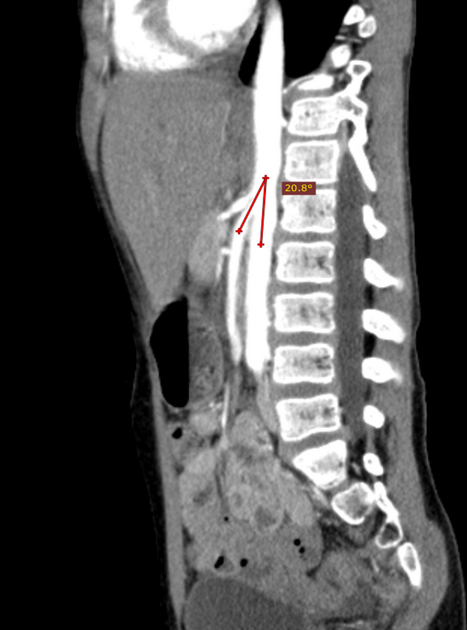
CT/MRI
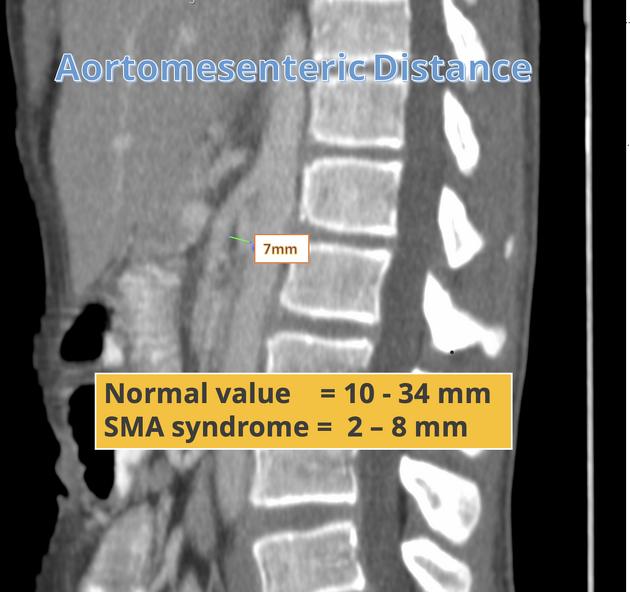
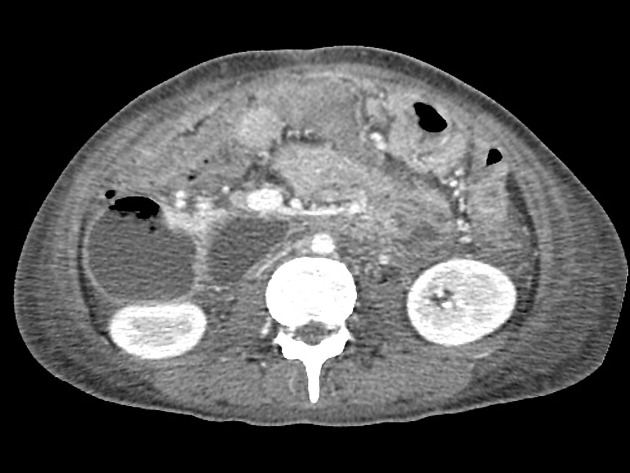
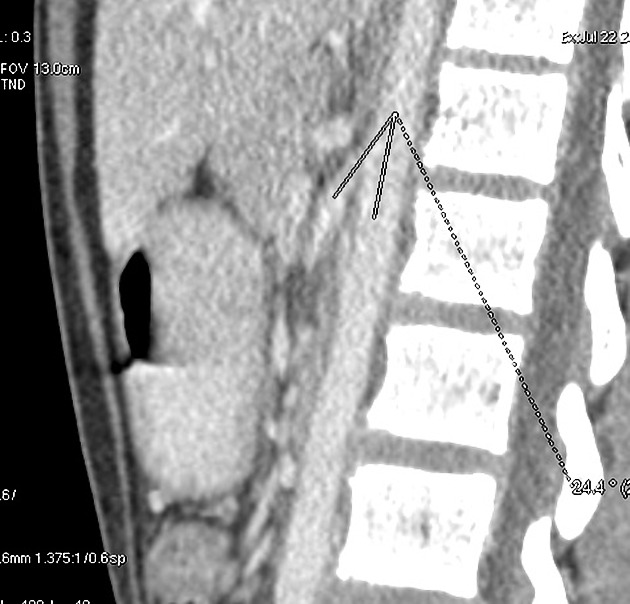
CT and magnetic resonance angiography (CTA/MRA) enable visualization of vascular compression of the duodenum and measurement of aortomesenteric distance:
normally, the aortomesenteric angle and aortomesenteric distance are 28-65° and 10-34 mm, respectively 6
in superior mesenteric artery syndrome, both parameters are reduced, with values of 6° to 22° and 2 to 8 mm 6
Ultrasound
Ultrasound is an additional modularity that can be used in the diagnosis of superior mesenteric artery syndrome. Characteristic findings include reduction of the aortic-mesenteric angle (angle <25° with the aorto-mesenteric distance <8–10 mm). Standing and supine positioning may assist the diagnosis - with angle reductions on supine projections 7.
Not all patients with angles less than 25 and a distance with 8-10mm will have superior mesenteric artery syndrome - thus findings should be interpreted in conjunction with their symptoms
History and etymology
Superior mesenteric artery syndrome was first described by Baron Carl von Rokitansky (1804-1878), Bohemian pathologist, in 1861. Later, Sir David Percival Dalbreck Wilkie (1882-1938), English surgeon, provided a more detailed clinical and pathophysiologic description in a series of 75 patients in 1927 and suggested treatment approaches 4,5.
Treatment and prognosis
Traditionally, treatment has consisted of conservative measures such as:
start with medical management, including decompression of the stomach and duodenum with a nasogastric tube, correction of nutritional and electrolytes deficiencies, through total parenteral nutrition, or preferably, if possible, enteral feeding with a nasojejunal tube past the point of compression, which fulfills nutritional requirements while avoiding the complications of total parenteral nutrition. When tolerated, oral feeding may be resumed. This helps build up the fat cushion between the superior mesenteric artery and aorta and, hence, may help in reversing the situation.
posturing maneuvers during meals and motility agents may be helpful in some patients
lying in right decubitus position may relieve compression of duodenum
Surgery may be considered if conservative treatment fails:
duodenojejunostomy is effective in the majority of patients
laparoscopic duodenojejunostomy offers a new minimally invasive therapeutic approach to superior mesenteric artery syndrome
laparoscopic surgery involving lysis of the ligament of Treitz with the mobilization of the duodenum is another minimally invasive approach
Differential diagnosis
Other disorders which can present in a similar manner include:
diabetic gastroparesis
hereditary megaduodenum
megaduodenum due to aganglionosis.
The distinction between these entities and superior mesenteric artery syndrome is important, particularly if surgical intervention is being considered.





















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.