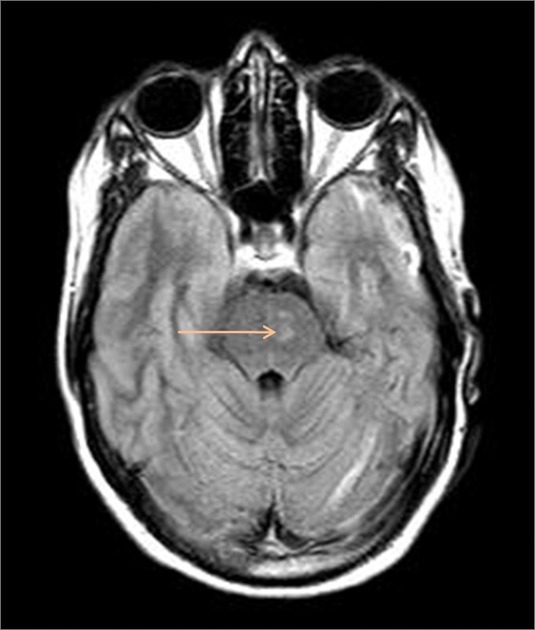
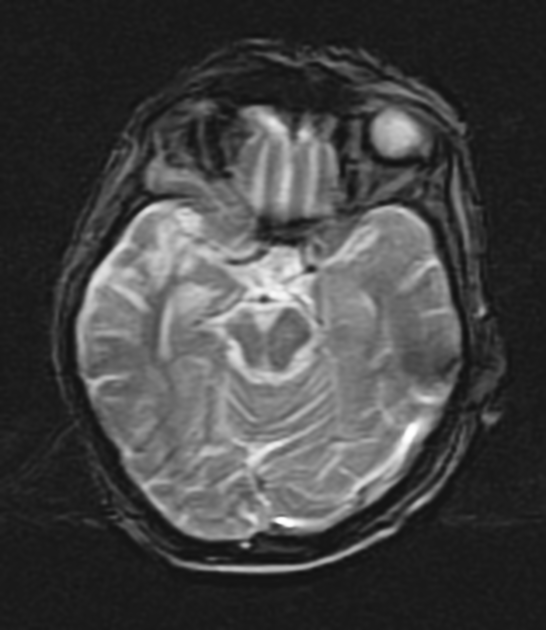
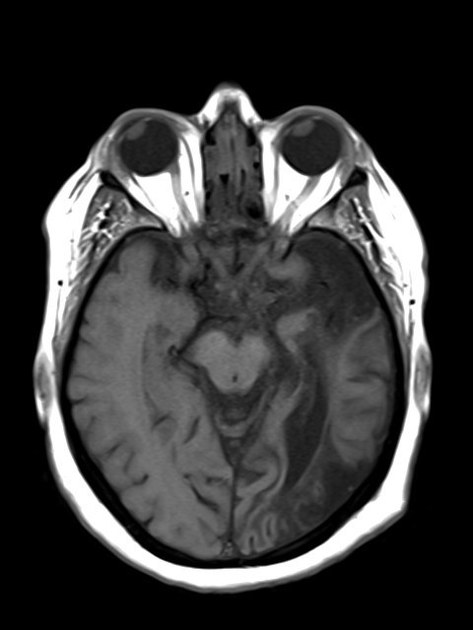
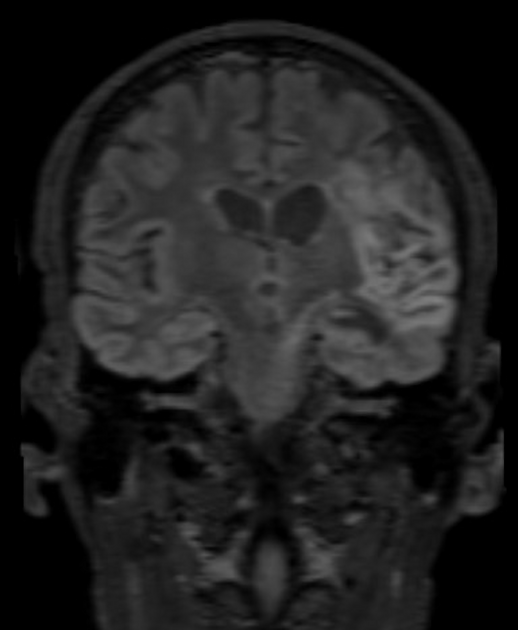
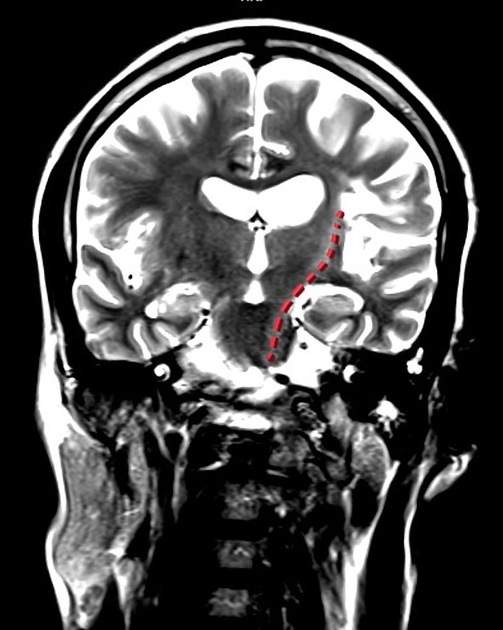
Wallerian degeneration is the process of antegrade degeneration of the axons and their accompanying myelin sheaths due to a proximal axonal or neuronal cell body insult. It may result following neuronal loss due to cerebral infarction, trauma, necrosis, focal demyelination, or hemorrhage.
On this page:
Pathology
Wallerian degeneration is an evolving process that can be arbitrarily divided into multiple descriptive stages for convenience. A number of publications, for example, have divided into four stages 2,3:
stage 1 (0-4 weeks): degeneration of the axons and myelin sheaths with mild chemical changes
stage 2 (4-14 weeks): rapid destruction of myelin protein fragments that were already degenerated, lipids remain intact
stage 3 (>14 weeks): gliosis replaces the degenerated axons and myelin sheaths, myelin lipid breakdown
stage 4 (months to years): atrophy of the white matter tracts
Distribution
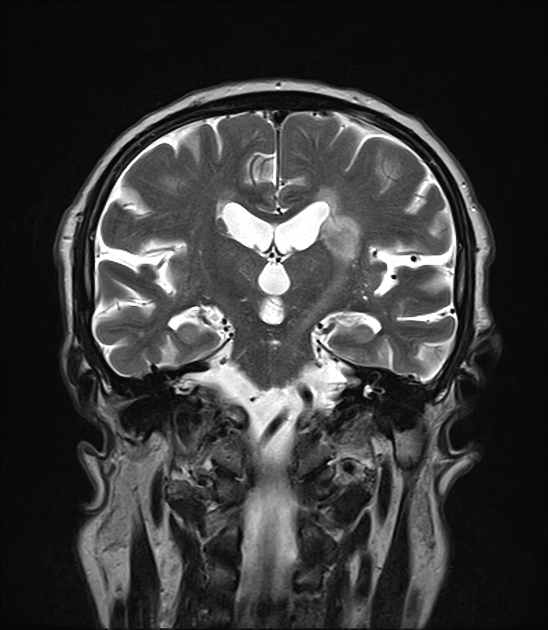
The distribution of Wallerian degeneration depends on the region of injury and how it relates to white matter tracts that originate there. The most commonly observed pattern is an injury to the precentral gyrus (such as may be seen in an MCA infarct) with resultant degeneration of the corticospinal tracts.
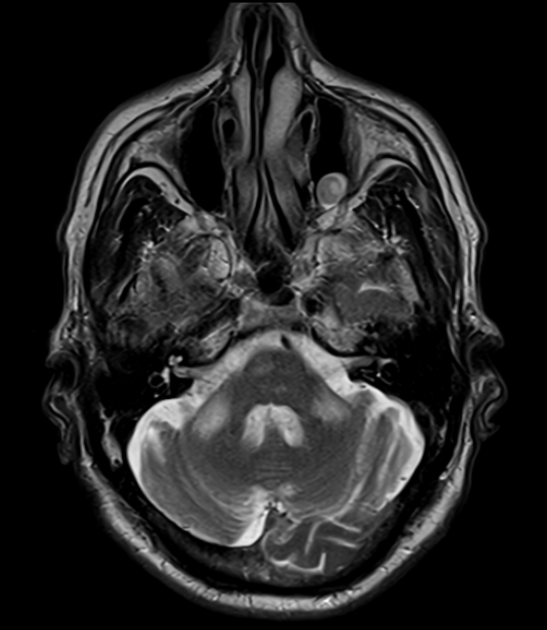
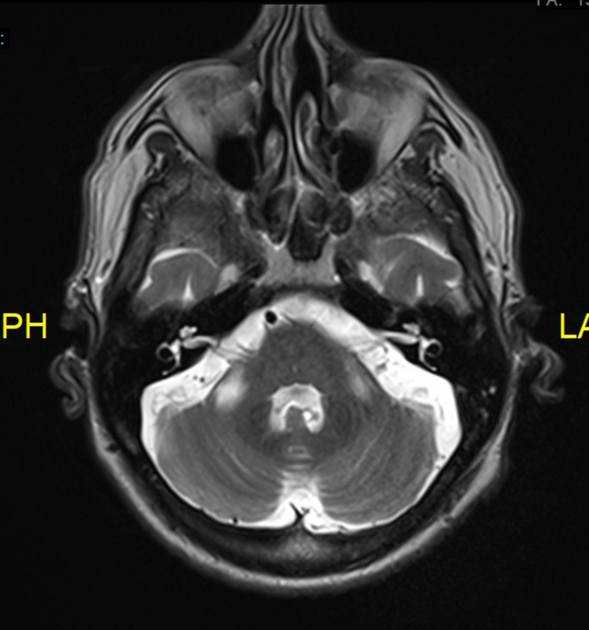
Infarction of the ventral pons (basis pontis), even if unilateral, can lead to bilateral middle cerebellar peduncle lesions due to Wallerian degeneration of the pontocerebellar fibers 10.
In the cord, Wallerian degeneration can occur both rostrally (involving the dorsal columns above the injury) and caudally (involving the lateral corticospinal tracts below the injury) 8.
Radiographic features
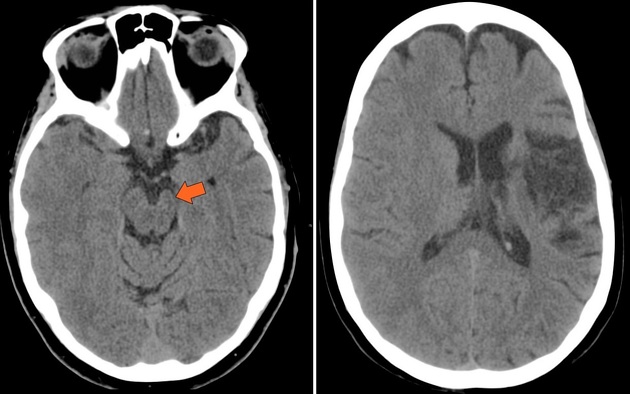
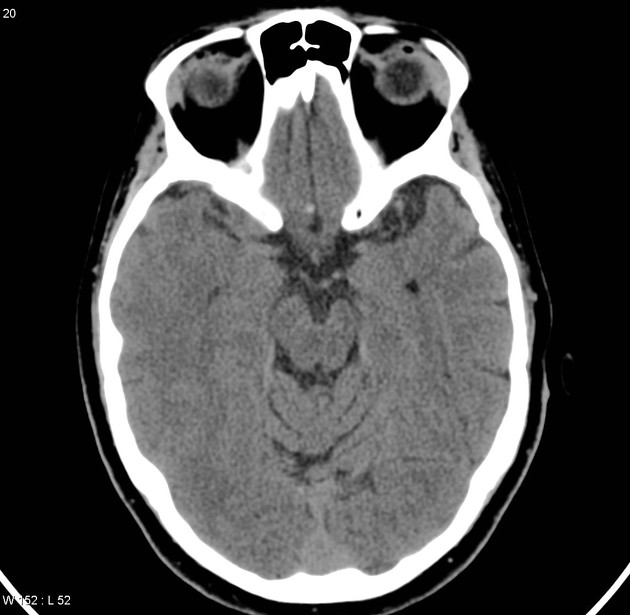
CT
CT is not as sensitive as MRI, and Wallerian degeneration is generally observed only in its chronic stage. It is seen as a contiguous tract of gliosis leading from a region of cortical or subcortical neuronal injury towards the deep cerebral structures, along the expected topographical course of the involved white matter tract.
MRI
Corresponding stages have been described on MRI 2,3.
-
T1
stage 1: no changes
stage 2: T1 hyperintense
stage 3: T1 hypointense
stage 4: brainstem atrophy with or without hypointensity
-
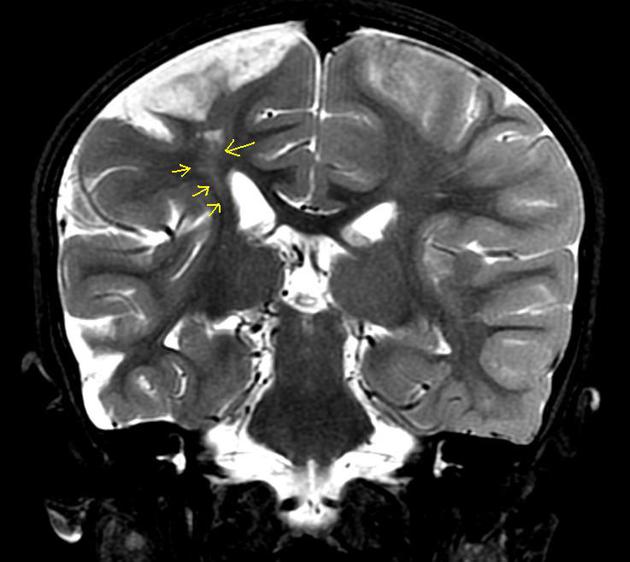
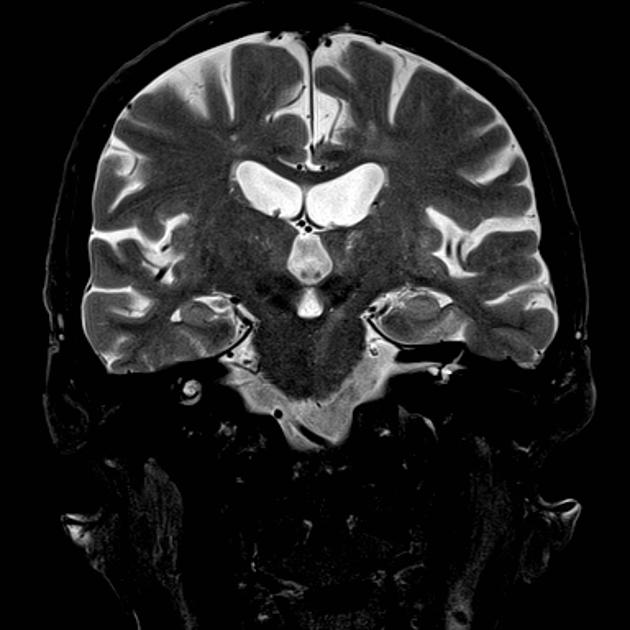
T2
stage 1: no changes
stage 2: T2 hypointense
stage 3: T2 hyperintense
stage 4: brainstem atrophy
DWI: high signal on DWI and low signal on ADC have been demonstrated along the affected white matter tracts, from the first days after insult until 8 months after 7
History and etymology
It is named after the English neurophysiologist Augustis Volney Waller (1816-1870), who described the process in 1850 6.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.