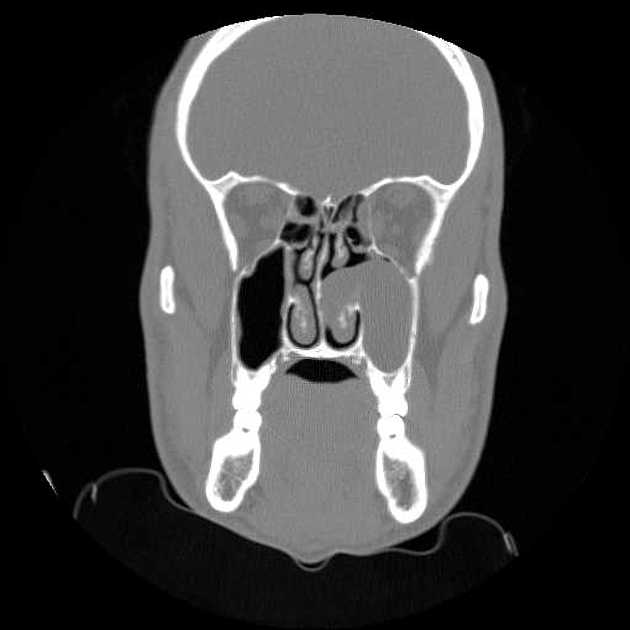
Antrochoanal polyps (ACP) are solitary sinonasal polyps that arise within the maxillary sinus (antrum). They pass through and enlarge the sinus ostium and posterior nasal cavity at the level of the choana.
Similar, less common, polyps can arise in the sphenoid sinus extending into the nasopharynx: these are termed sphenochoanal polyps. Likewise, there are nasochoanal, frontochoanal, and ethmochoanal polyps 9.
On this page:
Epidemiology
Antrochoanal polyps represent only ~5% of sinonasal polyps 3. They are most commonly seen in young adults in their 3rd to 5th decades. They are slightly more common in males than females 3.
Clinical presentation
Clinical presentation is usually with an obstructed nasal passage and/or sinus symptoms. Occasionally, larger masses may prolapse posteriorly enough that they may be visible through the mouth as they hang down from the nasopharynx 5.
Unlike other sinonasal polyps, antrochoanal polyps are usually found in non-atopic patients 3.
Pathology
The exact etiology is not known, but it is thought that infection may be a common causative association. Chronic sinusitis is present in ~25% of patients 7 but a causal relationship has not been firmly established.
Pathologically, antrochoanal polyps are identical to other inflammatory polyps. However, unlike other polyps, they usually have a narrow stalk arising from the maxillary sinus 5,7.
Microscopic appearance
Histologically, the polyp is lined by respiratory epithelium with increased inflammatory infiltrate. Due to the narrow pedicle, vascular compromise with secondary change may be seen. This may result in hemorrhage, organizing hematoma, neovascular changes, and/or papillary endothelial hyperplasia 5,7.
Radiographic features
Plain radiograph
Plain films are no longer considered adequate in the assessment of sinus pathology. However, they continue to be performed in some cases. Findings include 3:
unilateral opacification of the maxillary sinus
nasopharyngeal mass is occasionally seen
frequently, bilateral sinus involvement (23-42%) 3
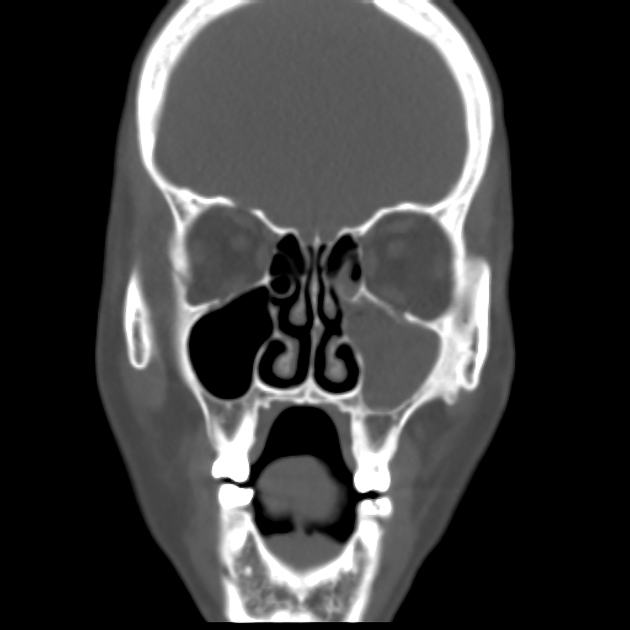
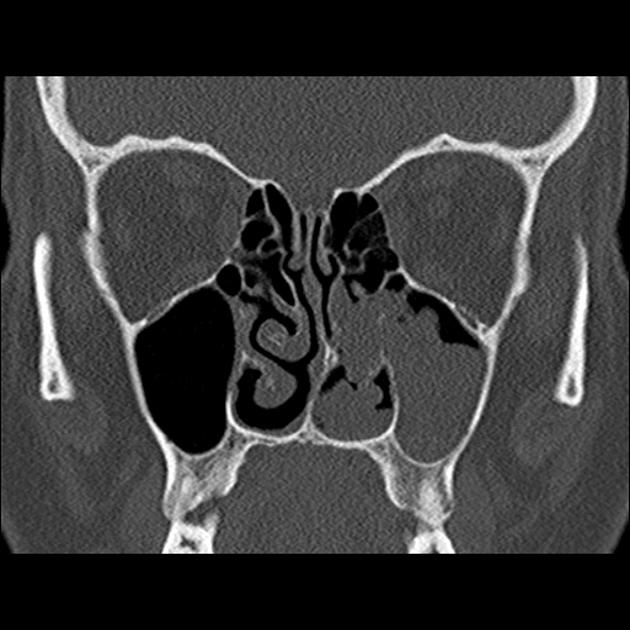
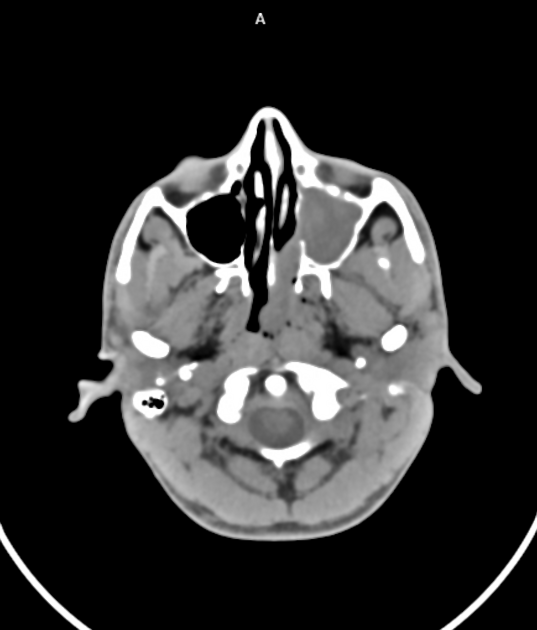
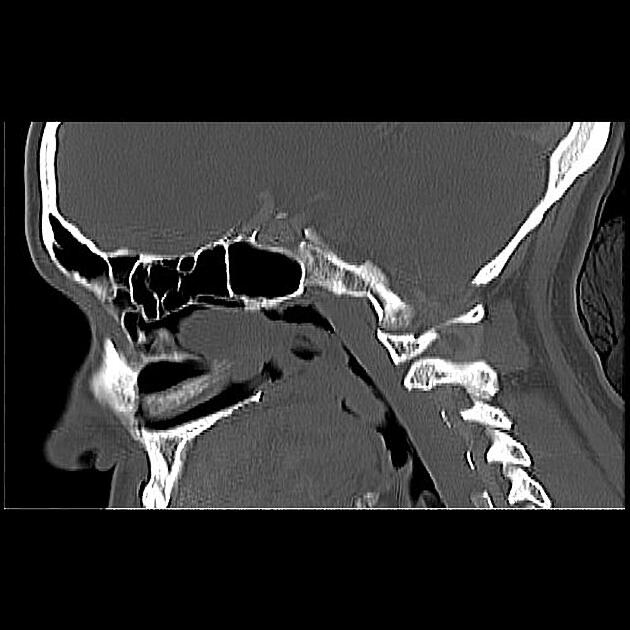
CT
CT is the preferred method for diagnosis due to the exquisite bony detail of the paranasal sinus anatomy. In general, a non-contrast scan is sufficient. Typically, antrochoanal polyps have the following features:
defined mass with mucin density is seen arising from the maxillary sinus
widening of the maxillary antrum or accessory ostium and extension into the nasopharynx
no associated bony destruction but rather smooth enlargement of the sinus
These features are best appreciated on true coronal or coronal reformatted scans. Although pathologically antrochoanal polyps have a narrow pedicle or stalk, this is usually not evident on CT.
Occasionally, antrochoanal polyps may have a higher density (and Hounsfield values) if they are long-standing (i.e. desiccated) and/or have an associated fungal infection (see fungal sinusitis) 1. A contrast-enhanced scan is not necessary but may demonstrate peripheral enhancement.
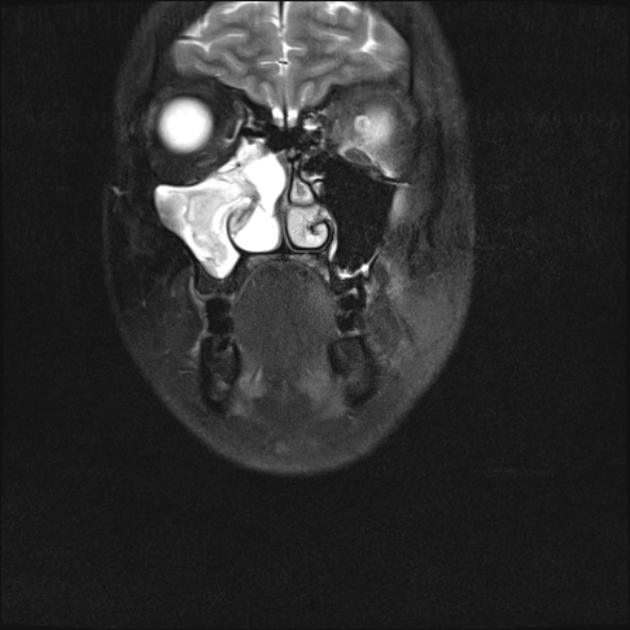
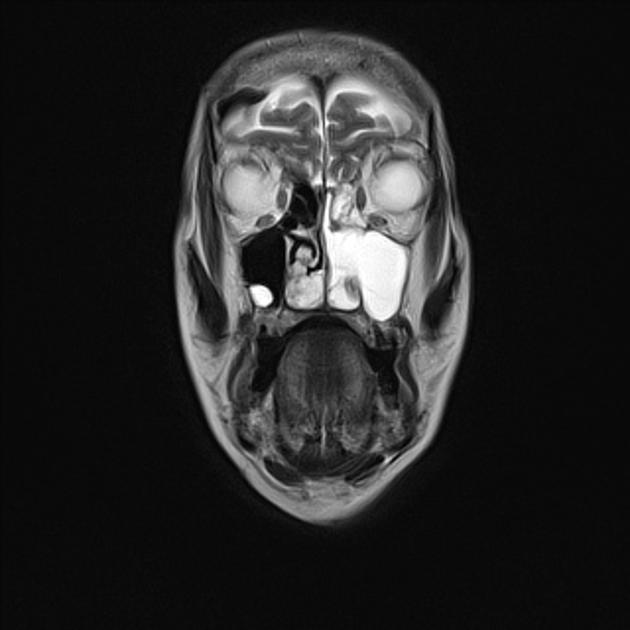
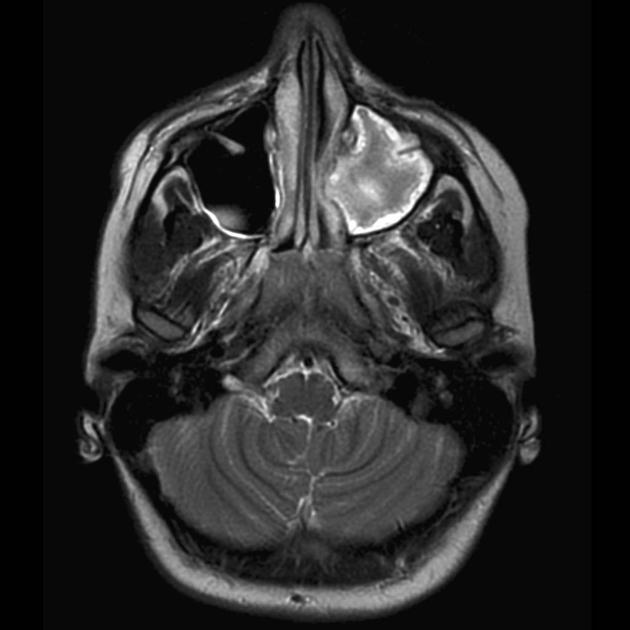
MRI
T1: intermediate to low signal
-
T2
high homogeneous T2 signal
signal may vary if they are chronic and/or if fungal infection is present
T1 C+ (Gd): peripheral enhancement is seen on post-contrast images
Treatment and prognosis
Classic treatment is intranasal snare polypectomy. However, if the base of the stalk is not excised, the polyp may recur. Ideally, minimally invasive endoscopic surgery is performed: the attachment site of the stalk is identified and excised along with a small cuff of adjacent mucosa. Visualization of the stalk base can be achieved in many cases via a medial meatotomy, or may require the creation of an additional window through the inferior meatus 6.
Recurrence rate is low (~7%) if the stalk base is excised 6.
History and etymology
They were first described by German physician Gustav Killian in 1906. Killian expressed the opinion that they arose from the maxillary sinus and gained access to the nasal cavity through the accessory ostium, based on a detailed study of 22 cases 8.
Differential diagnosis
General imaging differential considerations include:
acute sinusitis with edematous mucosa prolapsing from maxillary antrum 2








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.