Closed loop obstructions are a specific type of bowel obstruction in which two points along the course of the bowel are obstructed, usually but not always the transition points are adjacent at a single location. The closed loop refers to a segment of bowel without proximal or distal outlets for decompression.
On this page:
Terminology
Bowel obstructions which are not closed loop are called non-closed loop, open loop or simple obstructions 7,11.
Clinical presentation
Patients present with signs and symptoms of bowel obstruction, including crampy abdominal pain, vomiting, abdominal distension, and high-pitched or absent bowel sounds.
Complications
Closed loop obstructions are at higher risk than non-closed loop obstructions for strangulation (compromised blood supply) or distension-related ischemia, resulting in intestinal necrosis and perforation.
Pathology
Etiology
Closed-loop small bowel obstruction occurs when the bowel is obstructed at two points, typically close to one another, entrapping enteric contents in a closed-loop segment and leading to progressive vascular compromise with a high risk of developing ischemia and infarction.
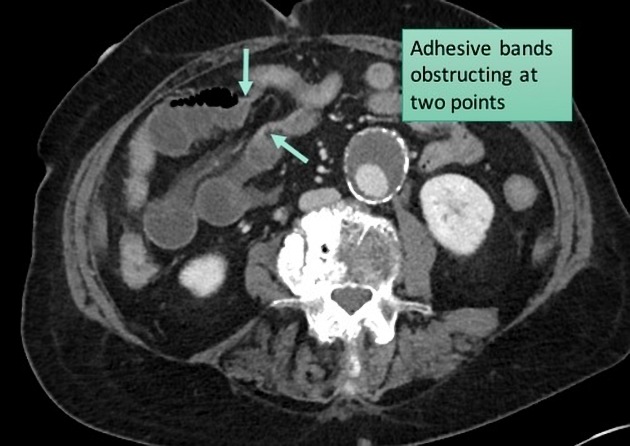
Closed loop small bowel obstructions occur secondary to adhesive bands, hernias (internal or external), or volvulus:
-
adhesive disease
most common cause of CLO
bowel becomes trapped under an adhesive band, leading to progressive dilation and rotation
most common with the antecolic roux limb technique in Roux-en-Y gastric bypass 12
-
internal hernias
second most common cause of CLO
result of surgical procedures (most commonly Roux-en-Y gastric bypass 6) or congenital defects
most common with the retrocolic roux limb technique in Roux-en-Y gastric bypass 12
-
primary small bowel volvulus
separate from the rotational changes seen in closed-loop obstruction, can likewise result in closed-loop physiology
-
a special subtype where the outflow of the pancreaticobiliary limb becomes obstructed, resulting in a closed-loop segment involving the remnant stomach
can be particularly confusing to diagnose as often the Roux/alimentary limb is not dilated and thus the patient will not improve with nasogastric tube decompression
-
large bowel volvulus (sigmoid or cecal)
additionally, large bowel obstructions occurring at a single point combined with a competent ileocecal valve, which occurs in 75% of patients, also create closed-loop pathophysiology with a risk of cecal perforation 8
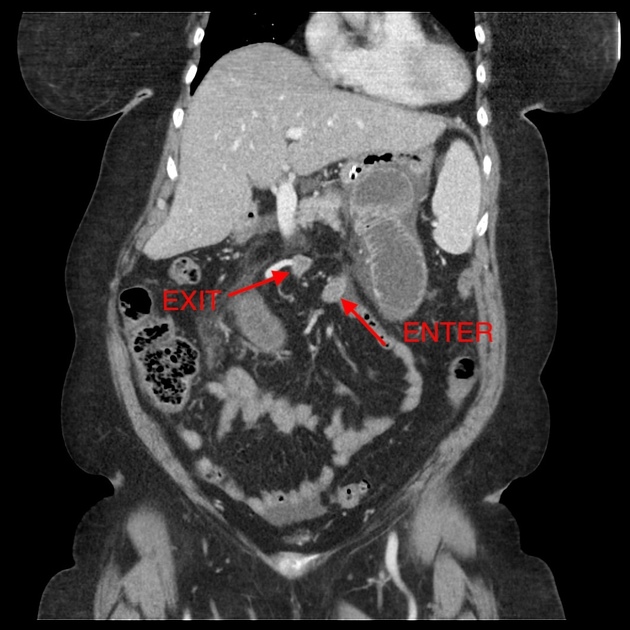
In a closed-loop obstruction, intraluminal contents are trapped, resulting in increased pressure due to ongoing fluid production. This pressure can exceed venous pressure, impairing perfusion and causing further fluid extravasation into the bowel wall and mesentery, which further exacerbates the obstruction. Vascular supply is compromised by narrowing at the entrance and exit of the closed-loop, as well as by rotation that occurs with dilation and twisting around the fixation point.
Closed-loop obstructions may also present as non-obstructive or partially obstructive conditions, where venous congestion occurs subtly without significant luminal blockage. This scenario can arise when the defect trapping the bowel is larger or less constrictive, such as in internal hernias post-gastric bypass. In these cases, bowel loops appear congested with vessels oriented toward the transition point, but without marked dilation. Patients may experience fewer acute symptoms and more intermittent discomfort.
Radiographic features
CT
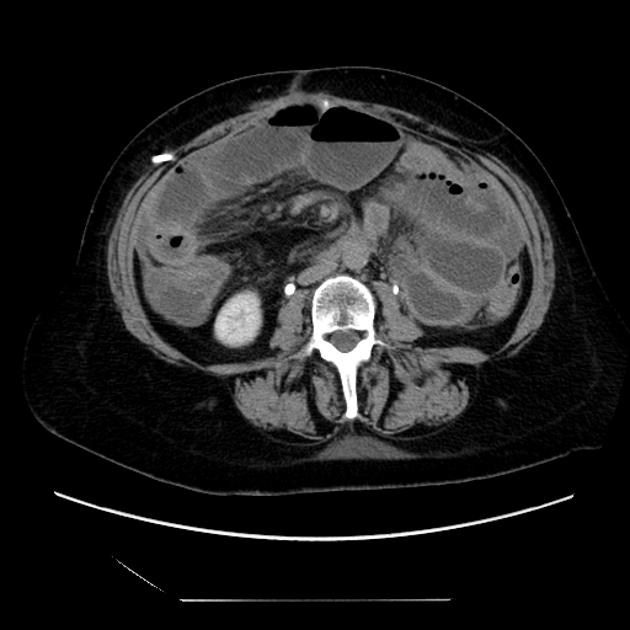
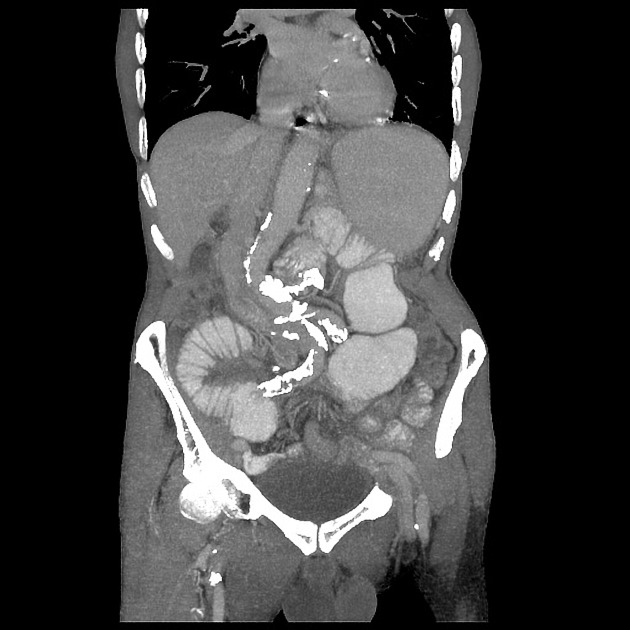
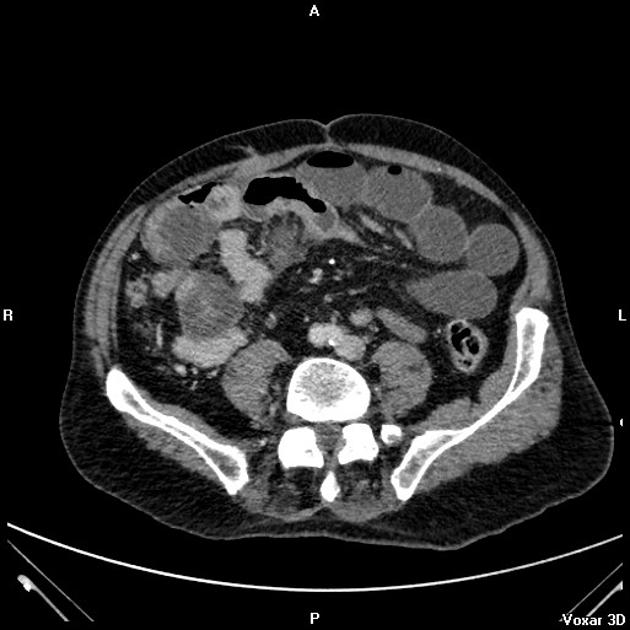
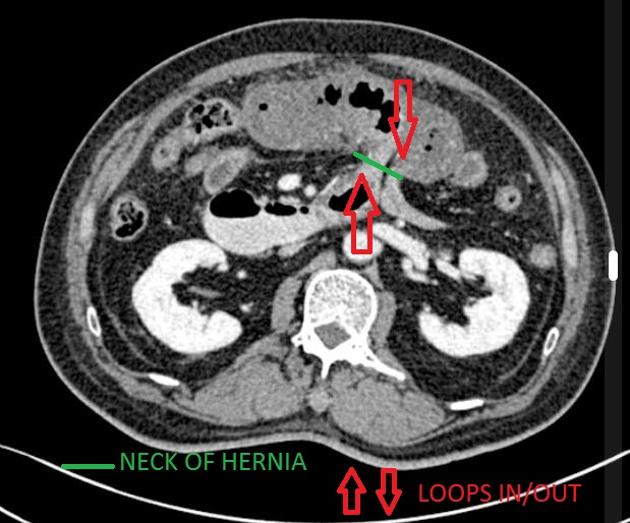
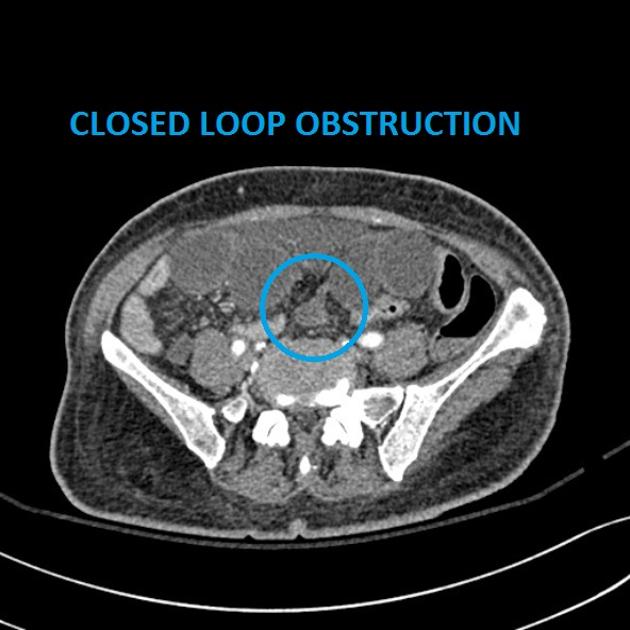
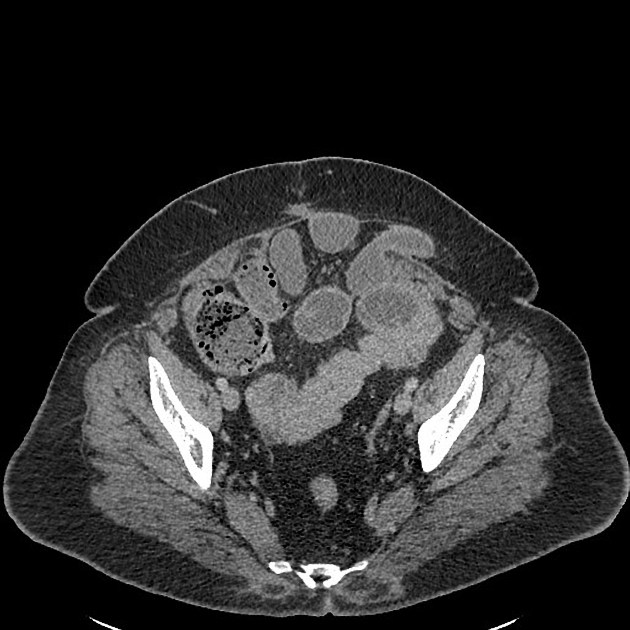
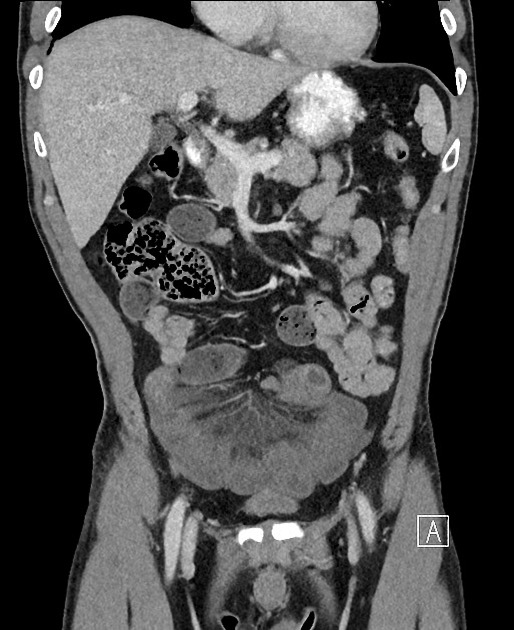
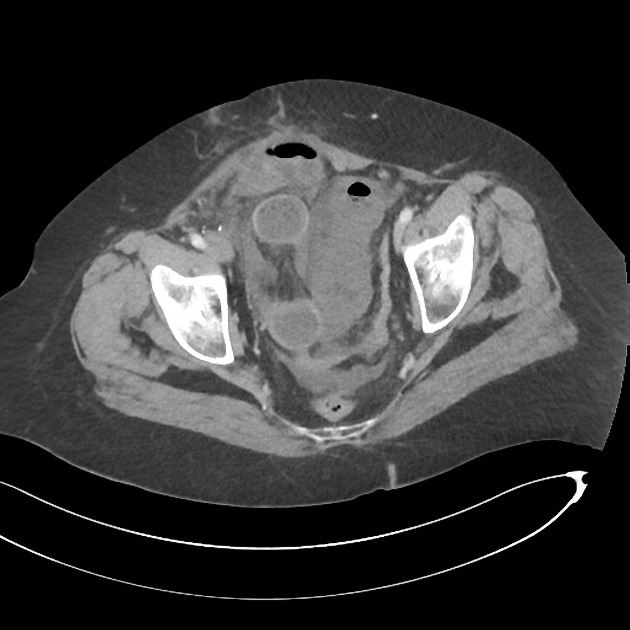
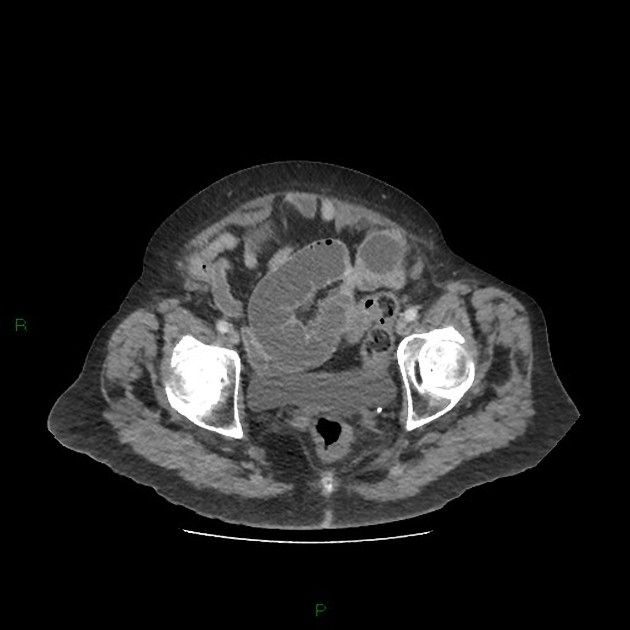
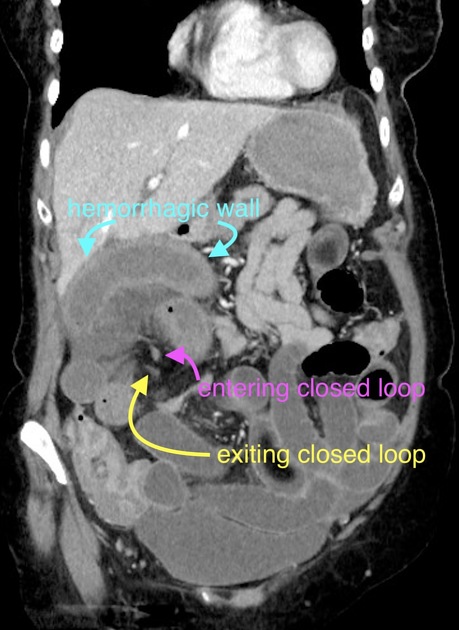
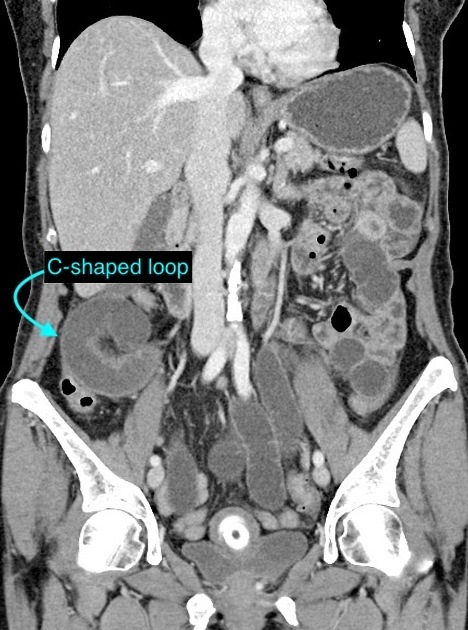
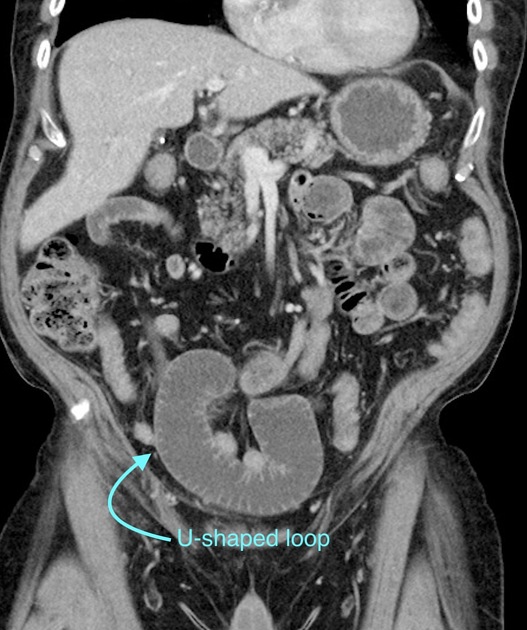
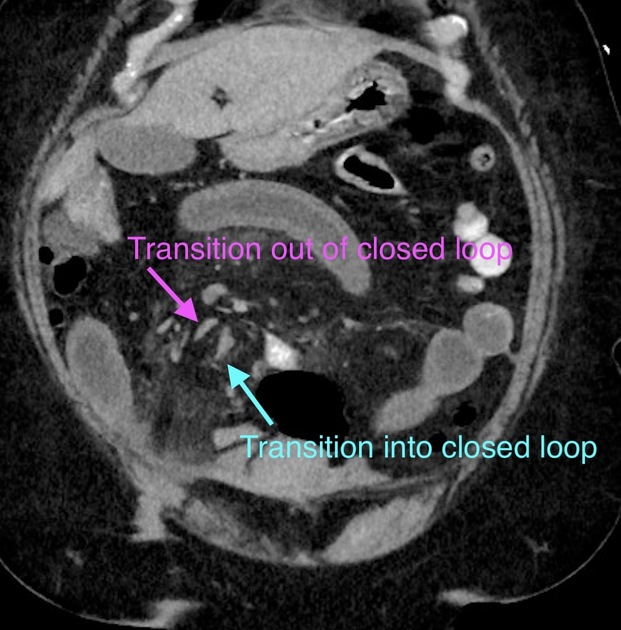
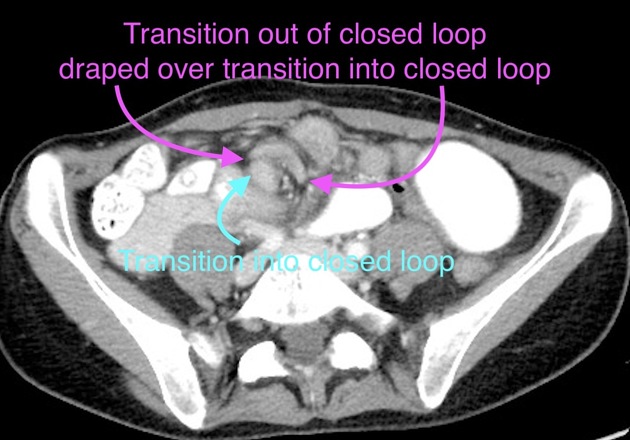
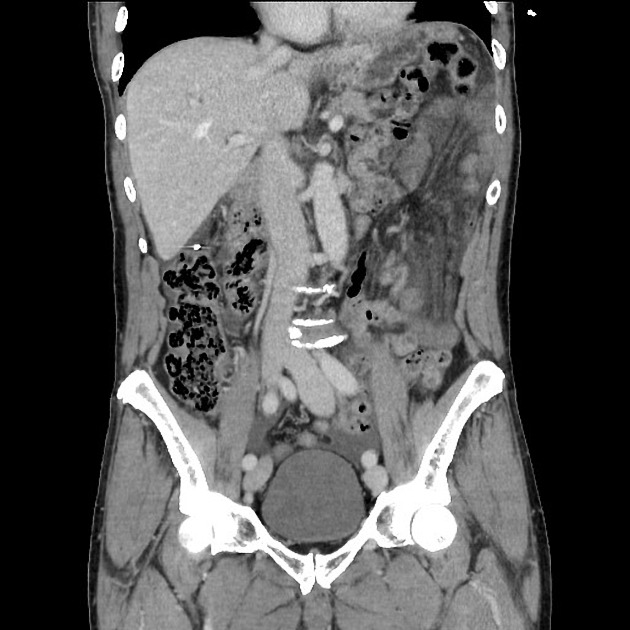
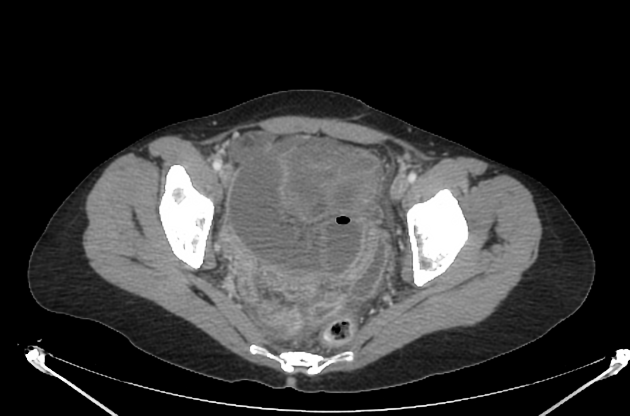
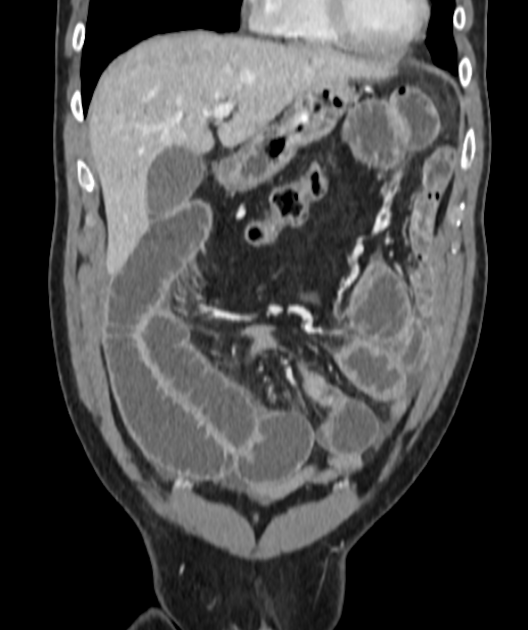
Closed-loop obstructions are diagnosed when a bowel loop of variable length is occluded at two adjacent points along its course, which may be partial or complete with characteristic features:
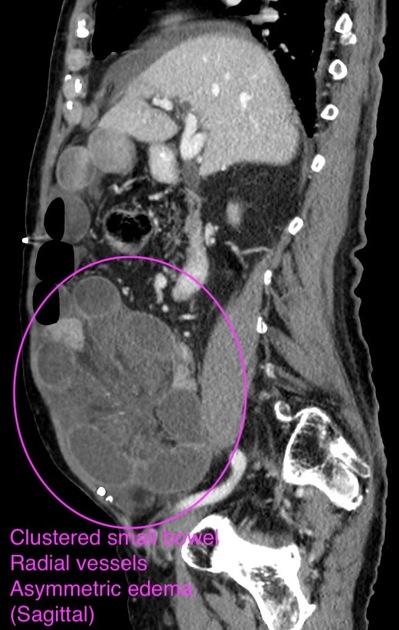
asymmetric mesenteric edema involving the closed-loop segment
stretching or sharp angulation/narrowing of the mesenteric vessels as they are distorted by the entrance/exit of the closed loop
radial distribution of several dilated, fluid-filled bowel loops
U-shaped or C-shaped configuration of the closed-loop, which often is best seen on the coronal reformats
double beak sign at the site of fusiform tapering, involving both ends of the closed loop
whirl sign reflecting rotation of bowel loops around a fixed point
intramural hemorrhage: high-density fluid within the wall of the affected small bowel is most prominent on non-contrast imaging
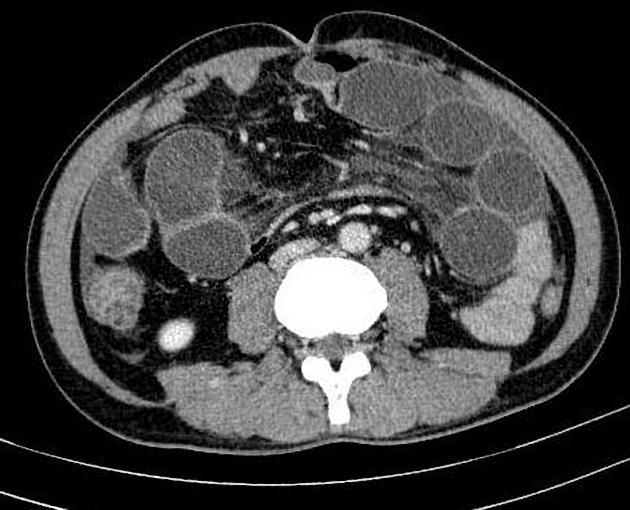
Strangulation refers to impaired blood flow (decreased perfusion) to the small bowel caused by obstruction, which can lead to bowel ischemia. Closed-loop obstructions are at particular risk for ischemia and infarction. This is mainly seen when the diagnosis is delayed (up to 10% of small bowel obstructions) and associated with high mortality 1. Features are non-specific and include 13,14:
thickened and increased attenuation of the bowel wall
increased attenuation of bowel contents due to hemorrhage
halo or target sign
pneumatosis intestinalis
portal venous gas
localized fluid or hemorrhage in the mesentery
Increased attenuation of bowel content in the closed loop (>8 HU) compared to content in the dilated proximal loop is easy to measure and, unlike bowel wall attenuation, is not affected by contrast medium administration. In a single study, sensitivity was 64% and specificity was 99% 10.
Treatment and prognosis
Risk of strangulation leads to high morbidity and mortality in closed loop bowel obstructions. Immediate surgical intervention is required especially in the setting of ischemia 6.






















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.