Gallbladder carcinoma is a type of gallbladder cancer and specifically refers to primary epithelial malignancies arising from the gallbladder, in which the vast majority (90%) are adenocarcinomas, and the remainder are squamous cell carcinomas. They are more prevalent in elderly women and, in most cases, are only symptomatic when in advanced stages.
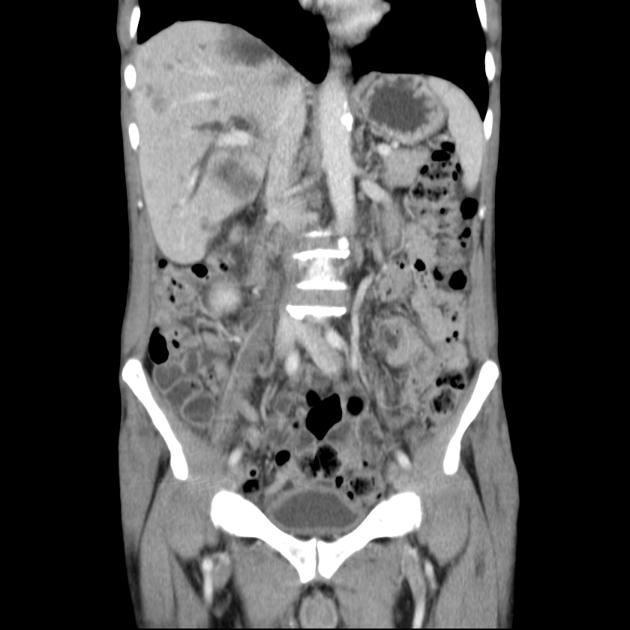
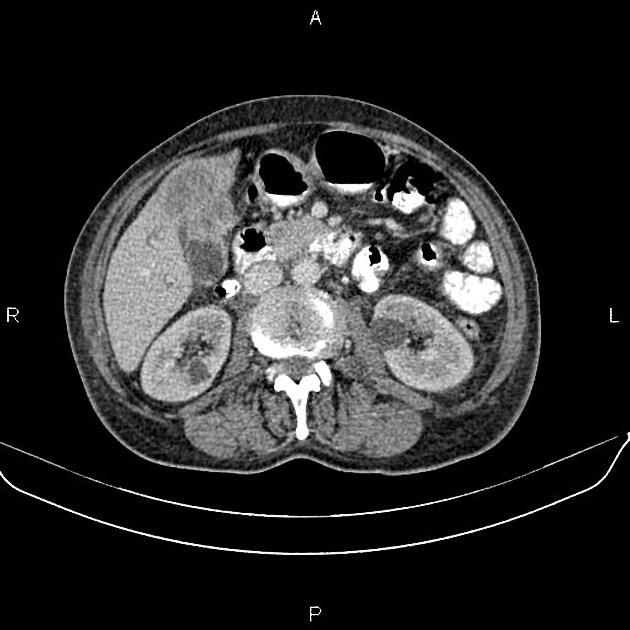
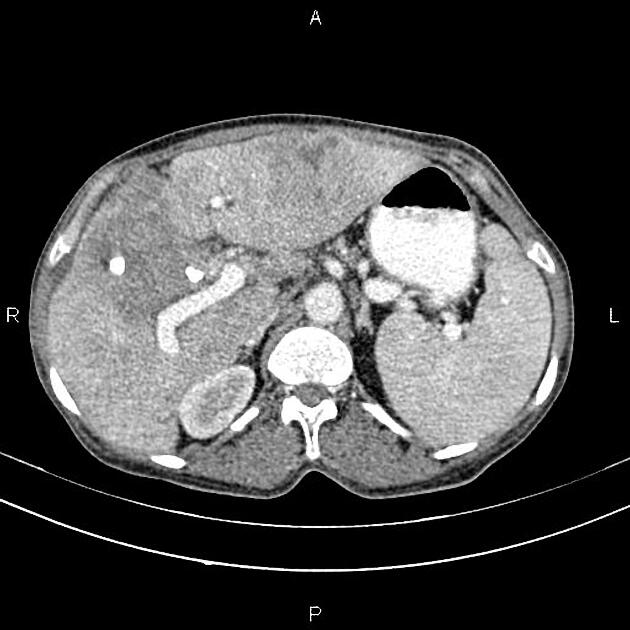
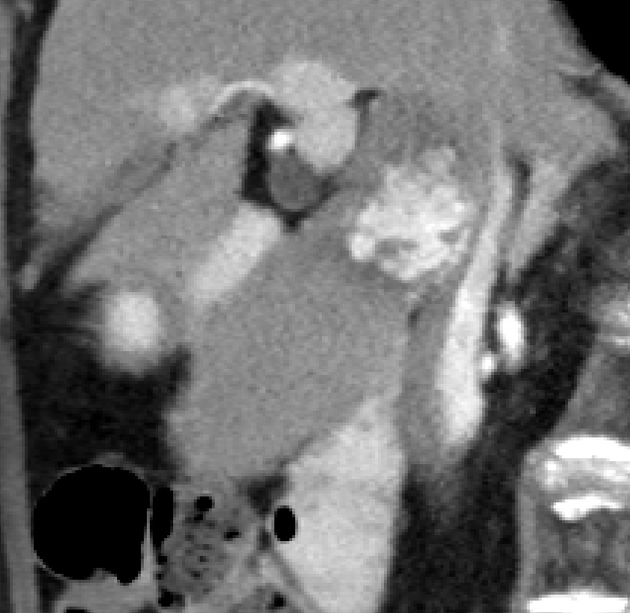
On imaging, they can present as a focal intraluminal mass, focal or diffuse gallbladder wall irregular thickening, or large mass lesion replacing the entire gallbladder. It is not uncommon to depict those tumors with some degree of invasion of adjacent structures or metastatic disease.
On this page:
Epidemiology
Although overall uncommon, gallbladder adenocarcinoma is the most common primary biliary carcinoma and the 5th most common malignancy of the gastrointestinal tract 1.
Predominantly affects older persons with long-standing cholecystolithiasis, and as such is most common in elderly women (>60 years of age, F:M ratio = 4:1) 1,3.
Risk factors
Risk factors include 1:
gallstones are seen in 70-90% of cases 3,4
-
gallbladder polyps >1 cm that are sessile and solitary
recent large-cohort data challenge polyps as a significant risk factor, and unlike colonic lesions (adenoma-carcinoma), gallbladder carcinoma likely follows a metaplasia-dysplasia-carcinoma pathway 23, 24
certain ethnicities and geographical groups (e.g. Native Americans and Chileans) 16
chronic infections including the typhoid carrier state 16
obesity, diabetes mellitus, and dietary factors 17
family history of gallbladder carcinoma 18
Clinical presentation
Early in the course of the disease, patients are invariably asymptomatic, and as such a therapeutic window is usually missed. Eventually, symptoms develop, at which time the mass is usually not resectable.
Clinical presentation depends on the direction in which the mass extends. In cases where the biliary obstruction is created then jaundice is often the first presentation. If the malignancy is located in the gallbladder's body or fundus, extending into the liver or adjacent colon or small bowel can lead to local pain or bowel obstruction, respectively.
Other symptoms include right upper quadrant pain, weight loss and anorexia.
Pathology
Over 90% of cases of gallbladder cancer are adenocarcinomas, with the majority related to chronic inflammatory metaplasia and dysplasia 15. Squamous cell carcinomas figure as the second most common histologic type of gallbladder carcinoma (representing up to 3% of all gallbladder primary malignancies) 19.
Unlike colonic lesions (adenoma-carcinoma sequence), gallbladder carcinoma likely follows a metaplasia-dysplasia-carcinoma pathway 24.
Radiographic features
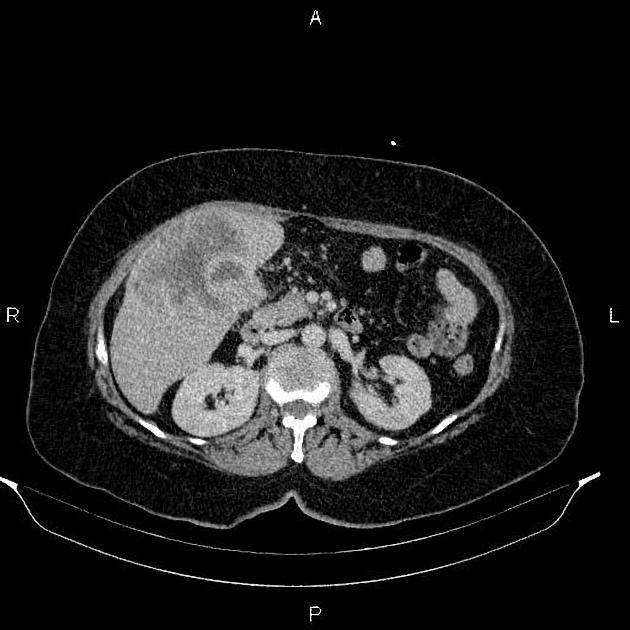
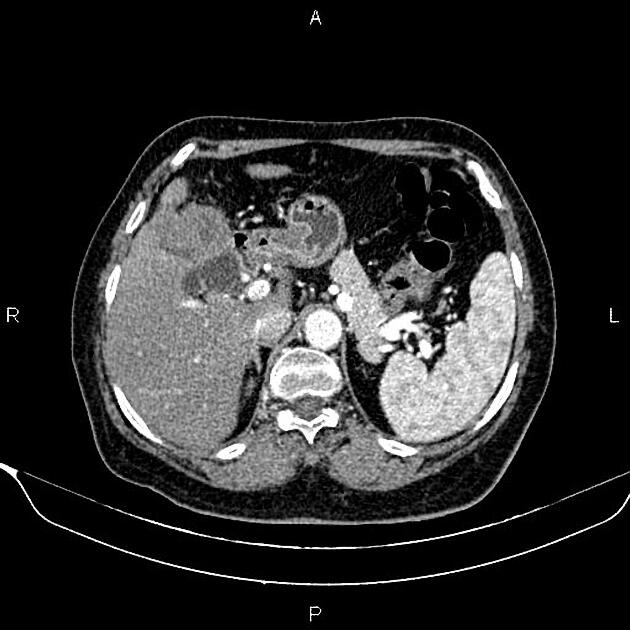
Gallbladder adenocarcinomas present in one of three morphologies 19:
intraluminal mass
diffuse mural thickening
-
mass replacing the gallbladder
presumably the end result of progression from either 1 or 2
most common presentation
Gallstones are commonly present (60%–90%) 14.
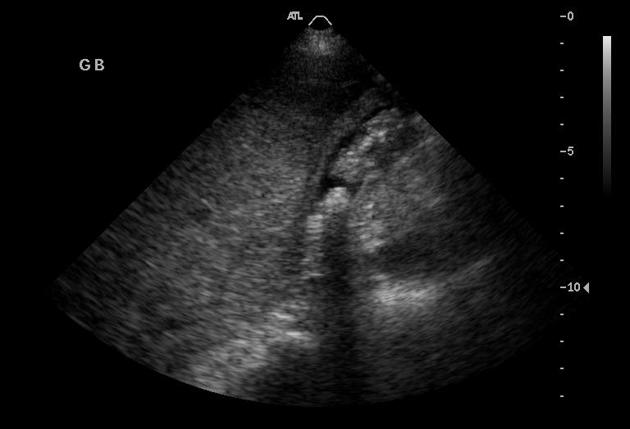
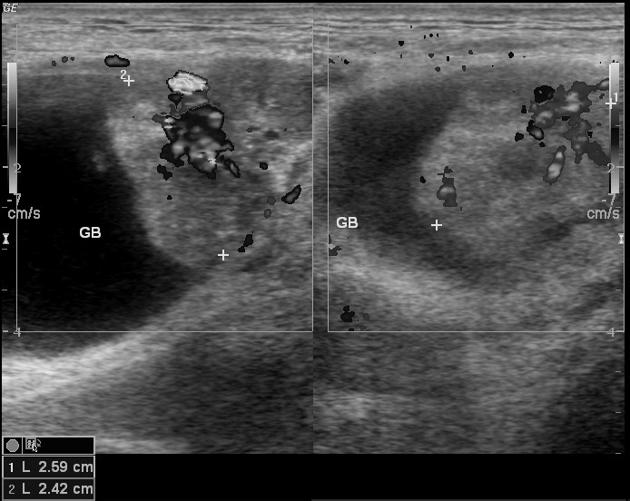
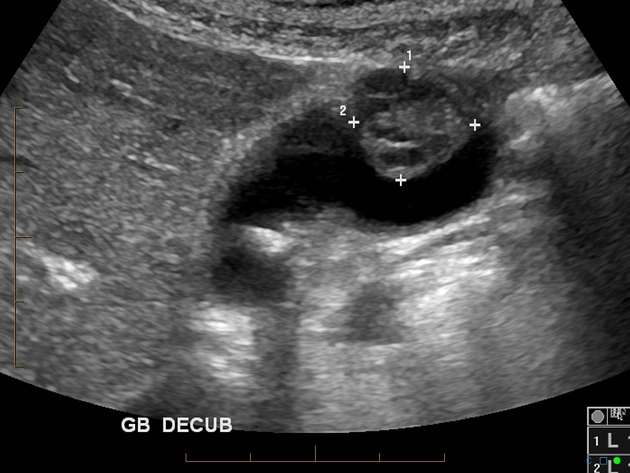
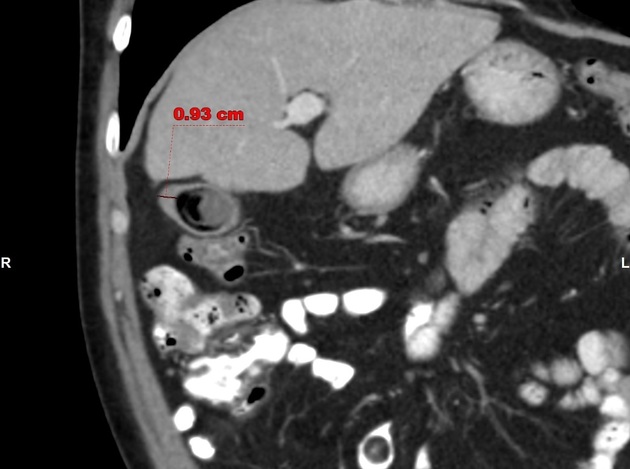
Ultrasound
Ultrasound can depict a focal intraluminal, wall involvement, or large mass-like lesion replacing the gallbladder. The tumor usually has irregular and sometimes ill-defined margins, with heterogeneous echotexture and predominantly low echogenicity. Hyperechoic foci with posterior acoustic shadowing may be seen within the mass, possibly reflecting gallstones or gallbladder wall calcifications (porcelain gallbladder) 19.
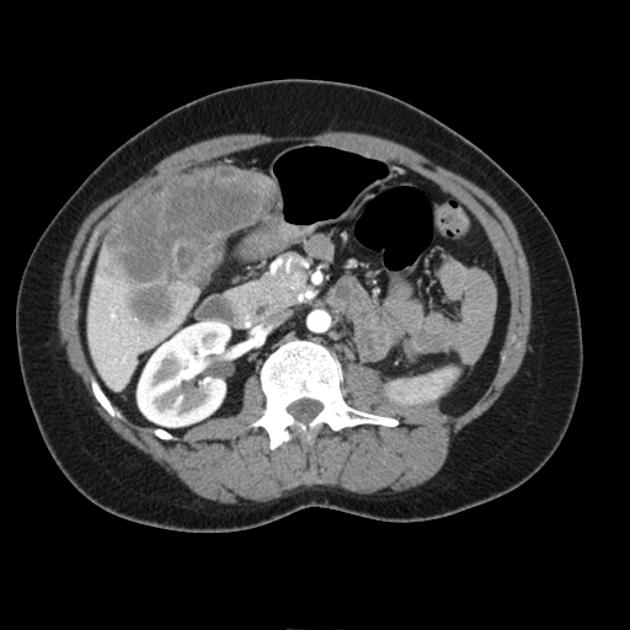
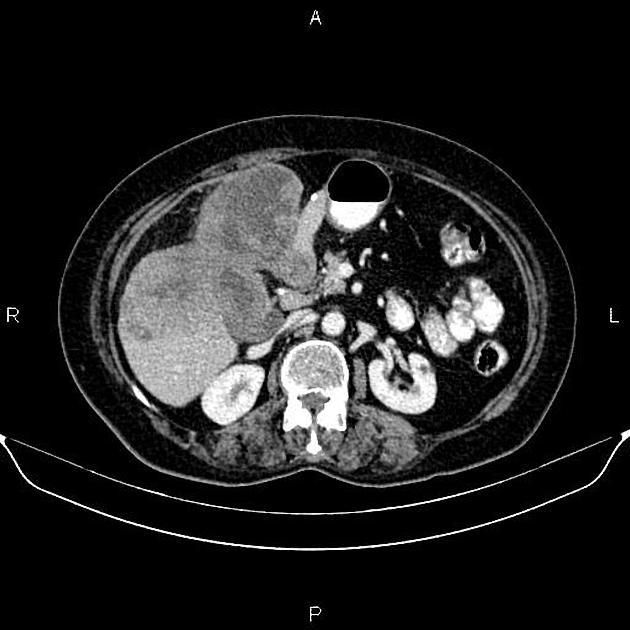
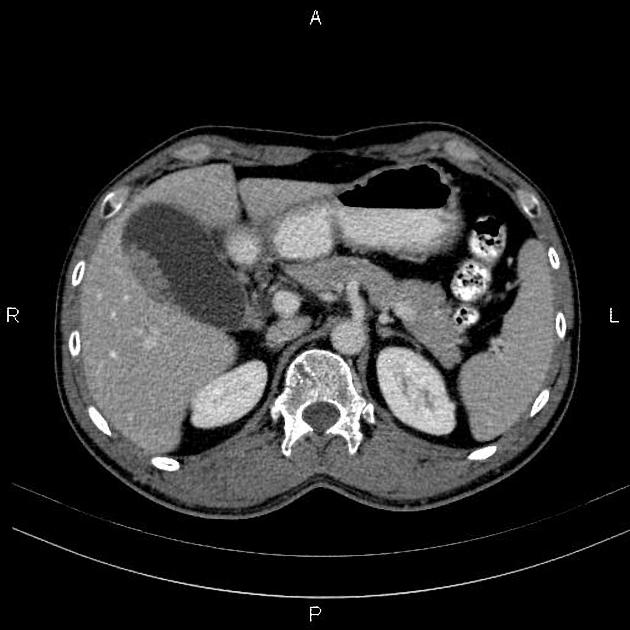
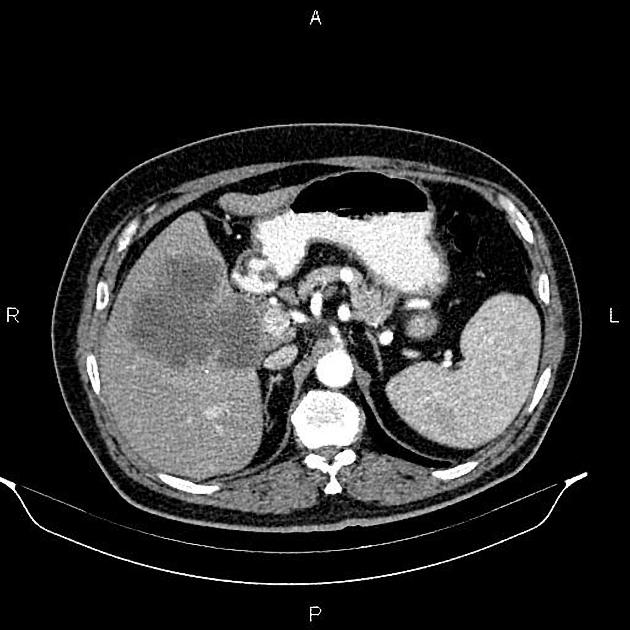
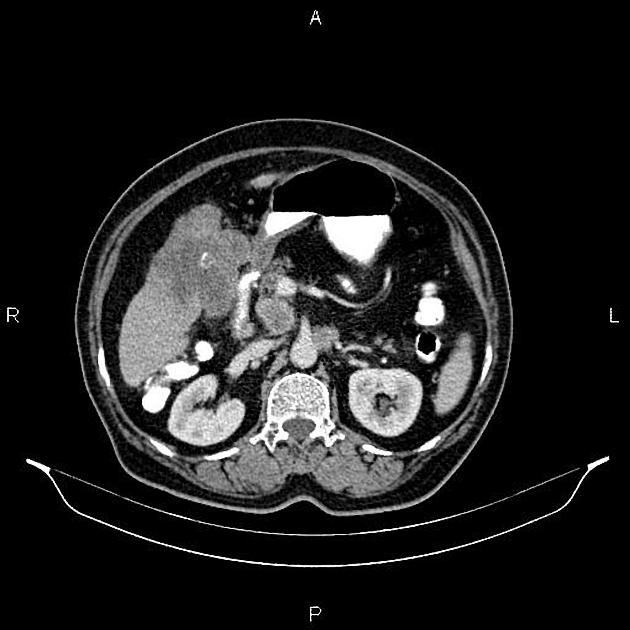
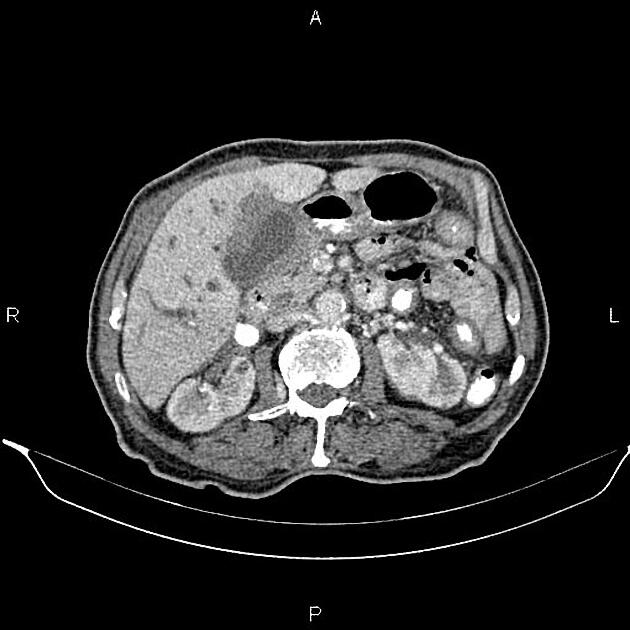
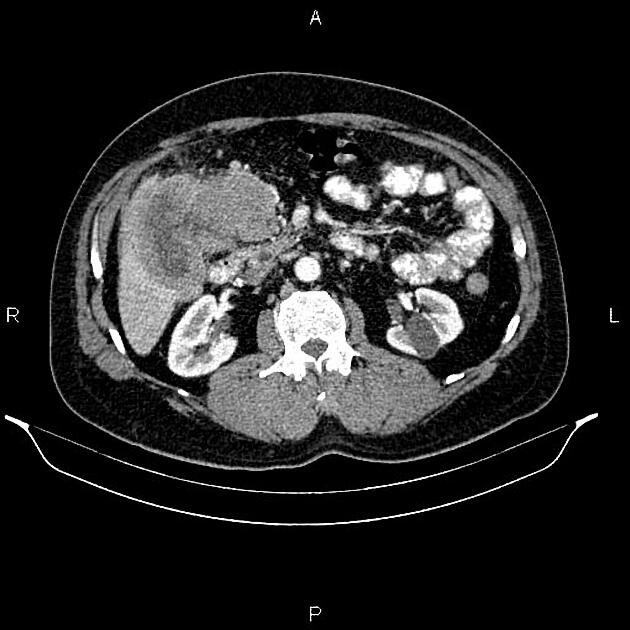
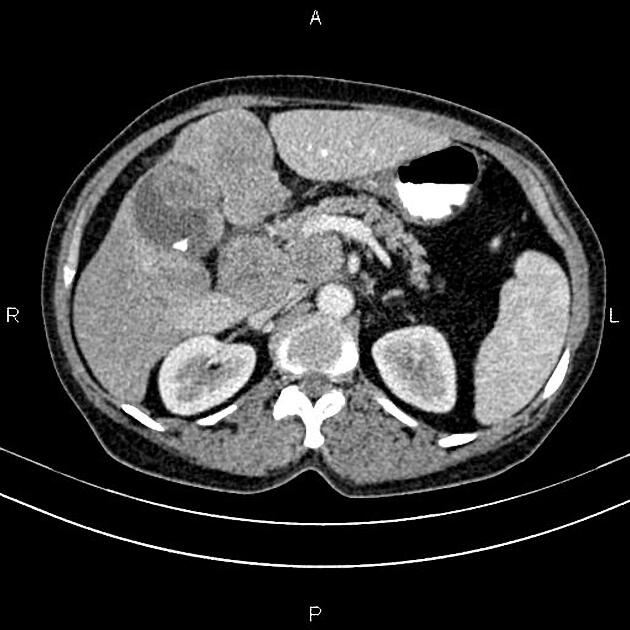
CT
In cases with strong suspicion of gallbladder cancer or biliary tract disease, arterial phase (at 20 to 30 seconds) and venous phase (50 to 60 seconds) can be acquired. When there is an incidental finding of gallbladder cancer and no suspicion of biliary tract cancer, only venous phase is required 21.
In plain CT scan, gallbladder cancer is typically hypodense. It shows irregular, peripheral enhancement on arterial phase 21.
Typically gallbladder adenocarcinomas appear as large heterogeneous masses 21, which may have engulfed gallstones or areas of necrosis. Patchy moderate contrast enhancement is usually seen.
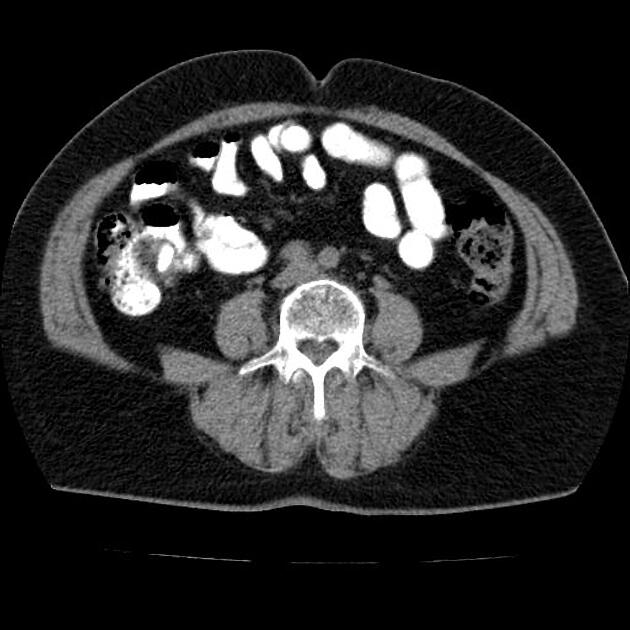
Features of advanced disease include 22:
intrahepatic biliary dilatation
invasion of adjacent structures
lymphadenopathy
hepatic and other distant metastases
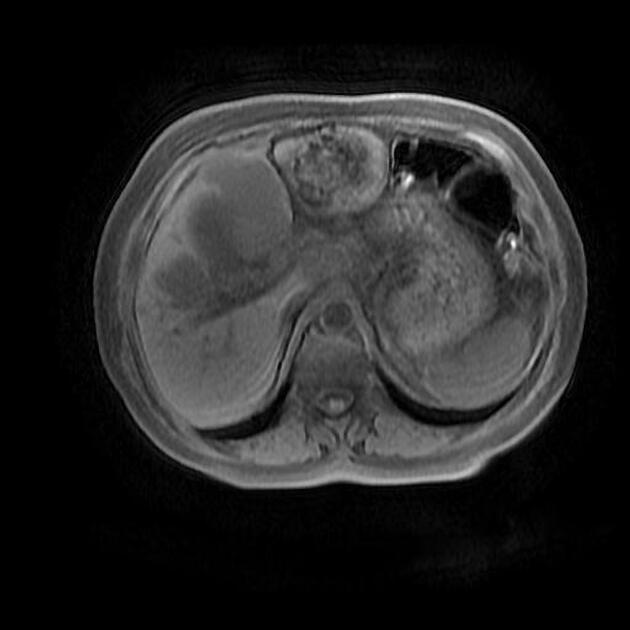
MRI
Dynamic MRI is considered useful and reliable in staging advanced gallbladder carcinoma. MRI combined with MRCP is sensitive in detecting obstructive jaundice, liver invasion, and hepatic and lymph nodal metastasis. It may be more difficult to delineate any invasion into the duodenum or to detect omental metastasis by MRI 6. Reported sensitivity rates for direct hepatic invasion and lymph node invasion on MRI can be as high as 100% and 92% respectively 7.
Staging
See article: gallbladder cancer (staging).
Treatment and prognosis
Unfortunately, due to the mostly asymptomatic nature of these tumors, the presentation is typically late with the majority of tumors being large, unresectable, with direct extension into adjacent structures or distant metastases present at diagnosis.
Curative resection is only possible for localized early disease, which is usually found incidentally. This is reflected in the dismal prognosis 4:
1-year survival: 80%
5-year survival: 1-5%
Differential diagnosis
The differential will depend on the growth pattern of the tumor
-
intraluminal masses
gallbladder polyp: see differentiating benign vs malignant gallbladder polyps
-
melanoma is the most frequent 9
other described primaries include: lung, esophagus, pancreas, colon, and kidney carcinomas 9
-
mural thickening has a limited differential but is difficult to distinguish on imaging alone, possibilities include:
gallbladder wall thickening due to portal hypertension
-
large tumors differentials include a number of nearby primaries with extension to the gallbladder
tumors from adjacent organs (pancreas, duodenum) invading gallbladder fossa 10















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.