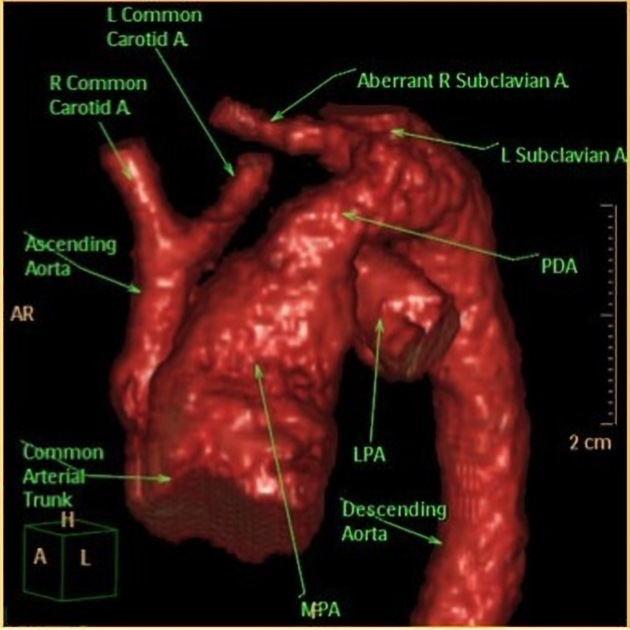
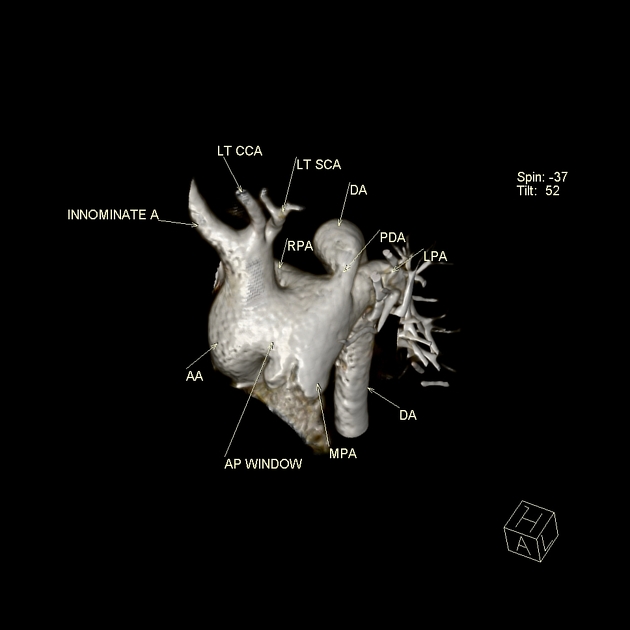
Interrupted aortic arch (IAA) is an uncommon congenital cardiovascular anomaly where there is a separation between the ascending and descending aorta. It can either be complete or connected by a remnant fibrous band. An accompanying large ventricular septal defect (VSD) and/or patent ductus arteriosus (PDA) is frequently present.
On this page:
Epidemiology
It may account for ~1.5% of congenital cardiac anomalies.
Pathology
Faulty embryological development of the aortic arch (thought to occur during the 5th to 7th week of intrauterine life).
Classification
According to the Celoria-Patton classification, IAA can be classified into three types according to the location of the anomaly:
type A: second most common, the interruption occurs distal to the left subclavian arterial origin
type B: most common (>50%), the break occurs between the left common carotid and left subclavian arterial origins
type C: rare, interruption occurs proximal to the left common carotid arterial origin
Each type is divided into three subtypes 7:
subtype 1: normal subclavian artery
subtype 2: aberrant subclavian artery
subtype 3: isolated subclavian artery that arises from the ductus arteriosus
Associations
-
found commonly in those with a type B interruption
almost always associated if there is a right-sided descending aorta
Radiographic features
Plain radiograph
Plain film features are often non-specific 3:
the aortic knuckle may be absent
may show cardiomegaly
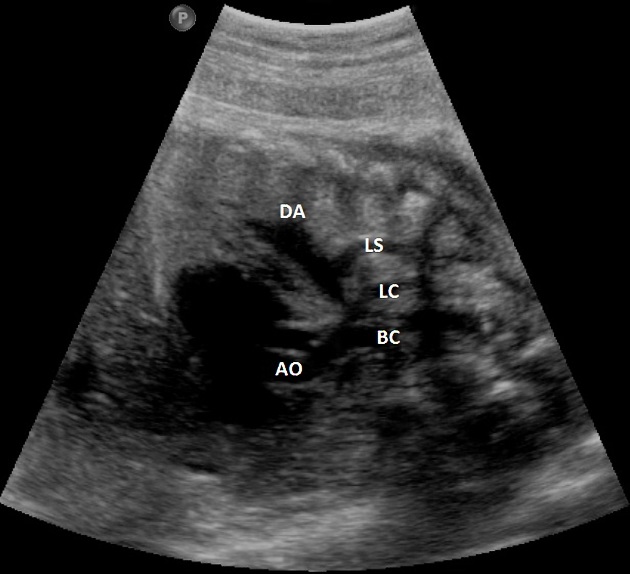
Ultrasound
The right ventricle may appear a lot larger than the left, although this is a non-specific finding. The ascending aorta may also appear more vertical than usual. These modalities may not allow differentiation of IAA from severe aortic coarctation with a hypoplastic arch 9.
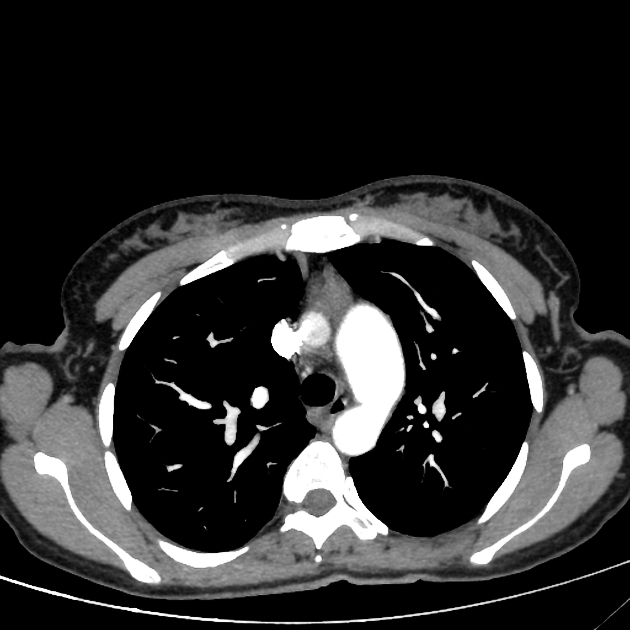
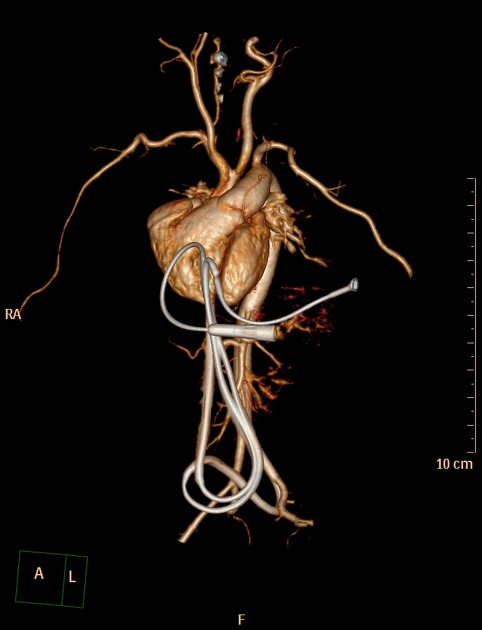
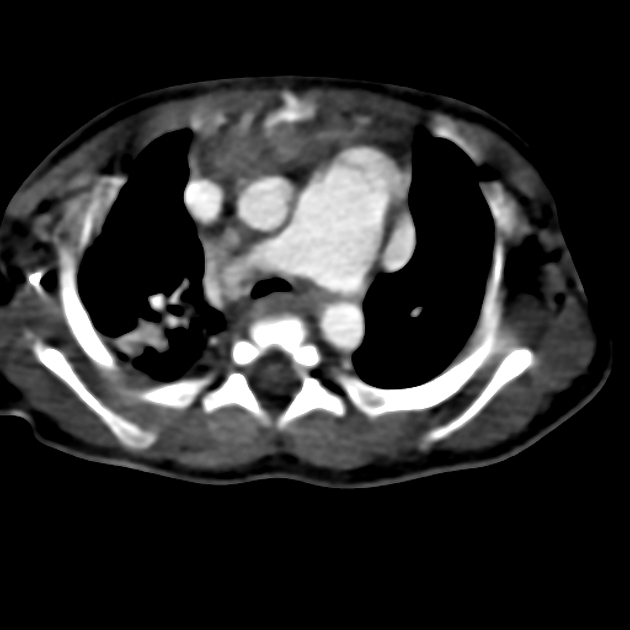
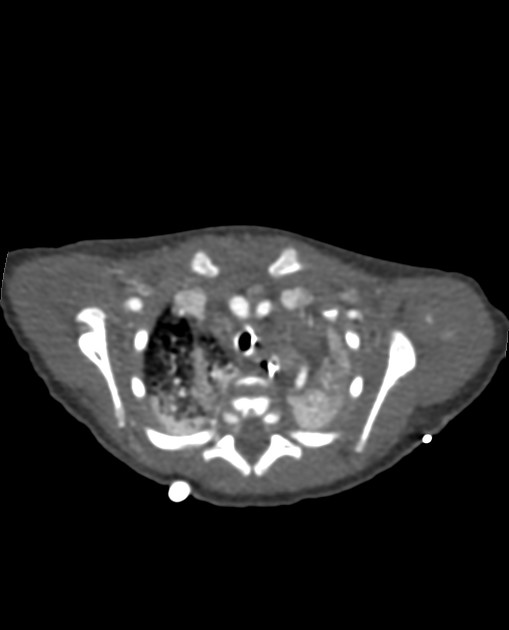
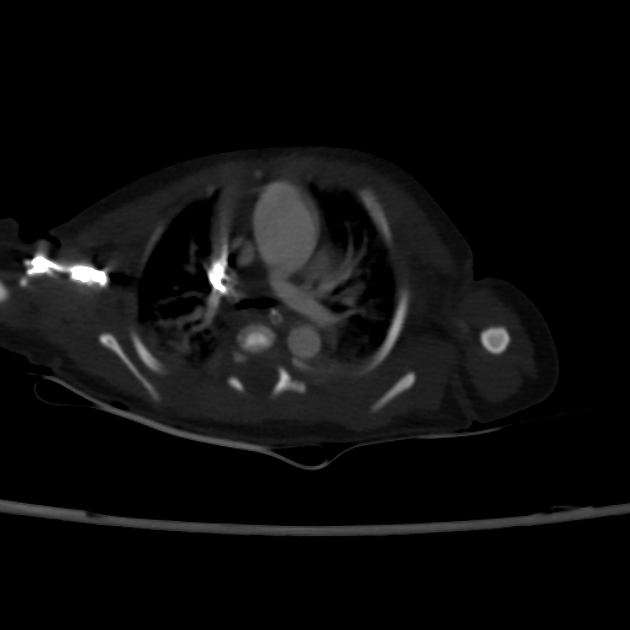
CT
Allows visualization of the interrupted aortic arch and associated anomalies.
MRI
non-visualization of the portion of interruption
great vessels may show a "V" configuration on coronal imaging 2
Treatment and prognosis
If uncorrected, it carries a very poor prognosis with extrauterine survival being as little as a few days. Prostaglandin E1 may be given to initial management to keep the ductus open. Surgical correction (either single- or multistage) is the definitive treatment.
Differential diagnosis
General differential considerations include:
short segment severe aortic coarctation







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.