Juxtacortical chondromas, also known as periosteal chondromas, are rare benign chondral tumors that arise from the periosteum of tubular bones. They are thought to account for ~2% of benign bone tumors.
On this page:
Epidemiology
They tend to present around the 2nd to 4th decades. There is a recognized male predilection 1.
Location
Typical sites include 3:
proximal humerus and distal femur (70%)
phalanges (25%)
tibia
radius
ulna
Radiographic features
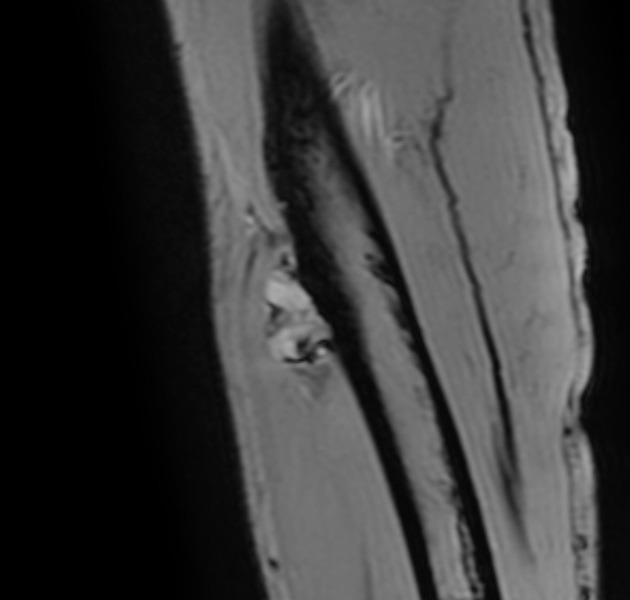
Plain radiograph
may be seen as a saucerisation of the adjacent bony cortex with a sclerotic periosteal reaction
distinct soft tissue mass may be difficult to identify
matrix calcification may be seen in ~50% of cases; as with all chondroid lesions, this tends to be rings and arcs
most lesions are <3 cm in size 1
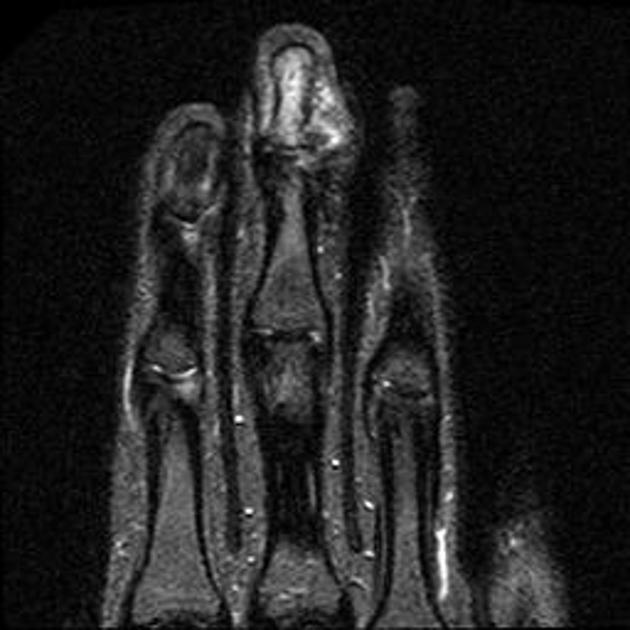
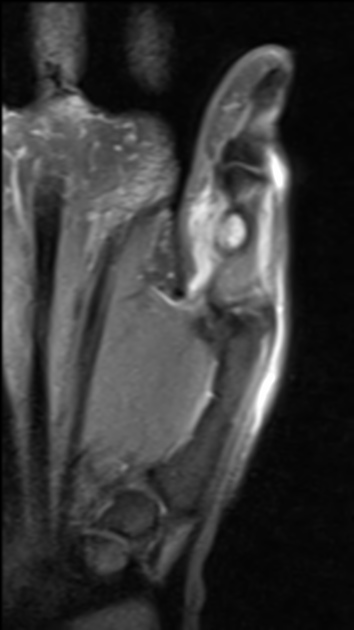
MRI
Typically seen as a soft tissue lesion abutting the cortex and may better demonstrate evidence of pressure erosion of neighboring bone. Often has a lobulated configuration. Tends to lack associated medullary bone or soft tissue edema.
Signal characteristics include 8:
T1: typically iso to low signal relative to muscle
T2/T2*: high signal but with low signal areas representing calcification
T1 C+ (Gd): heterogeneous and tends to show peripheral predominant contrast enhancement
Treatment and prognosis
They are benign lesions, however, may be similar in imaging and histopathologic appearance to juxtacortical chondrosarcomas. Local excision is often the treatment of choice. Once resected lesions usually do not recur.
Differential diagnosis
Imaging differential considerations include:
periosteal osteosarcoma: lobulated margins and high T2 chondral nodules of periosteal chondroma are absent
non-epiphyseal chondroblastoma: typically associated with reactive marrow edema on MR
juxtacortical chondrosarcoma: often larger than 3 cm (mean size 5.5 cm)
bizarre parosteal osteochondromatous proliferation (Nora lesion): for phalangeal lesions
cortical desmoid: for the posteromedial distal femoral lesions
tenosynovial giant cell tumor: for phalangeal lesions





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.