Periosteal osteosarcomas are intermediate-grade bone-forming neoplasms originating on the bony surface in strong association, typically underneath the periosteum.
On this page:
Epidemiology
Periosteal osteosarcomas are the second most common type of surface-based osteosarcoma after parosteal osteosarcoma and account for 1-2% of all osteosarcomas 1-4. Periosteal osteosarcomas are seen in a wide age range from the first to the seventh decade with a peak in the second decade of life 1.
Diagnosis
The diagnosis of periosteal osteosarcomas is based on a combination of typical radiographic features and histology.
Diagnostic criteria
Diagnostic criteria according to the WHO classification of soft tissue and bone tumors (5th edition) 1:
imaging features of a bone tumor
histology of an intermediate-grade mostly chondroblastic osteosarcoma
origin from the surface of the bone under the periosteum
typically involves the diaphysis of long tubular bones
Clinical presentation
Typical symptoms include swelling and/or pain lasting for weeks to months 1.
Pathology
Periosteal osteosarcomas are predominanty chondroblastic osteosarcomas with a chondroid matrix. They typically arise from the inner cambium layer of the periosteum 4 and are attached to the underlying cortex 1. The cytologic grade is intermediate which is higher than parosteal osteosarcoma and lower than conventional osteosarcomas 1.
Etiology
The etiology of periosteal osteosarcomas is unknown.
Location
Periosteal osteosarcomas tend to be diaphyseal and are found in the following locations 1-5:
the femur and tibia are the most common sites
occasionally in other long bones and/or flat bones
rarely in the hand and feet or the craniofacial bones
Macroscopic appearance
Grossly tumors are characterized by the following features 1,5:
ovoid broad-based lobulated pale cartilaginous appearance
attachment to the osseous cortex in continuity with the inner periosteum
possible reactive bony spiculae
commonly delineated capsule
Microscopic appearance
Microscopically, periosteal osteosarcomas are characterized by cartilaginous areas with a transition to an osteoid matrix with the following histological features 1,5:
lobules of atypical cartilage
intervening bands of reactive bone
periosteal reaction with linear reactive bone spicules separated by cartilaginous matrix
primitive undifferentiated mesenchymal cells at the tumor perimeter with mitoses and nuclear atypia
Immunophenotype
On immunohistochemistry stains periosteal osteosarcomas express SATB2 which is not particularly helpful in the differentiation from periosteal chondrosarcoma 1.
Radiographic features
Typical imaging characteristics include 3,4,6:
broad-based cortically attached tumor with a partially mineralized soft tissue mass
extrinsic erosion of thickened underlying diaphyseal cortex with a surface-base crater
perpendicular or spiculated periosteal reaction
usually involves ~50% of the cortical circumference
intramedullary extension is rare
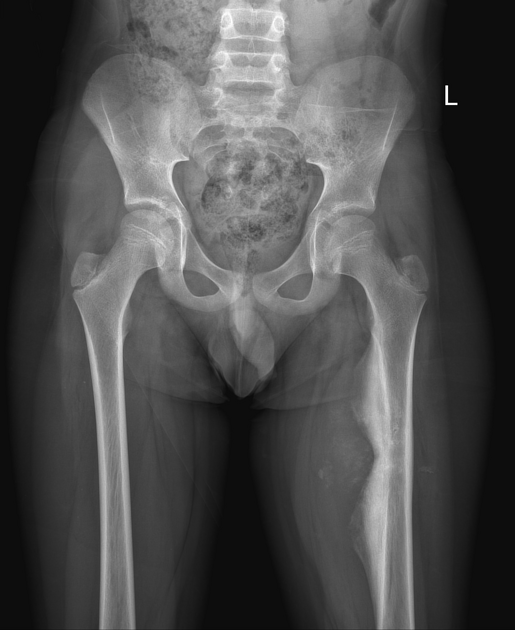
Plain radiograph
lucent fusiform mass attached to the bony surface
variable mineralization
cortical thickening with ectosteal scalloping or “saucerization” 6
solid, lamellated or spiculated periosteal reaction and occasionally Codman triangle 1
CT
Periosteal osteosarcomas feature a chondroid matrix that is characterized by a low attenuation on CT images 1,4,6.
MRI
As on the other imaging modalities on MRI periosteal osteosarcomas appear as cortical-based tumors with strands of ossification within the lesion perpendicular radiating from the surface and more pronounced towards the cortex 1,3,4. They usually surround about half of the affected bone 3. Compared to muscle lesions are usually hyperintense in T2 and intermediated-weighted images 6 with areas of low-signal intensity due to matrix mineralization. They might have reactive abnormal intramedullary signal changes, even though true bone marrow infiltration is rare 1,4.
Signal characteristics
T1: intermediate to high signal
T2: intermediate to high signal
STIR/IMFS: heterogeneously high signal
T1 C+ (Gd): enhancement
Radiology report
The radiological report should include a description of the following 4:
form, location and size
tumor margins and transition zone
circumferential extent
periosteal reaction
cortical erosion, cortical breakthrough
medullary involvement (less likely)
infiltration of neurovascular structures (if present)
Treatment and prognosis
Periosteal osteosarcoma is of intermediate grade with the prognosis being better than conventional osteosarcoma, but not as good as parosteal osteosarcoma (which is usually low grade) with 5-year and 10-year survival rates of 89 and 77-86% 1,8. Bone marrow invovement is rare but if present is associated with less favorable outcome 1. Treatment usually consists in wide excision. Chemotherapy does not seem to influence prognosis or survival and has been associated with the occurance of secondary malignancies in occasional cases 9. Local recurrences, metatsases and death usually occur within a period of 3 years after the diagnosis 1,8.
History and etymology
Periosteal osteosarcomas were first recognized by the American pathologist James Stephen Ewing in 1939 and again described later by the American pathologist Louis Lichtenstein 9,10 .
Differential diagnosis
Differential diagnoses that look similar to periosteal osteosarcoma on imaging studies include the following entities 4:
conventional osteosarcoma: intramedullary extension
periosteal chondrosarcoma: affects older individuals





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.