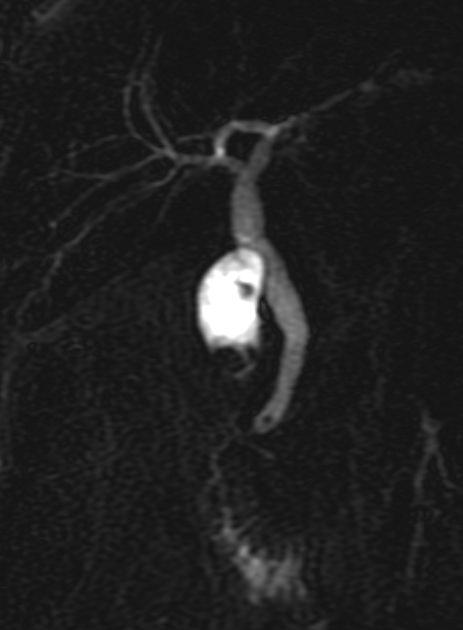
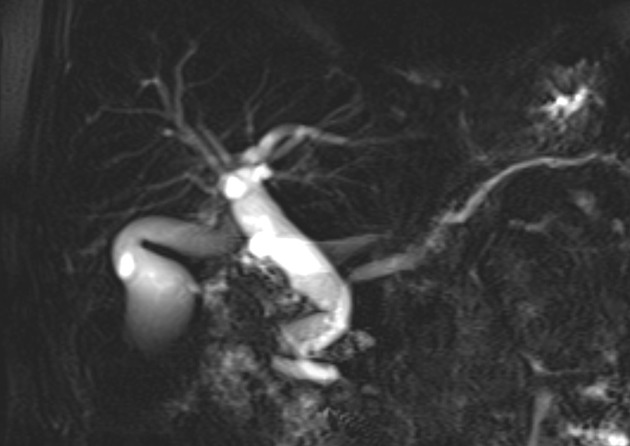
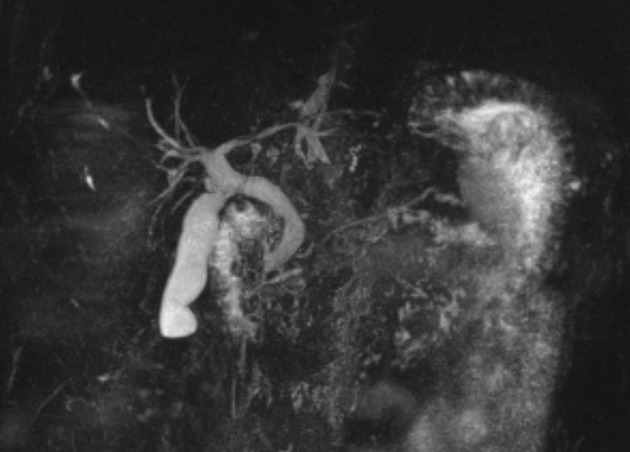
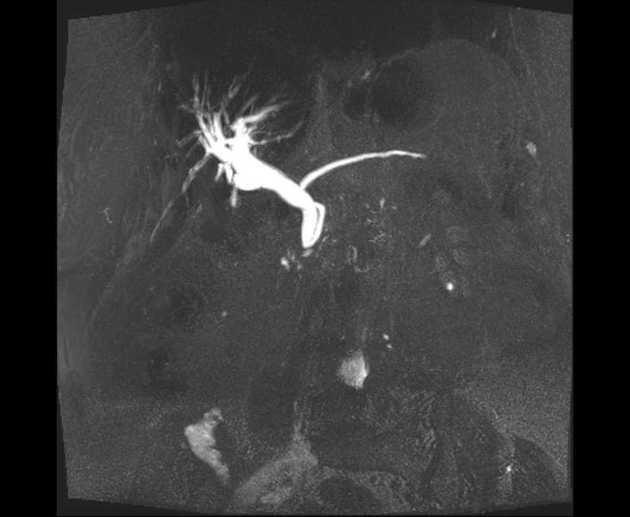
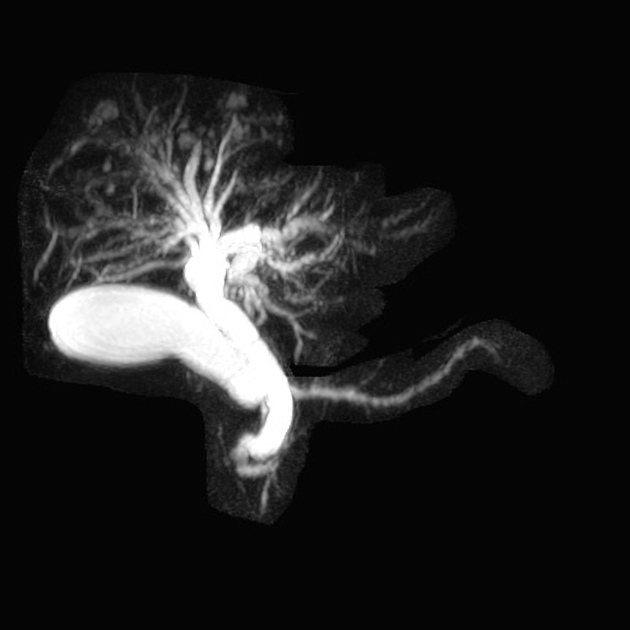
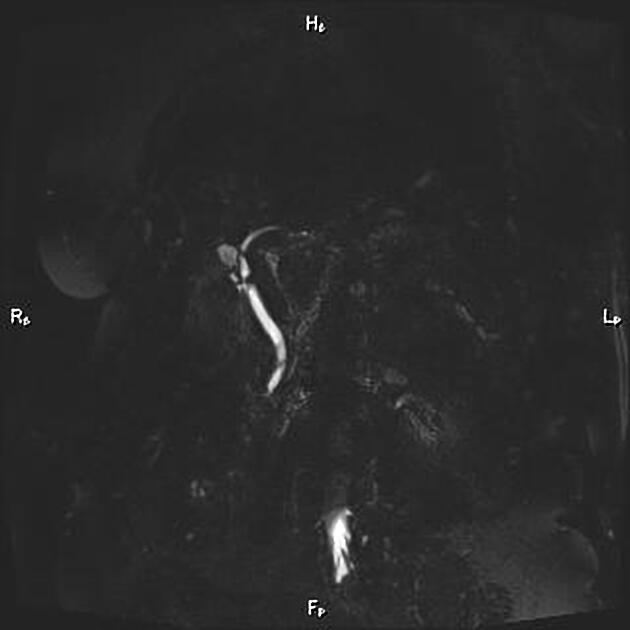
Magnetic resonance cholangiopancreatography (MRCP) is a non-invasive imaging technique to visualize the intra and extrahepatic biliary tree and pancreatic ductal system.
It can provide diagnostically-equivalent images to ERCP and is a useful technique in high risk patients to avoid significant morbidity.
On this page:
Indications
MRCP can be used to evaluate various conditions of the pancreaticobiliary ductal system, some of which are:
identification of congenital anomalies of the cystic and hepatic ducts
post-surgical biliary anatomy and complications 9
biliary or pancreatic trauma
Physics
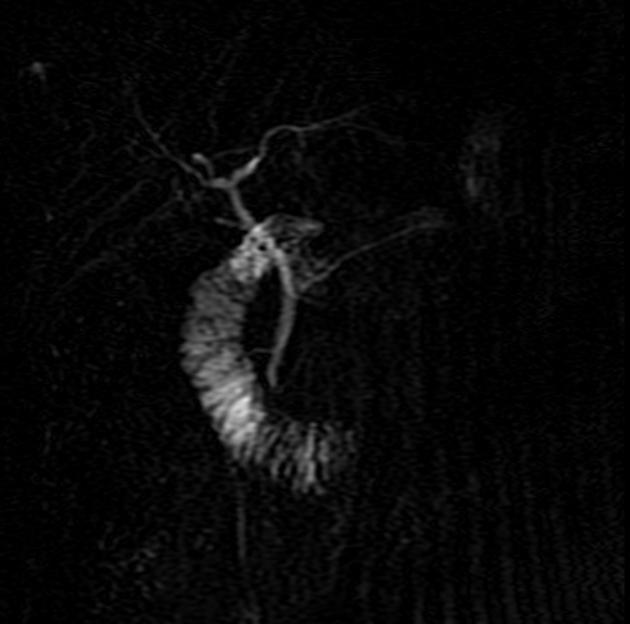
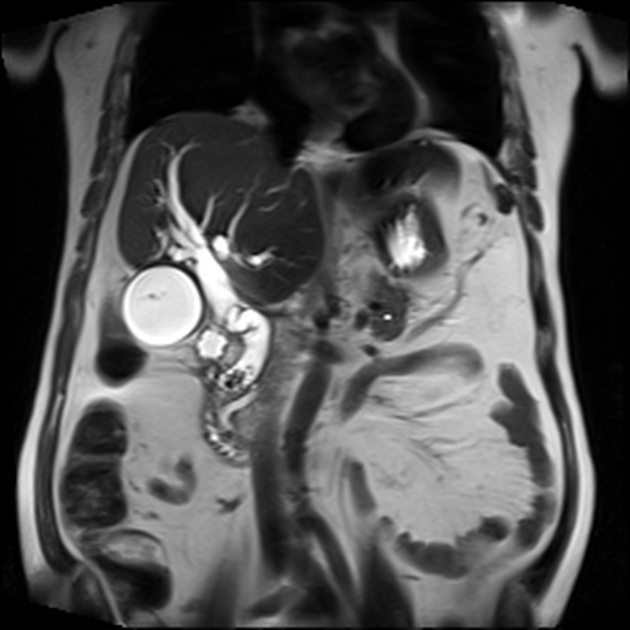
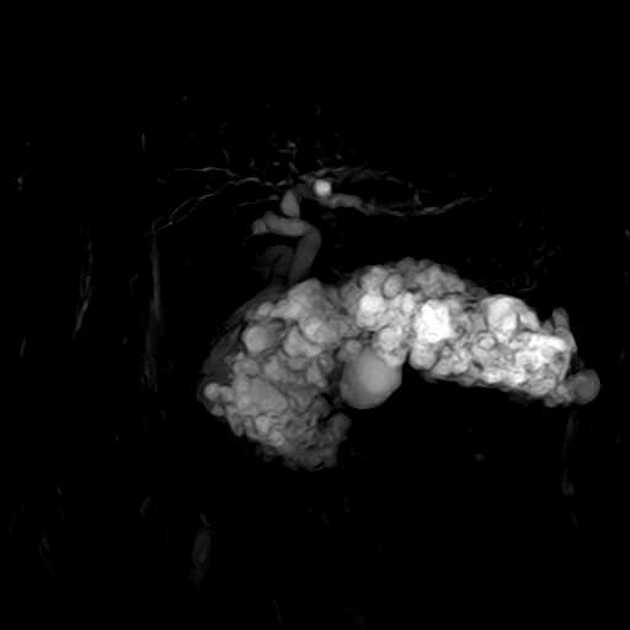
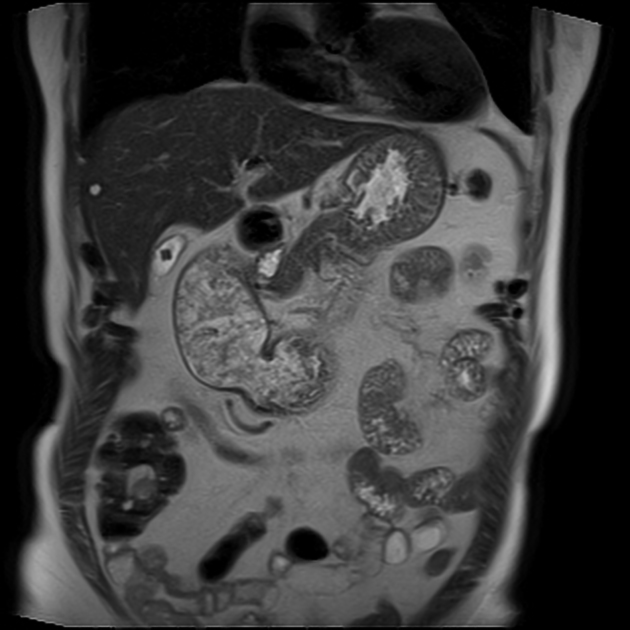
The technique exploits the fluid which is present in the biliary and pancreatic ducts as an intrinsic contrast medium by acquiring the images using heavily T2-weighted sequences. Since the fluid-filled structures in the abdomen have a long T2 relaxation time as compared to the surrounding soft tissue, these structures appear hyperintense against the surrounding non-fluid-containing tissues on a heavily T2-weighted sequence and can easily be distinguished.
Technique and protocols
No exogenous contrast medium is administered to the patient.
Fasting for 4 hours prior to the examination is required to reduce gastroduodenal secretions, reduce bowel peristalsis (and related motion artifact) and to promote distension of the gallbladder. Insufficient fasting may lead to the appearance of a shrunken gallbladder (see: Case 20). MRCP is performed on a 1.5 T or higher field system, using a phased-array body coil.
All protocols obtain heavily T2-weighted sequences. Most commonly obtained sequences are:
RARE: rapid acquisition and relaxation enhancement
FRFSE: fast-recovery fast spin-echo coronal oblique 3D respiratory triggered
HASTE: half-Fourier acquisition single shot turbo spin echo-axial 2D breath hold sequence which provides superior images and can be performed in single breath hold (<20 s) and a fat-suppressed sequence
-
an additional sequence that can be acquired to evaluate the duct wall is a fat suppressed T1 GRE sequence
T1 sequences may also help differentiate biliary calculi from pneumobilia 7
For optimal visualization of ducts, acquired images are reformatted in different planes using multiplanar reconstruction (MPR) and maximum intensity projection (MIP).
The advantage of FRFSE, as a 3D technique, is the ability to perform multiplanar reconstructions. However, despite respiratory triggering, this sequence is often prone to motion artifact.
Technical modifications
With the evolution of MRCP, modified techniques came into existence. Commonly applied modified MRCP techniques are:
-
secretin-stimulated MRCP
-
secretin (administered intravenously) causes exocrine secretion of the pancreas, dilating the pancreatic duct and improving its visualization; indications include 1:
detection/characterization of pancreatic duct anomalies or strictures
characterizing communications between the pancreatic duct and pseudocysts/fistulas
characterizing pancreatic and sphincter of Oddi dysfunction
-
-
functional MRCP
intravenous administration of MR lipophilic paramagnetic contrast agents which are then excreted by the hepatobiliary system
-
negative oral contrast to 'null' the duodenum
commercially available agents
natural products which are rich in manganese (e.g. pineapple or blueberry juice) shorten the T2 relaxation time 8
Practical points
Artifacts related to technique and reconstruction, and motion or susceptibility artifacts due to metal clips and gas, may give rise to poor spatial resolution and limited interpretation. Reviewing thin section and multiple planes may help overcome some of these issues 6.
Artefactual narrowing and pseudo-stricture of the extrahepatic bile duct can be caused by pulsatile vascular compression of the hepatic and gastroduodenal arteries, and it should not be misdiagnosed as a bile duct stricture, tumor or stone 10,11.










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.