Myxopapillary ependymomas are a variant type of ependymoma that occurs predominantly in the filum terminale and/or conus medullaris. They are the most common tumors of the cauda equina region and tend to result in CSF seeding.
On this page:
Epidemiology
Myxopapillary ependymomas represent 1-5% of all spinal tumors and 13% of all spinal ependymomas 14. They tend to have an earlier clinical presentation than other spinal ependymomas, with a mean age of presentation of 35 years. There is a slight male predominance.
Clinical presentation
The most common presenting symptoms are low back, leg or sacral pain. Up to 25% of patients may present with leg weakness or sphincter dysfunction.
They may occasionally present as a subarachnoid hemorrhage 8.
Pathology
Etiology
They are thought to arise from the ependymal glia of the filum terminale.
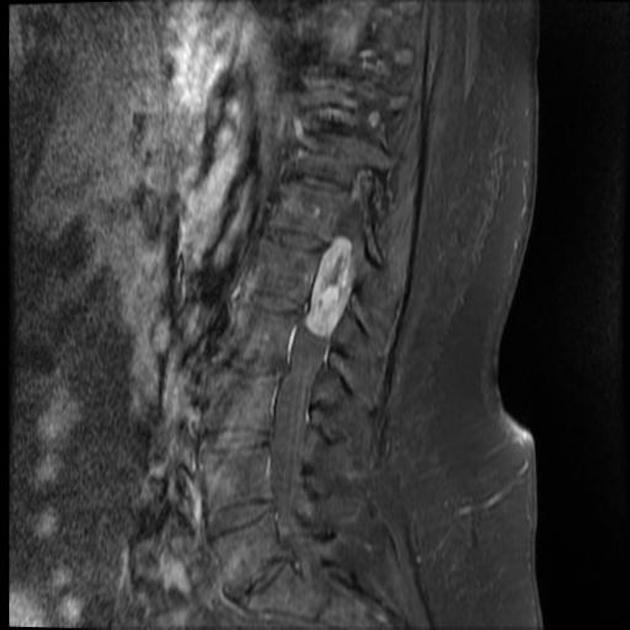
Location
The vast majority are intradural and extramedullary spinal tumors, occurring in the lumbosacral spine involving the filum terminale and/or conus medullaris. Less commonly, they extend from the lumbar to the thoracic spine 10. Rarely, they can arise in the cervicothoracic spine or fourth ventricle 11.
Grading
Historically, myxopapillary ependymomas were considered grade I tumors, however, in the 5th edition (2021) of the WHO classification of CNS tumors they have been upgraded to grade 2 tumors in recognition of the fact that local recurrence is similar to that of other spinal cord ependymomas 12,13.
Macroscopic appearance
They are typically lobulated, encapsulated, and oval or sausage-shaped. They often have associated hemorrhage and may calcify or undergo cystic degeneration 9.
Microscopic appearance
Histologically, they contain papillary elements arranged radially around a hyalinized fibrovascular core, forming perivascular pseudorosettes, with myxoid material between the blood vessel and tumor cells 9. "Balloons" (rounded eosinophilic PAS positive structures) are sometimes encountered 9.
Molecular markers
As is the case with ependymomas generally, myxopapillary ependymomas are GFAP, S100, and vimentin positive 9. CD99, AE1/AE3 and NCAM1 are also commonly positive 9.
The diagnosis can be supported by DNA methylation 14.
Radiographic features
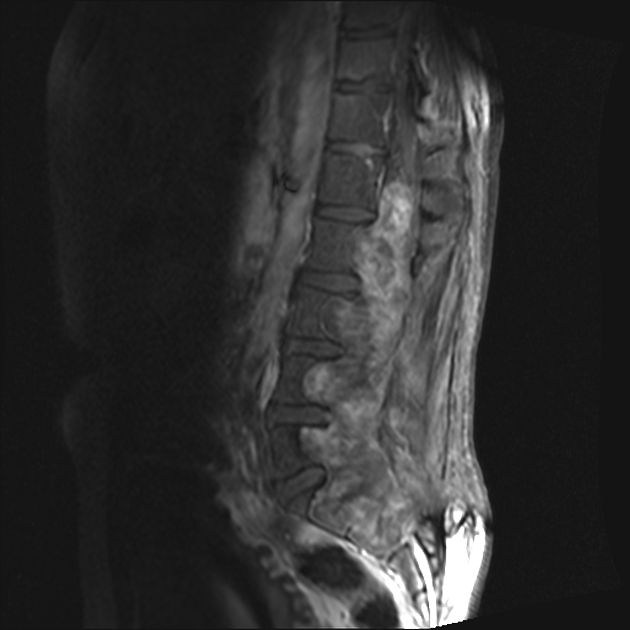
Plain radiograph / CT
If they become large, myxopapillary ependymomas may expand the spinal canal, cause posterior vertebral body scalloping and extend out of the neural exit foramina.
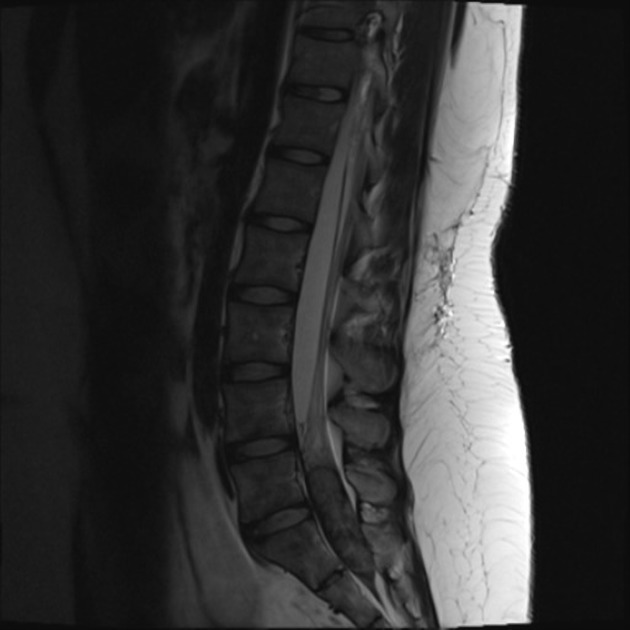
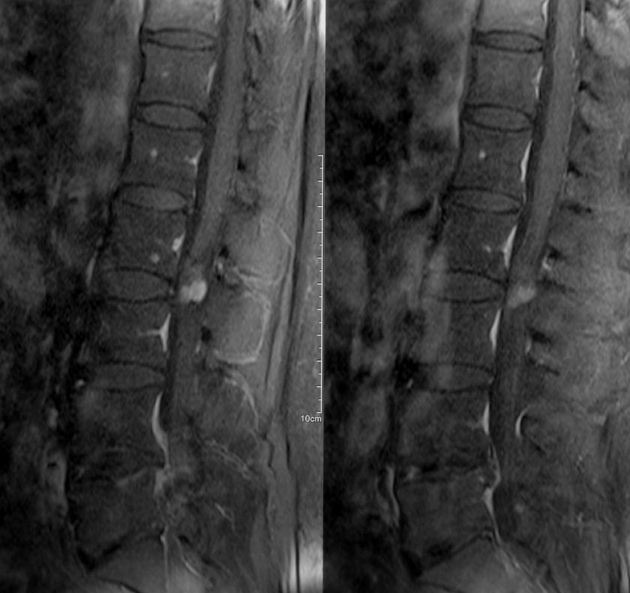
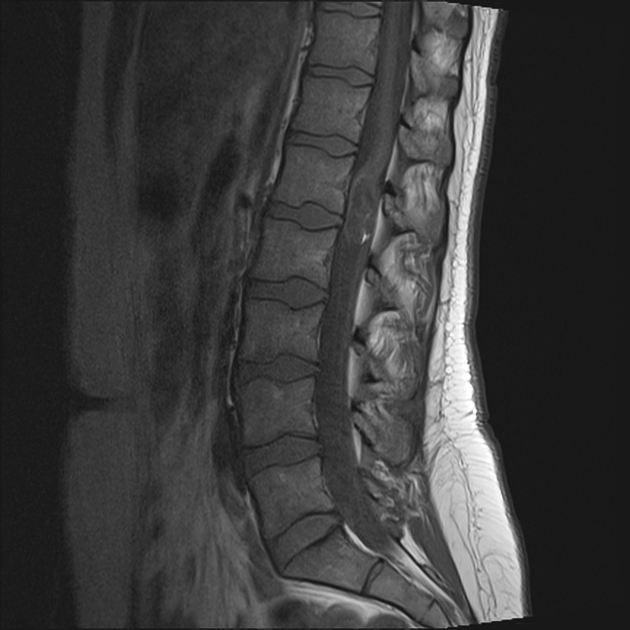
MRI
They are well-defined intradural tumors. Classically, they present when larger and sausage-shaped, spanning more than one vertebral level, but small oval tumors are also seen. Smaller tumors tend to displace the nerve roots of the cauda equina; larger tumors often compress or encase them 8.
-
T1
usually isointense
prominent mucinous component occasionally results in T1 hyperintensity
hemorrhage and calcification can also lead to regions of hyper- or hypointensity 14
-
T2
overall high intensity 14
low intensity may be seen at the tumor margins because of hemorrhage, called the cap sign (myxopapillary ependymomas are the subtype of ependymomas that are most prone to hemorrhage 8)
calcification may also lead to regions of low T2 signal
-
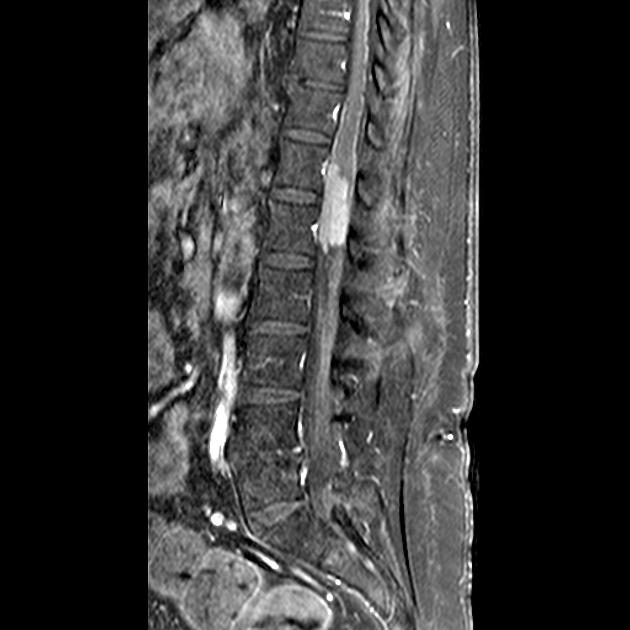
T1 C+ (Gd)
enhancement is virtually always seen 14
the enhancement pattern is typically homogeneous, however, they can have a variable enhancement pattern that, in part, depends on the amount of hemorrhage present
-
T2*/SWI
hemorrhage is common and may lead to internal signal heterogeneity or superficial siderosis 14
Treatment and prognosis
Myxopapillary ependymomas are generally slow-growing but are considered WHO grade 2 tumors 13. CSF dissemination is common and multiple lesions are seen in ~30% (range 14-43%) of cases 4,14. Some sacral lesions are locally aggressive and metastasize to lymph nodes, lungs, and bone. Aggressive behavior is more commonly seen in children 9.
They can often be excised completely. In these cases, the prognosis is excellent, with 5-year-survival over 98% 9.
If the tumor has extended to the conus medullaris, resection is often incomplete, with a greater risk of local recurrence, and there is a greater risk of neurologic deficit 11.
Differential diagnosis
Differential diagnosis of a small conus and filum terminale myxopapillary ependymoma includes:
cauda equina neuroendocrine tumor (formerly known as paraganglioma)
Differential diagnosis of a large myxopapillary ependymoma that causes sacral destruction:
aneurysmal bone cyst: involving the spine
giant cell tumor: involving the spine















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.