Osteoarthritis
Updates to Article Attributes
Osteoarthritis (OA), or degenerative joint disease (DJD),
Terminology
Given thatSome authors prefer the term osteoarthrosis instead of osteoarthritis isas some authors do not primarilybelieve in an inflammatory process,cause as might be suggested by the suffix "itis", some authors prefer the term osteoarthrosis insteadnamesakeosteoarthritis, which is a different clinical and radiological entity, the condition is sometimes called non-erosive osteoarthritis.
Epidemiology
Osteoarthritis is common, affecting ~25% of adults 7.
Clinical presentation
Patients present with decreased function from joint pain, instability and stiffness 7,10. Many cases of radiological OA are asymptomatic and conversely clinically apparent OA may not manifest radiographic change 9,10.
Pathology
Primary osteoarthritisThe pathogenesis and pathophysiology of OA are yet to be fully understood 7. Despite emphasis being placed on articular cartilage degeneration, the remainder of the joint is involved including bone remodelling, osteophyte formation, ligamentous laxity, periarticular muscle weakness and synovitis8,10.
Location
OA can affect both the lessaxial and appendicular skeleton. The most common variant and is characterised by the peripheral joints affected include ref:
Risk factors
Strong risk factors for developing OA include 7,10:
- obesity
- increasing age
- female sex (particularly between ages 50-80)
- family history
Classification
Osteoarthritis can be:
-
primary/idiopathic/typical
- absence of an antecedent insult
. There is a - strong genetic component
5.Secondary osteoarthritis is more common, caused by
- absence of an antecedent insult
-
secondary/atypical
- abnormal mechanical forces (e.g. occupational stress,obesity)
or by a - previous joint
insultinjury-
trauma
- either osseous or soft tissue
- major cause in young adults 9
- prior surgery, e.g. meniscal debridement, anterior cruciate ligament reconstruction
-
crystal deposition (e.g.
traumagout, CPPD). - haemochromatosis
-
trauma
- abnormal mechanical forces (e.g. occupational stress,obesity)
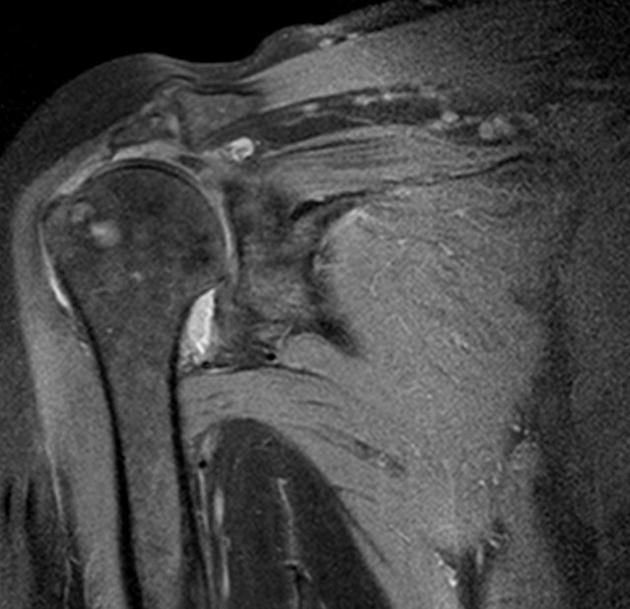
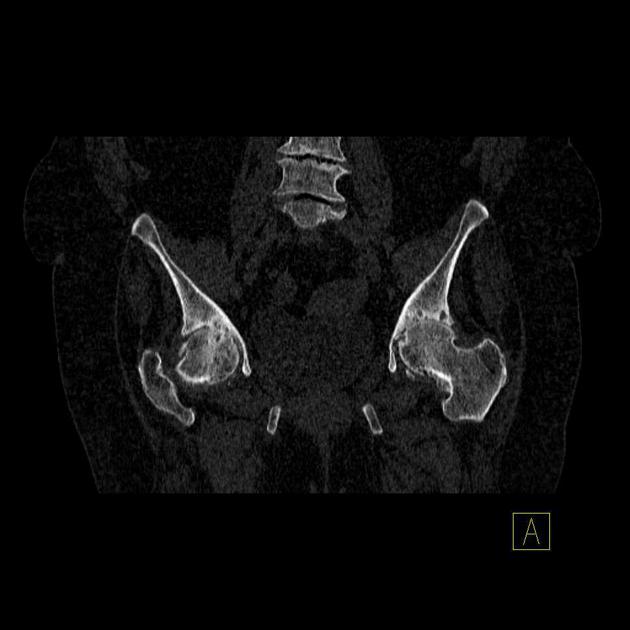
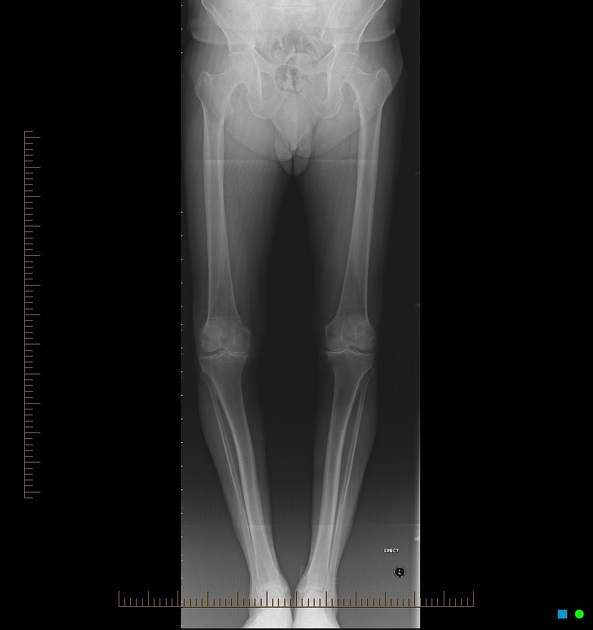
Radiographic features
Key radiographic features are joint space narrowing (JSN), sclerosis, and osteophytosis. If all three of these findings are not present, another diagnosis should be considered.
Joint space narrowing
- characteristically asymmetric
- least specific: present in many other pathological processes
Sclerosis
- sclerotic changes occur at joint margins
- frequently seen unless severe osteoporosis is present
Osteophytosis
- i.e. development of osteophytes
- common DJD finding
- will also be diminished in the setting of osteoporosis
- some osteophytes carry eponymous names,
as discussed below
It affects the distal interphalangeal joints (e.g. Heberden nodes), the proximal interphalangeal joints (Bouchard nodes), (mnemonic H-D, B-P) and the base of the thumb in a bilaterally symmetric fashion. If it is not bilaterally symmetric, the diagnosis of primary osteoarthritis should be questioned.
Joint erosions
- several joints may exhibit degenerative erosions 1
- temporomandibular joint
(TMJ) - acromioclavicular joint
(ACJ) - sacroiliac joints
(SIJ) - symphysis pubis
- temporomandibular joint
Subchondral cyst
- also known as a geode
- cystic formations that occur around joints in a variety of disorders, including, rheumatoid arthritis, calcium pyrophosphate dihydrate crystal deposition disease (CPPD) and avascular necrosis.
Treatment and prognosis
Simple analgesiaThere is no effective treatment to slow or reverse the mainstaychanges of osteoarthritis 7. The mainstays of treatment for most patientsinclude exercise, walking aids, bracing, and analgesia (including intra-articular steroid injections) 8. Arthroplasty can result in improved function and reduced pain 10.
There is increasing evidence that the condition erosive osteoarthritis (EOA) is a severe form of 'normal' osteoarthritis and not a discrete disease entity, and that therefore a subset of patients may progress from the non-erosive to the erosive form 6.
References changed:
- 7. Chen D, Shen J, Zhao W et al. Osteoarthritis: Toward a Comprehensive Understanding of Pathological Mechanism. Bone Res. 2017;5(1):16044. <a href="https://doi.org/10.1038/boneres.2016.44">doi:10.1038/boneres.2016.44</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/28149655">Pubmed</a>
- 8. Kolasinski S, Neogi T, Hochberg M et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020;72(2):220-33. <a href="https://doi.org/10.1002/art.41142">doi:10.1002/art.41142</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/31908163">Pubmed</a>
- 9. Zhang Y & Jordan J. Epidemiology of Osteoarthritis. Clin Geriatr Med. 2010;26(3):355-69. <a href="https://doi.org/10.1016/j.cger.2010.03.001">doi:10.1016/j.cger.2010.03.001</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/20699159">Pubmed</a>
- 10. Litwic A, Edwards M, Dennison E, Cooper C. Epidemiology and Burden of Osteoarthritis. Br Med Bull. 2013;105(1):185-99. <a href="https://doi.org/10.1093/bmb/lds038">doi:10.1093/bmb/lds038</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/23337796">Pubmed</a>
Tags changed:
- overview
- oa














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.