The Ovarian-Adnexal Reporting and Data System Ultrasound (O-RADS US) forms the ultrasound component of the Ovarian-Adnexal Reporting and Data System (O-RADS). This system aims to ensure that there are uniform unambiguous sonographic evaluations of ovarian or other adnexal lesions, accurately assigning each lesion to a risk category of malignancy being present, which informs the appropriate management to be instituted.
For MRI, see the Ovarian-Adnexal Reporting and Data System MRI (O-RADS MRI).
These recommendations have been published to guide the management of "average-risk patients without acute symptoms" who demonstrate adnexal lesions. Individual case management may be modified based on professional judgment, regardless of the O-RADS ultrasound recommendations1.
On this page:
Images:
Classification
For risk stratification, the O-RADS US system uses five categories (O-RADS 1–5), from normal (1) to high risk of malignancy (5). An O-RADS US 0 (zero) category is used for an incomplete evaluation.
An external diagnostic validation study has suggested that both the O-RADS lexicon and the IOTA 2-step strategy are effective in stratifying patients into risk groups 6. However, the observed malignancy rate in O-RADS 2 was approximately 1.1%, not clearly below 1%.
O-RADS US 0
an incomplete evaluation
O-RADS US 1
Physiologic category (normal premenopausal ovary)
ovarian follicle (<3 cm)
corpus luteum (typically <3 cm)
O-RADS US 2
Almost certainly benign category (<1% risk of malignancy) - consider gynecology referral for cases that require imaging follow-up
-
simple cyst 3-5 cm
premenopausal: no follow-up
postmenopausal: 1-year follow-up
-
simple cyst 5-10 cm
premenopausal: 1-year follow-up
postmenopausal: 1-year follow-up
-
non-simple but smooth unilocular cyst OR smooth bilocular cyst <3 cm
premenopausal: no follow-up
postmenopausal: 1-year follow-up
-
non-simple but smooth unilocular cyst OR smooth bilocular cyst 3-10 cm
premenopausal: 6-month follow-up
postmenopausal: 6-month follow-up
-
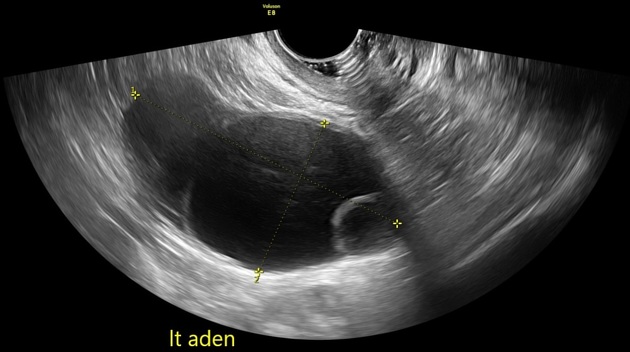
lesions with "classical ultrasound characteristics" of the following but may have specific recommendations and measure < 10 cm:
O-RADS US 3
Low risk of malignancy (1% to <10%) - needs a referral to ultrasound specialist or gynecologist with a view to MRI
unilocular or bilocular >10 cm (simple or non-simple)
lesions looking like typical dermoids, endometriomas, or hemorrhagic cysts >10 cm
multilocular cyst <10 cm smooth inner wall with color score 1-3
solid lesion - smooth outer contour, any size, color score 1
solid lesion - smooth outer contour, any size, color score 2-3 with shadowing
unilocular irregular cyst of any size
O-RADS US 4
Lesions with an intermediate risk of malignancy (10% to <50%) - needs ultrasound specialist review or MRI as well as management by a gynecologist with gynecological oncology support or solely by a gynecological oncologist
unilocular cyst with a solid component, any size, 1-3 papillary projections, any color score
multilocular cyst with solid component, any size, color score 1-2
-
multilocular cyst without solid component
>10 cm, smooth inner wall with color score 1-3
any size smooth inner wall with color score of 4
any size with an irregular inner wall or irregular septations of any color score
solid - smooth outer contour, any size, color score 2-3
bilocular irregular cyst of any size, no solid components
O-RADS US 5
Lesions with a high risk of malignancy (≥50%) - needs a referral to a gynecological oncologist
presence of ascites / peritoneal nodularity
unilocular cyst with 4 or more papillary projections
multilocular/bilocular cyst with a solid component - color score 3-4
solid lesion - smooth outer contour, any size, color score 4
solid lesion - irregular contour, any size, any color score
Color scoring (CS) indicator
CS1: no flow
CS2: minimal flow
CS3: moderate flow
CS4: strong flow
History and etymology
O-RADS was developed and published in 2018 by an international multidisciplinary committee, comprising clinicians and researchers from the fields of radiology, gynecology, pathology, and gynecologic oncology, and sponsored by the American College of Radiology (ACR). It was originally designed for sonographic evaluation, and in 2020 the system was extended to include MRI evaluation. The O-RADS MRI was an evolution from the AdnexMR Scoring System published in 2012. An update to the O-RADS assessment system was published by the ACR in 2022.
See also
External links
If any of these links are broken or for other problems and questions, please contact editors@radiopaedia.org.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.