Relapsing polychondritis is a rare multisystem disease characterized by recurrent inflammation of cartilaginous structures in the body. It can also affect other proteoglycan-rich structures 1.
On this page:
Epidemiology
The condition is extremely rare with an estimated incidence of ~1 in 285,000. Patients typically present in middle age and there is equal occurrence in men and women 11.
Clinical presentation
Respiratory symptoms are seen in ~20% of patients at presentation and eventually ~60% will develop respiratory tract involvement which is manifested by a combination of symptoms including laryngeal tenderness, hoarseness, dyspnea, and stridor/wheeze.
Pathology
An autoimmune-mediated mechanism has been postulated.
Location
Commonly affected areas include:
tracheobronchial tree: present in up to 50% of cases 2,3
peripheral joints
Other areas that can be involved include 8:
Radiographic features
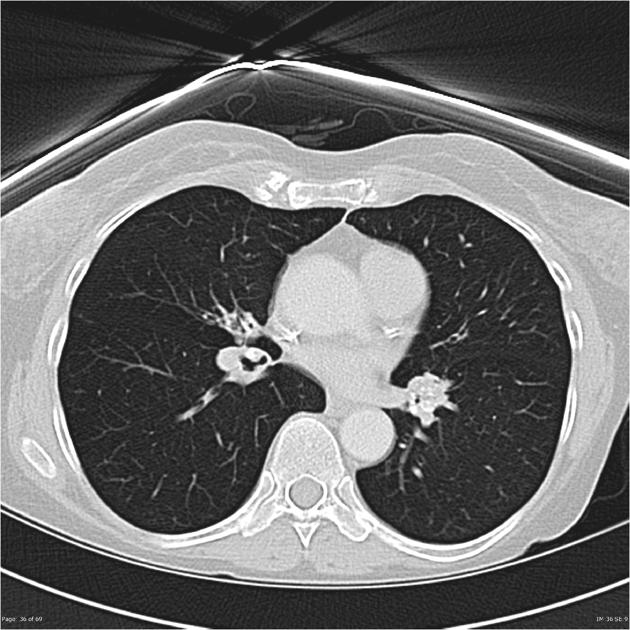
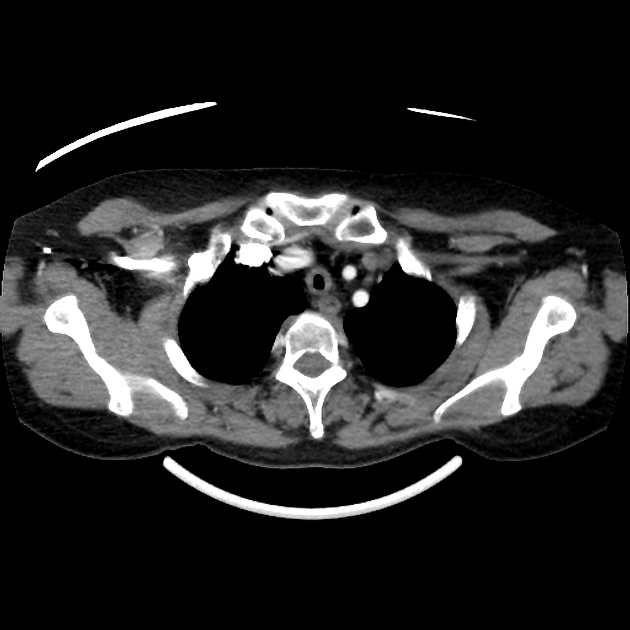
CT
In the chest:
increased airway wall attenuation: common 4
smooth anterior and lateral tracheal wall thickening with sparing of the posterior membranous wall: if present is considered virtually pathognomonic 2
luminal narrowing: tracheobronchial and peripheral bronchial
accompanying dense tracheal cartilage calcification
dynamic imaging may demonstrate airway collapse best seen at end-expiratory phase (dynamic tracheal collapse)
lobar air trapping
bronchiectasis: uncommon
lymphadenopathy is generally not a feature 9 but may be present in some cases 12
Treatment and prognosis
Many patients have a fluctuating but progressive course. Most morbidity and mortality is due to respiratory involvement (frequent respiratory infection and airway collapse). Medical management (with corticosteroids, NSAIDs, azathioprine, cyclosporine) is the mainstay of treatment.
Selected surgical options include 7:
tracheostomy: for localized upper airway involvement
endobronchial polymeric silicone stent placement to aid/maintain airway patency
Differential diagnosis
Tracheobronchial abnormalities that also spare the posterior wall:
-
tracheobronchopathia osteochondroplastica
thickening is irregular and nodular
submucosal ossifications and calcifications can be seen extending from the tracheal cartilage rings
Tracheobronchial abnormalities that involve the posterior wall:
-
granulomatosis with polyangiitis (GPA)
circumferential involvement
the subglottic trachea is the most commonly affected area (involvement down to the main bronchi is possible)
ulcerations of the trachea are possible
-
circumferential involvement
may appear as focal or diffuse narrowing
calcifications of the tracheal wall can be seen
-
post-intubation tracheal stenosis
focal involvement
irregular and concentric stenosis
For tracheal narrowing consider: differential of diffuse tracheal narrowing







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.