Sialolithiasis refers to the formation of calculi (sialoliths) inside the ducts or parenchyma of salivary glands and most commonly occurs in the submandibular glands and their ducts.
On this page:
Epidemiology
Sialolithiasis is the most common disease of salivary glands, accounting for approximately 50% of all major salivary gland pathology 5. The submandibular salivary gland is most commonly affected (80-90% of cases) with almost all the remaining cases located in the parotid duct 1,2,5,6. This is primarily believed to be due to the increased viscosity of the secretions from the submandibular gland 6.
Sialolithiasis is a disease of adults, typically between 30 and 60 years of age. There is a male predilection 5.
Clinical presentation
Typically patient presents with a history of recurrent swelling and pain in the involved gland usually associated with eating due to obstructions of the draining duct, e.g. submandibular duct (Wharton duct) thus slowing down or disabling the flow of saliva. This, in turn, predisposes infection of the gland proximal to the obstruction, resulting in bacterial sialadenitis.
In chronic cases of obstruction, the gland undergoes fatty atrophy and becomes asymptomatic, unless secondarily infected.
Radiographic features
Multimodal imaging can be used to evaluate these stones.
Plain radiograph
Not all stones are radiopaque. Plain radiography is able to visualize only 80-90% of submandibular stones (which are usually located in the duct 6) and ~60% of parotid duct stones (more frequently found within the gland itself 6) presumably due to differences in the composition of the secretion of the parent glands 2,3. Oblique views are often required to project the stones away from adjacent bone and teeth.
Sialography
Sialography excels at delineating the exact size and location of stones within the salivary gland ducts. The stone will be visualized as a filling defect within the duct. In some cases, the contrast will not be able to pass beyond the stone.
However, if active infection is suspected, sialography is contraindicated due to the risk of exacerbating the extent of infection 2.
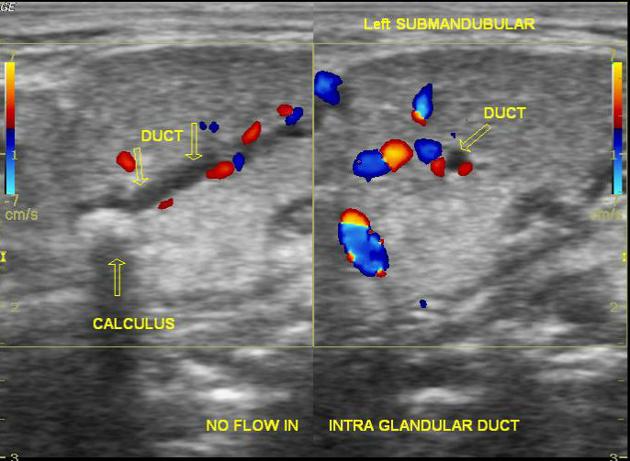
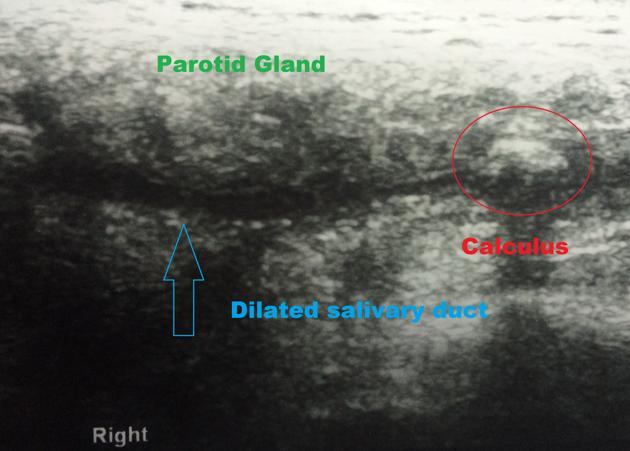
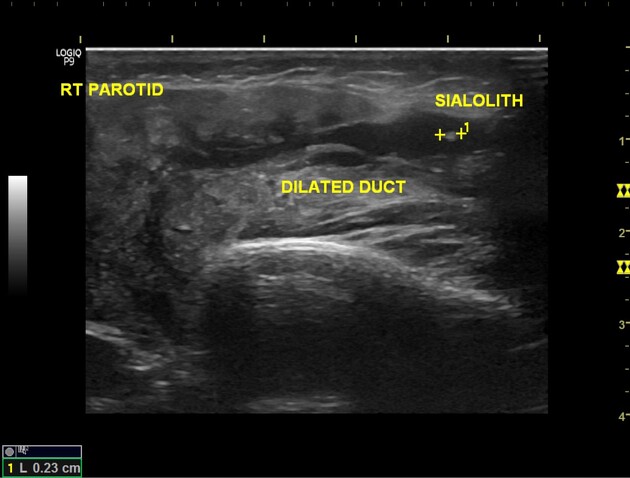
Ultrasound
Ultrasonography is well-established in cases of clinical suspicion of sialolithiasis, able not only to visualize the stone in many instances but also the gland 2,3. Stones appear as strongly hyperechoic lines or points with distal acoustic shadowing represent stones. Small stones (<2 mm) may however not shadow 2,3. Ultrasound is able to visualize stones that are radiolucent.
In acute obstructive cases, the gland appears enlarged and excretory ducts proximal to the stone may be visibly dilated.
The examination is best performed with small high-frequency intraoral probes 5.
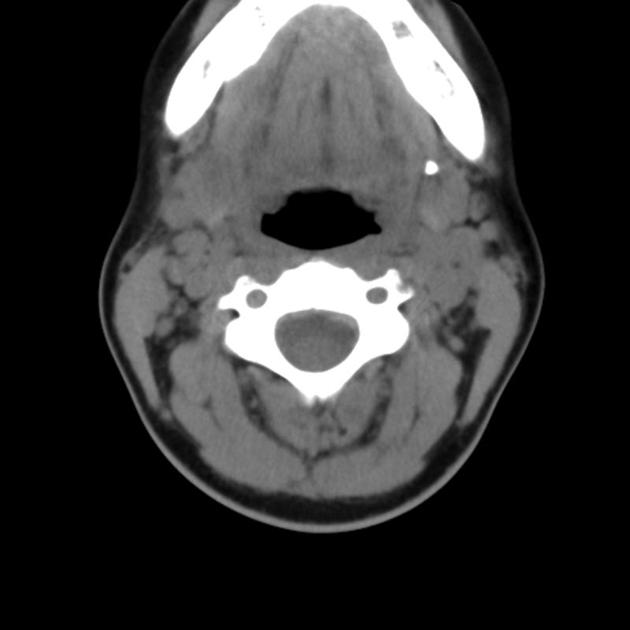
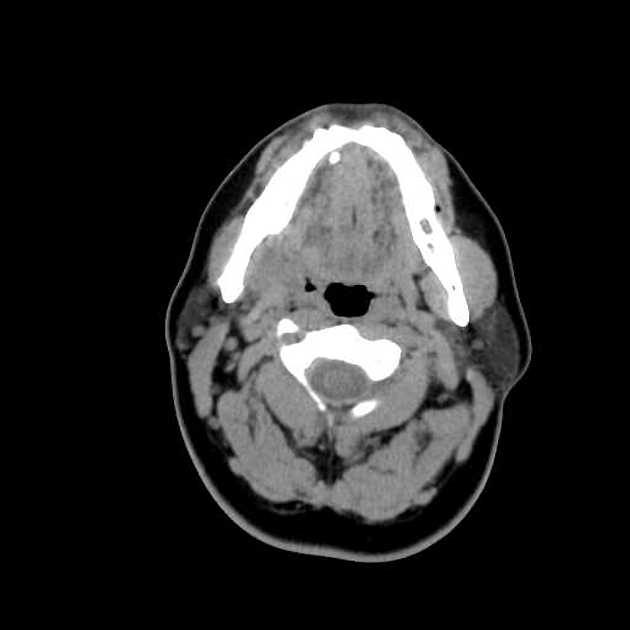
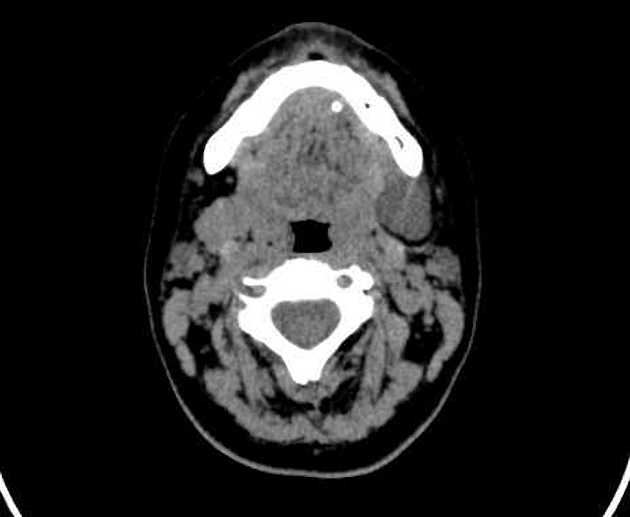
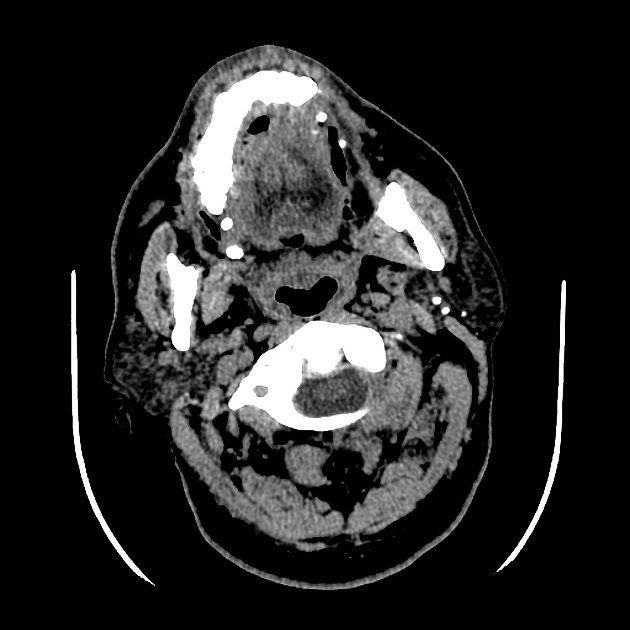
CT
CT is excellent at visualizing stones both within the duct and within the gland. The spatial resolution is not as high as plain radiography and as such very small stones may not be evident.
Additionally, CT is able to assess the gland, although not as well as MRI (see below). In acute obstructive cases, the gland may appear enlarged, hyperdense and associated with stranding and enhancement following contrast administration.
In chronic cases, fatty atrophy will be evident, with the parenchyma reduced in volume and replaced by fat.
MRI
MRI is able not only to visualize larger stones but able in many instances to map the ductal anatomy and to assess the gland 2,4.
Stones appear as low signal regions (on all sequences) outlined by high signal saliva on T2 weighted images 2.
MRI is able to distinguish acute from chronic obstruction as well as glands with only incomplete obstruction 1.
In the acute setting, glands are enlarged and demonstrate inflammatory changes:
T1: reduced signal compared to the other side
T2: increased signal (best seen on fat suppressed sequences)
In chronic cases, the gland is reduced in size and demonstrates fatty atrophy 1:
T1: increased signal compared to the other side
T2: a reduced signal of gland parenchyma which is itself reduced in amount
In cases where a small non-obstructive sialolith is present, the gland may appear entirely normal.
Treatment and prognosis
In many instances, conservative medical management suffices. Hydration and moist heat are helpful. NSAIDs may be beneficial. Sucking on something sour, such as a lemon, may increase salivation and promote spontaneous expulsion of the stone.
If these measures are unsuccessful, surgical removal of the salivary stone from the duct may be required. In chronic cases or if the stone is positioned within the parenchyma of the submandibular salivary gland, the gland may need to be excised.
Increasingly non-surgical options exist to treat symptomatic stones, including 4:
extracorporeal sialolithotripsy
endoscopic stone removal
endoluminal balloon dilatation and stone extraction
Differential diagnosis
The differential diagnosis really depends on the modality. In general, there is little confusion as the clinical presentation is relatively specific. For plain radiography and CT, the differential is that of other calcific foci, which include 2:
hemangioma/phlebolith
atherosclerotic calcification
Filling defects on sialography may be caused by:
an injected bubble of air
tumor
blood clot


































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.