Squamous cell carcinoma of the tongue has tobacco smoking and alcohol ingestion as major risk factors and spans two regions: the anterior two-thirds (oral tongue) is a common subtype of squamous cell carcinoma of the oral cavity whereas the posterior third (base of tongue) is considered part of the oropharynx.
On this page:
Epidemiology
The epidemiology of squamous cell carcinoma of the tongue including its risk factors are similar to squamous cell carcinomas elsewhere in the upper aerodigestive tract, with tobacco smoking and alcohol ingestion being major risk factors 1-3,9.
Of note, the role of human papillomavirus (HPV) as an etiological factor for squamous cell carcinoma is strongest in oral cavity (compared to other regions in the head and neck), with HPV DNA isolated from up to 50% of cases, and thought responsible for the tumor in over half of these 1-3.
Clinical presentation
Approximately 20% of all SCCs of the oral cavity arise from the tongue, and approximately 75% of all squamous cell carcinomas of the tongue arise from the anterior two-thirds of the tongue (oral part) 9.
Squamous cell carcinoma of the tongue usually arises from the ventrolateral aspect of the mid and posterior tongue, probably due to adjacent pooling of carcinogens 1. Despite the ease of inspecting the tongue by both patient and physician, they often present late, as they are usually painless and often ignored by the patient. Eventually, they present as a non-healing ulcer which demonstrates growth over time 6.
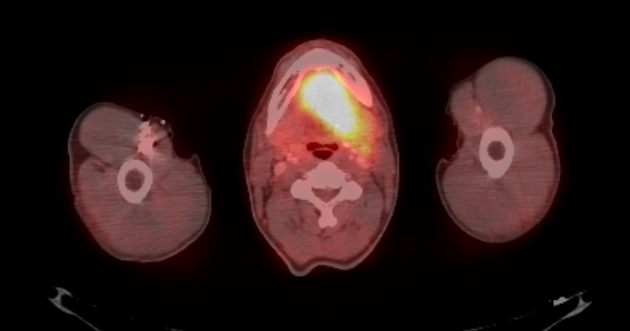
Due to the extensive lymphatic drainage of the tongue, nodal metastases are common (37-58%) 7,9 at the time of diagnosis (more common than any other site in the oral cavity) 6. A neck mass may, therefore, be the presenting complaint.
Radiographic features
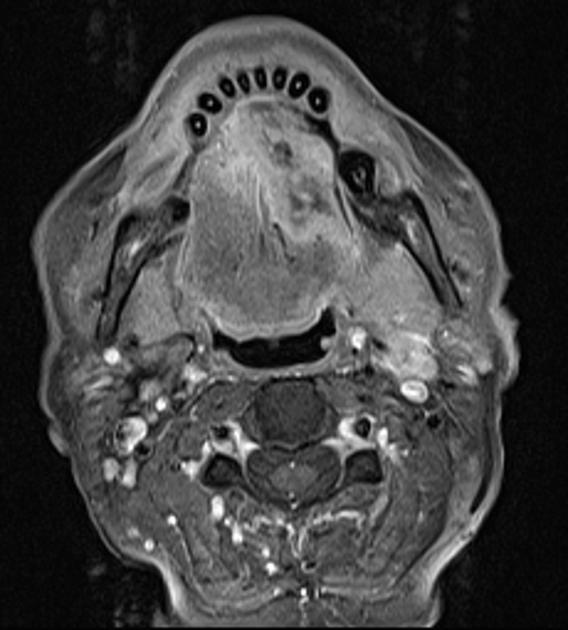
A common staging system is used for all squamous cell carcinomas of the oral cavity, with tumor staging being based on size and extension into adjacent structures. Nodal staging is the same as that used for squamous cell carcinomas of the oral cavity, oropharynx, hypopharynx and larynx (see: staging of oral cavity squamous cell carcinomas).
Whether CT or MRI is used the same features should be assessed 14:
- the size of tumor and tumor thickness
- extension across the midline
- extension beyond the intrinsic muscles of the tongue
- involvement of adjacent structures
- neurovascular bundle and submandibular duct in the floor of mouth
- mandible
Lymphatic drainage of the tongue is extensive, accounting presumably for the high rate of nodal metastases present at the time of diagnosis. Drainage patterns depend on the location of the primary lesion 6:
- anterior tongue: level Ia nodes (submental nodes)
- lateral tongue
- level Ib nodes: submandibular and
- level II nodes: upper jugulodigastric nodes
- potentially drain directly to level IV nodes 6
- posterior tongue: level II nodes (upper jugulodigastric nodes)
It is important to remember that significant lymphatic drainage occurs across the midline, and thus the nodes of both sides of the neck need to be carefully examined for the presence of nodal metastases.
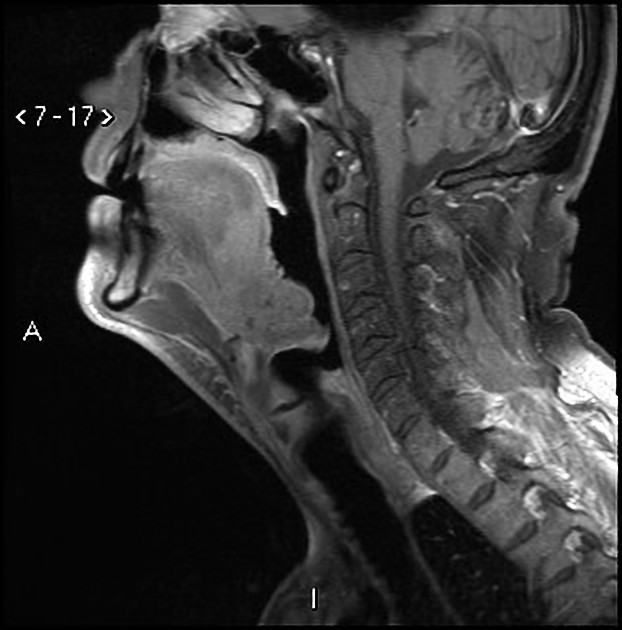
The incidence of lymph node metastases correlates with tumor thickness, which is best assessed on coronal images 7.
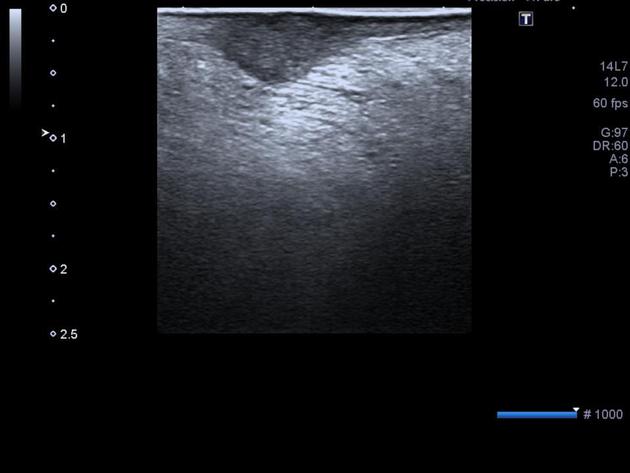
US
The primary tumor can be assessed directly with a small high-frequency probe evaluate tumor thickness. Tumor thickness of ≤7 mm has a 12% risk of lymph node metastasis whereas a tumor thickness >7 mm has a 57% risk of lymph metastasis in one series of 65 patients 12.
Ultrasound is also used for assessment of cervical lymph nodes and to aid in FNAC of suspicious nodes.
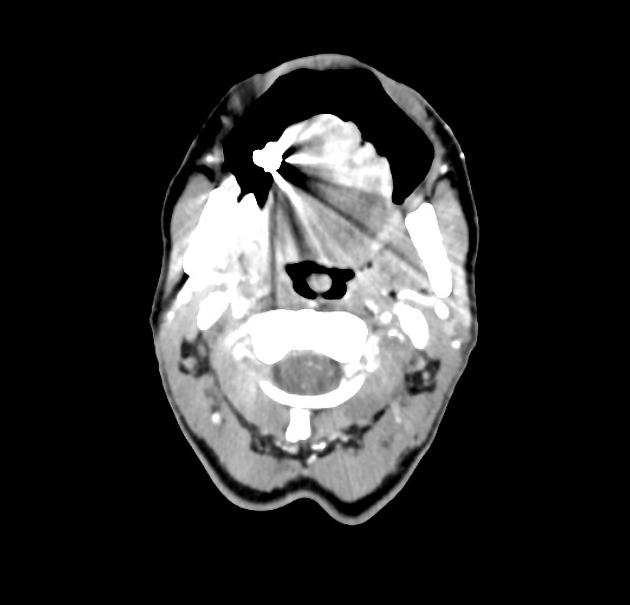
CT
CT is the most commonly used modality for assessment of tongue squamous cell carcinoma, able to both locally stage the tumor and assess for nodal metastases.
Lesions typically appear of soft tissue attenuation, usually a little more attenuating than normal tongue musculature (on account of the keratin) and enhance following contrast administration.
Bony algorithm thin section CT is the most sensitive modality for assessing early bony erosion.
Non-contrast scans of the neck may demonstrate increased attenuation of involved nodes due to keratin production by tumor deposits 8.
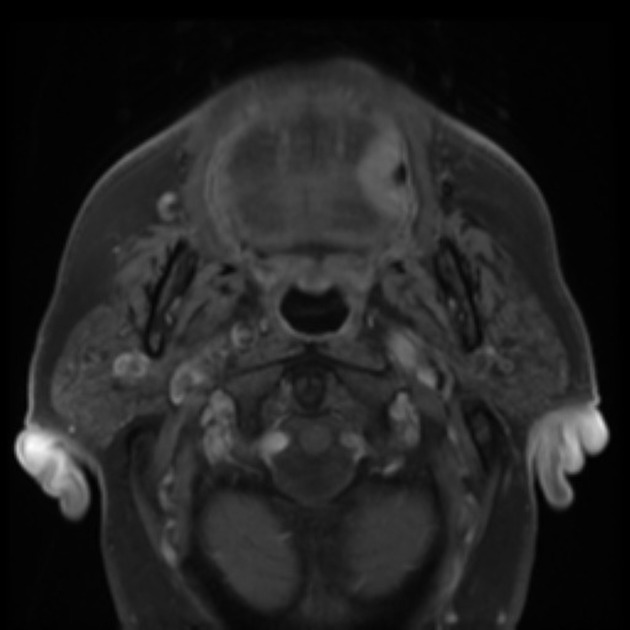
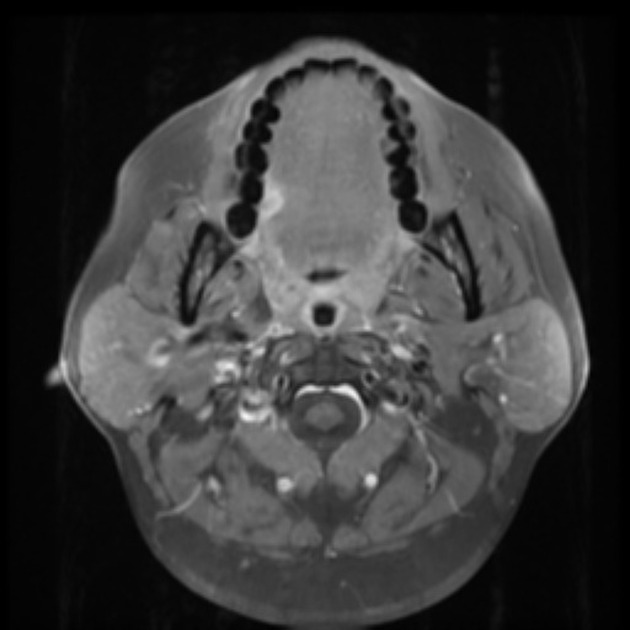
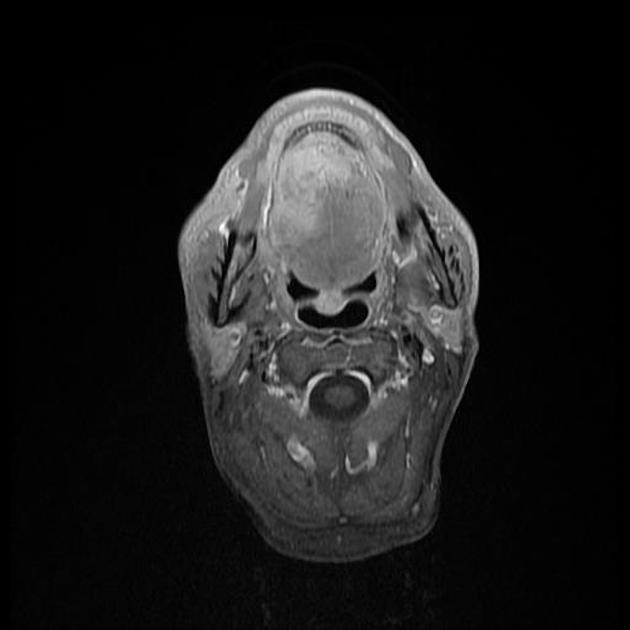
MRI
MRI is excellent at identifying the extent of tumor infiltration and is especially useful in patients with significant dental amalgam which causes artifact on CT 7,9.
- T1: intermediate to low signal
- T2: intermediate to high signal
- T1 C+ (Gd) with fat saturation: enhances
In larger lesions that abut the mandible, MRI is more sensitive than CT at identifying early marrow change (low T1 signal, high T2 signal, enhancement) but less sensitive at visualizing cortical erosion 9.
Treatment and prognosis
For small tumors excision is possible with a hemiglossectomy or partial hemiglossectomy. Reconstruction of the tongue depends on the size of the defect. When less than a third of the tongue has been resected primary closure is possible. Larger defects require pedicle or free-flap reconstruction 1,4. Larger lesions which cross the midline, although sometimes technically resectable with a total glossectomy, are usually not resected due to the operation being poorly tolerated 1.
In tumors that extend laterally across the floor of the mouth and into the mandible, resection is challenging often requiring segmental mandibulectomy and reconstruction 5.
Radiotherapy is often used either in conjunction with surgery or alone in advanced cases.
Differential diagnosis
The differential diagnosis of squamous cell carcinoma of the tongue is essentially that of other malignant lesions of the oral cavity as well as a few non-neoplastic lesions. It therefore includes:
- other malignancy
- lymphoma
- minor salivary gland tumors
- adenoid cystic carcinoma
- adenocarcinoma
- mucoepidermoid carcinoma
- sarcoma
- rhabdomyosarcoma
- liposarcoma
- infection: more a concern for the floor of mouth lesions, or those with involvement of the mandible
- normal adenoidal tissue: for a base of tongue lesion
Practical points
- ultrasound is more reliable than MRI at estimating tumor thickness, which can direct the need for neck dissection 13
- post-biopsy edema/hematoma can result in overestimation of tumor thickness 13





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.