Vertebral hemangiomas are the most common benign vertebral neoplasms. That said, they are not true neoplasms but venous malformations. They are usually asymptomatic and incidentally detected due to their characteristic features on imaging for other reasons. Rarely, they can be locally aggressive (see: aggressive vertebral hemangioma).
Please refer to the article on primary intraosseous hemangioma for a general discussion on this entity.
On this page:
Terminology
Atypical hemangiomas have lower fat content, lipid-poor hemangiomas is a term preferred by some authors to avoid confusion with aggressive vertebral hemangiomas 13.
Epidemiology
The incidence of vertebral hemangiomas is about 10% at autopsy 1. The majority of hemangiomas are incidentally noted on routine radiographs of the spine. Often, small hemangiomas cannot be visualized on radiographs and are found with more advanced imaging such as CT or MRI, or upon gross dissection. The occurrence of vertebral hemangiomas is seen slightly more in females for unknown reasons and is more symptomatic in the 4th decade of life.
Clinical presentation
Most hemangiomas are asymptomatic. The collapse of the vertebral body or encroachment into the neural canal are some of the classic causes of pain. An increase in activity can cause the vertebral hemangioma to become painful, such as starting to exercise, housework and such like. This is most likely due to axial loading through the body of the vertebra.
Pathology
They are composed of vascular spaces which causes a displacement of the bone. There are two main histopathological types 11:
cavernous (involves relatively large vessels)
capillary (involves small capillaries)
In some cases, specifically capillary types, lytic erosion into the epidural space can occur, however this is rare 2. They are slow-growing and most hemangiomas are asymptomatic.
Distribution
The majority of vertebral hemangiomas occur in the thoracic spine but they can be found throughout the spine.
Radiographic features
The classic “corduroy” or "jail bar" appearance is strongly associated with vertebral hemangiomas.
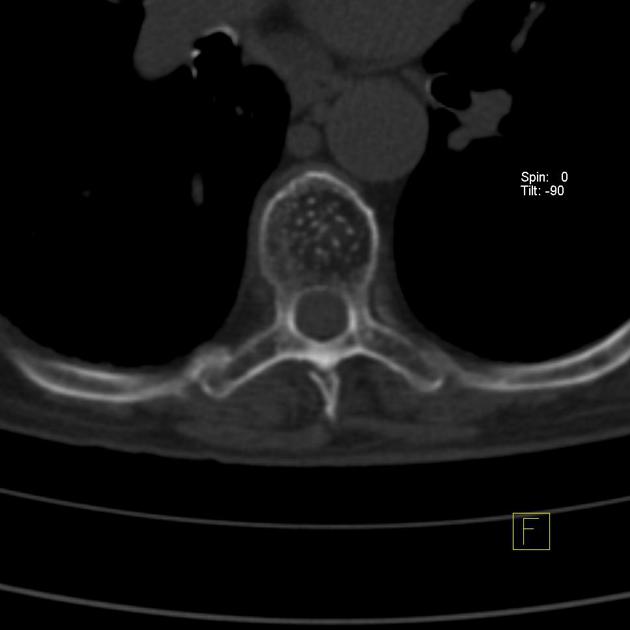
CT
Axial CT will show a “polka dot” or "salt and pepper" appearance due to the thickened vertebral trabeculae 3,4. On sagittal CT, vertebral hemangiomas typically show the "corduroy" sign due to thicker or denser vertical trabeculae 14.
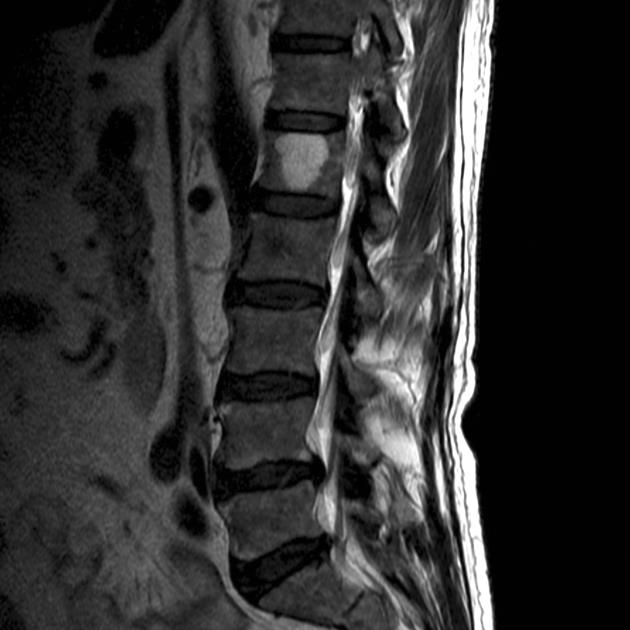
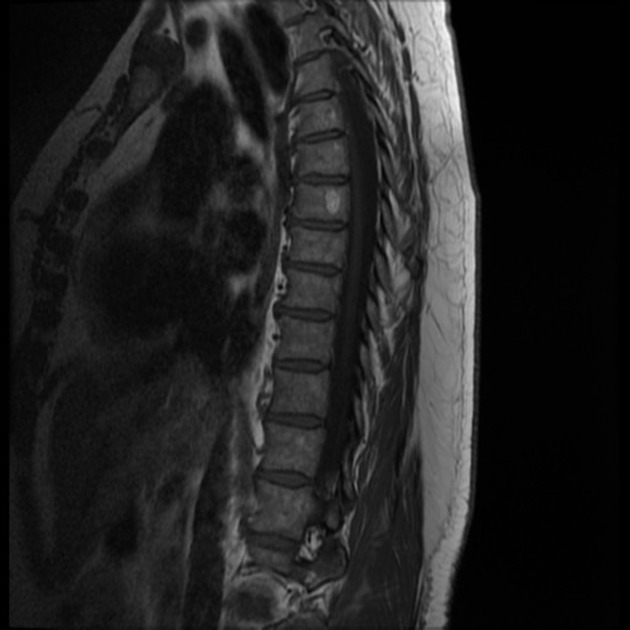
MRI
MRI shows extraosseous components better and depicts the hemangioma components as fat and water. Thickened trabeculae appear as low signal areas in both T1 and T2 images.
-
T1
typical: lipid-rich will demonstrate high signal
atypical: lipid-poor will demonstrate low signal
T2: bright/high-intensity signal, usually greater than on T1, due to its high water content
STIR: variable signal intensity depending on the amount of fat in the lesion relative to the vascularity
T1 C+: significant enhancement is seen due to high vascularity
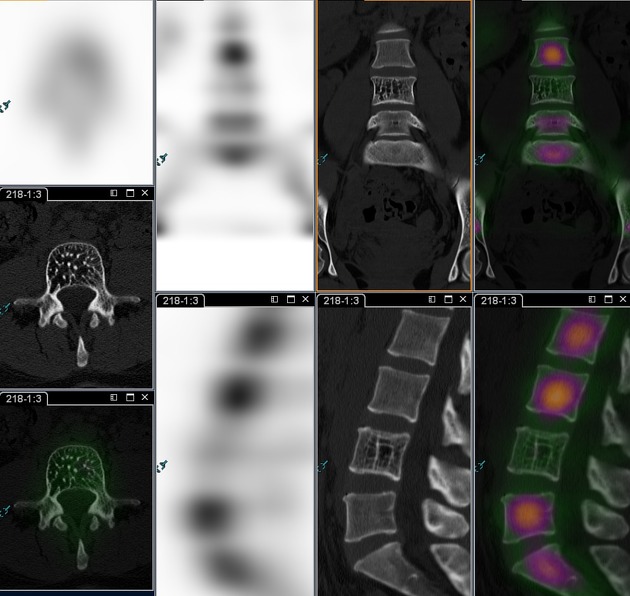
Nuclear medicine
Bone scintigraphy (99mTc MDP) tends to show no increased activity for hemangiomas with rare exceptions 16.
PET-CT
Vertebral hemangiomas are typically ametabolic with very rare exceptions 15.
Treatment and prognosis
Treatment for most hemangiomas is not necessary. When neurological deficits or severe pain treatment is necessary. In symptomatic lesions, there are many options that must be weighed. Radiotherapy, balloon kyphoplasty or transarterial embolization with associated laminectomy are some of those options 5.
Serious bleeding can be a complication so care must be taken when undergoing open procedures.
Differential diagnosis
metastases: usually have decreased signal intensity on T1 and increased signal intensity on T2
focal fatty marrow: will have decreased signal intensity on fat suppressed sequences











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.