Anaplastic astrocytomas are a historical term used to denote histological grade III diffuse astrocytic tumors (regardless of molecular markers). The term has been removed and is no longer recognized as a distinct entity as of the 5th edition (2021) of the WHO classification of CNS tumors 5.
On this page:
Terminology
Tumors once considered anaplastic astrocytomas are to be classified as either astrocytoma IDH-mutant grade 3 or grade 4 tumors or glioblastoma grade 4 according to their molecular characteristics (see astrocytic tumors).
Pathology
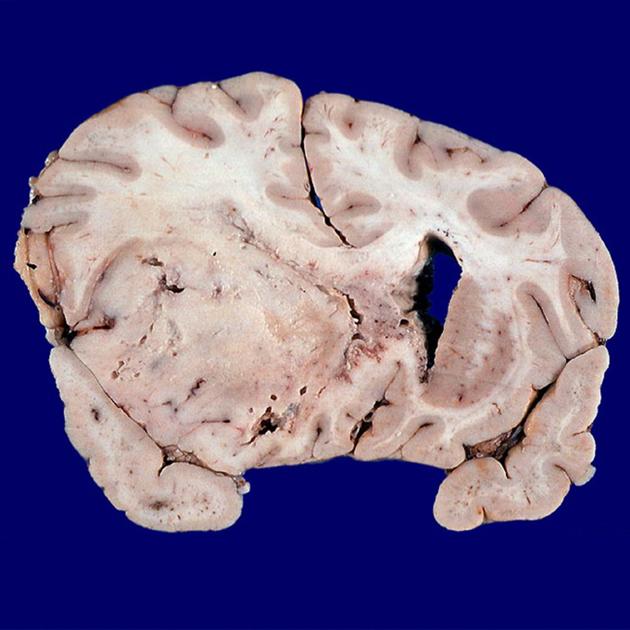
The histological features of anaplastic astrocytomas were intermediate between those of diffuse low-grade astrocytomas (WHO grade II) and what was then termed glioblastomas (WHO grade IV).
Note: the term glioblastoma as it is used does not equate to how it was used prior to the 5th edition of the WHO classification.
The key features present in anaplastic astrocytomas that were absent in low-grade tumors were mitotic activity and cellular pleomorphism. Unlike glioblastomas, however, they did not demonstrate necrosis or vascular proliferation.
Radiographic features
CT
CT appearances were intermediate, appearing as regions of low attenuation with positive mass effect. Enhancement was variable.
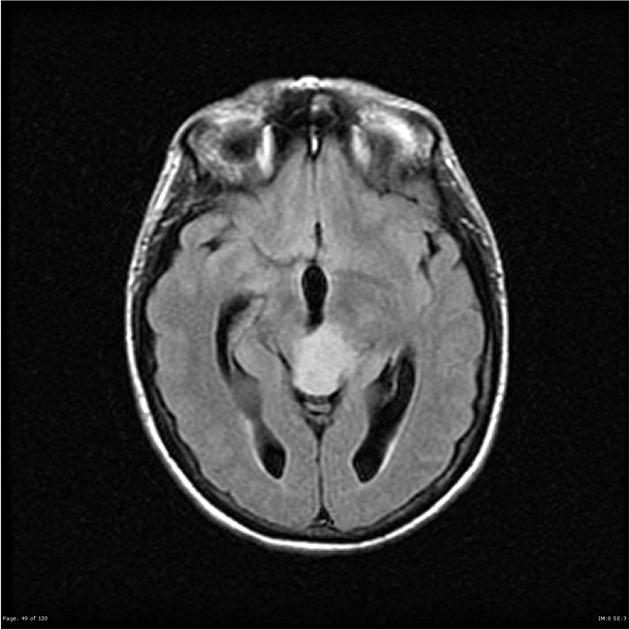
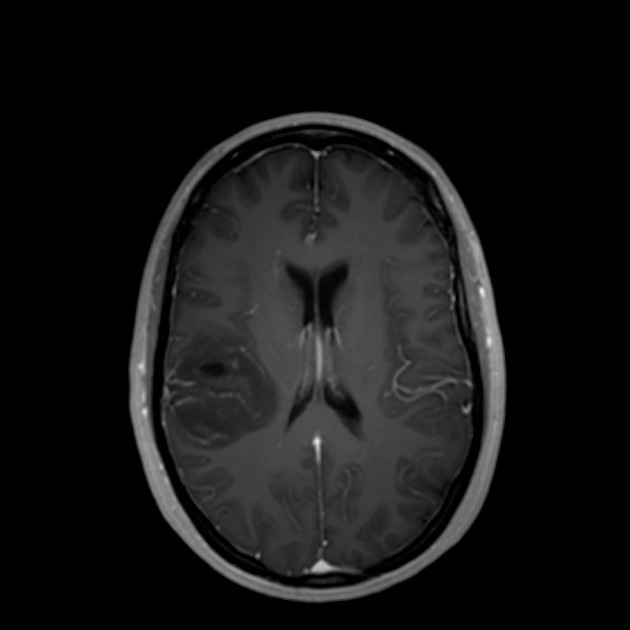
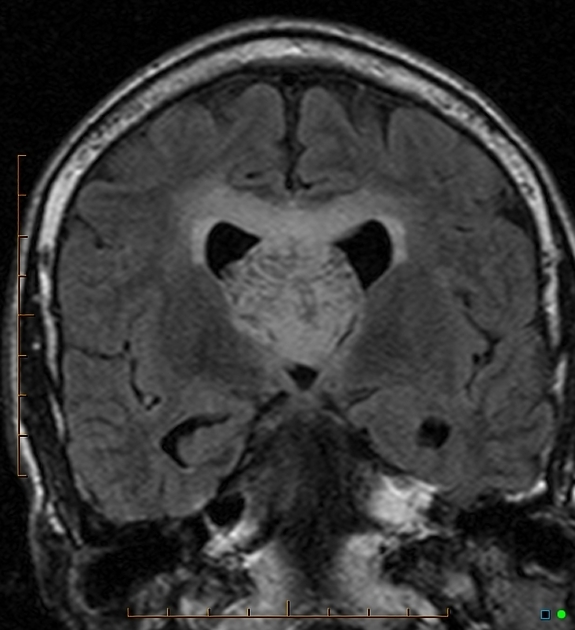
MRI
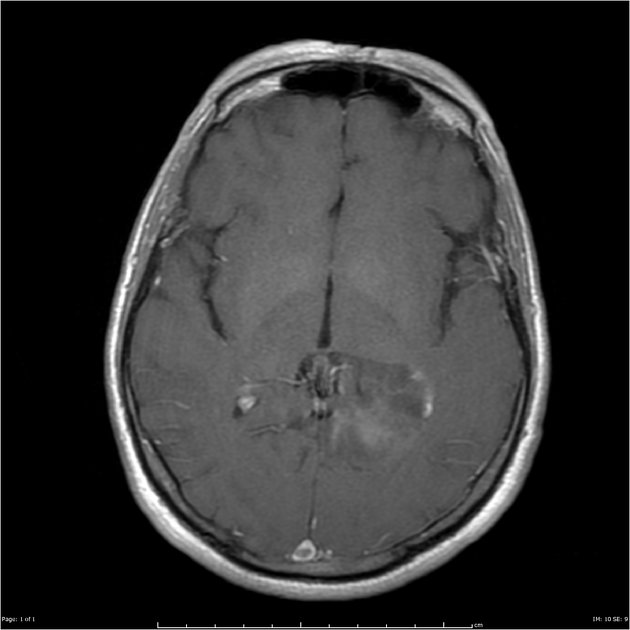
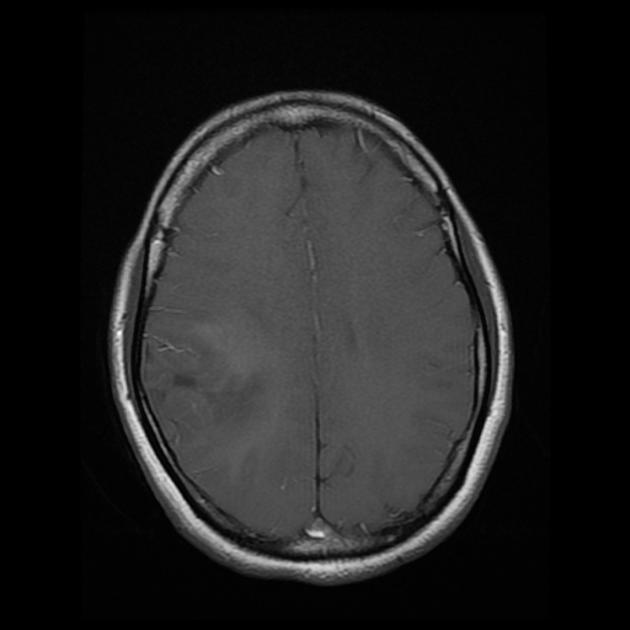
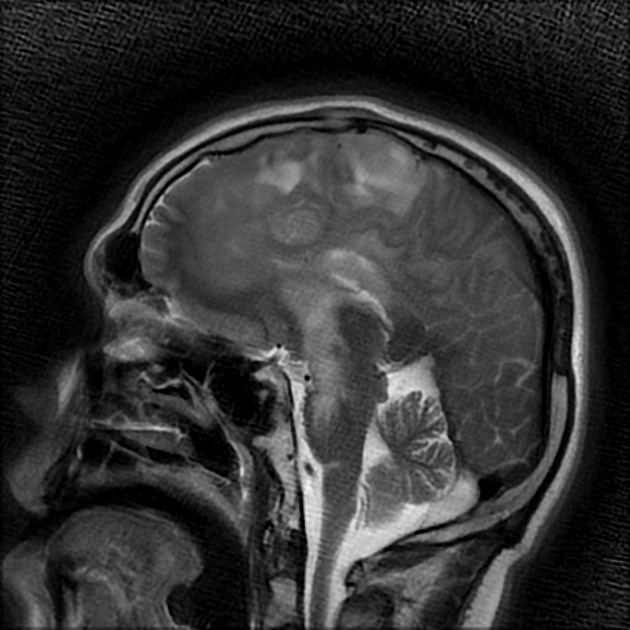
Anaplastic astrocytomas appeared similar to low-grade astrocytomas but were more variable in appearance.
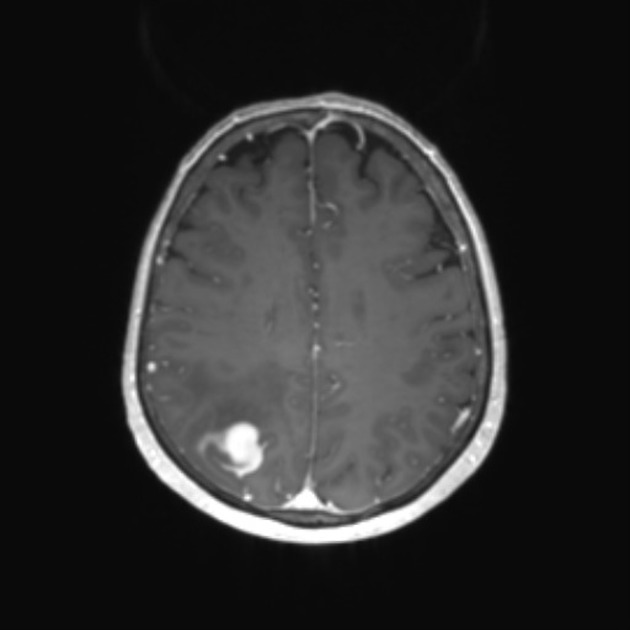
The key to distinguishing anaplastic astrocytomas from low-grade tumors was the presence of enhancement which should generally be absent in the latter 1.
Unlike glioblastomas, anaplastic astrocytomas lacked frank necrosis 1.
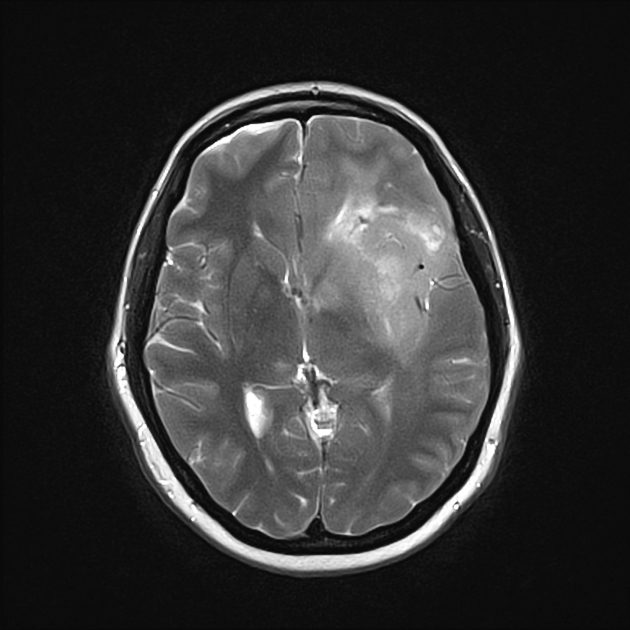
T1: hypointense compared to white matter
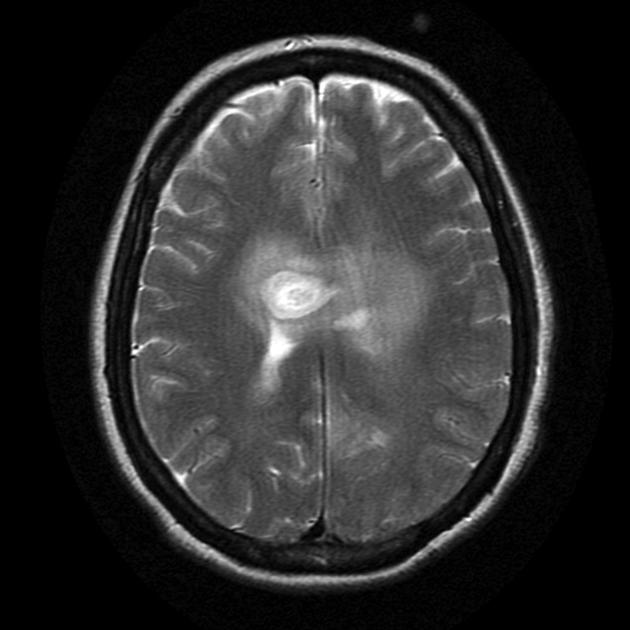
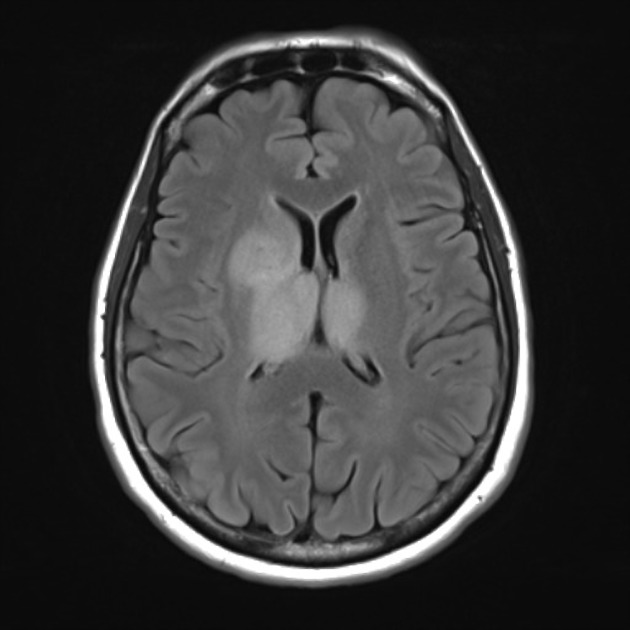
T2: generally hyperintense but can be heterogeneous in cases with blood calcification
T2-FLAIR: relative hypointensity of most of the tumor except a hyperintense rim (T2-FLAIR mismatch sign)
-
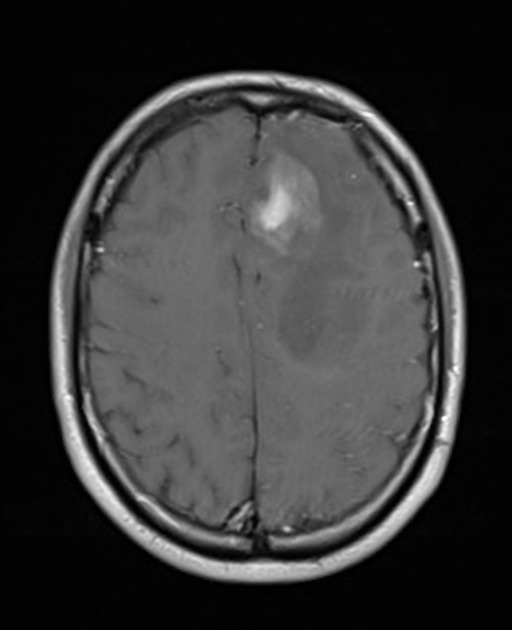
T1 C+ (Gd)
very variable but usually at least some enhancement was present
presence of ring enhancement suggested central necrosis and thus glioblastoma rather than anaplastic astrocytoma
-
MR spectroscopy
increased choline-to-creatine ratio
NAA preserved or mildly depressed
no significant lactate
intermediate levels of myo-inositol (lower than low grade, but higher than GBM) 2
MR perfusion: elevated cerebral blood volume
Treatment and prognosis
Compared to glioblastomas, there were relatively few trials looking at treatment regimens for anaplastic astrocytoma 3. General principles were the same, however, with surgical resection when possible being the treatment of choice with or without subsequent radiotherapy and/or chemotherapy. This depends on the treating clinician's preference, the degree of resection, patient demographics and whether or not the tumor has recurred.
As is the case with everything about anaplastic astrocytomas, the prognosis was also intermediate between low-grade astrocytomas and glioblastomas. Typically patients succumbed to their tumor in 2-3 years, often with transformation into a glioblastoma 4.
Differential diagnosis
The differential, given the heterogeneous and variable appearance of these tumors, was relatively wide and included:
-
other astrocytomas
-
no enhancement (except gemistocytic variant)
more homogeneous
higher myo-inositol on MRS
younger age
-
prominent enhancement with areas of non-enhancement (necrosis)
older age group
depleted NAA
absent myo-inositol
-
-
often multiple
located at grey-white matter junction
absent NAA, absent myo-inositol
ring enhancement
older age group
-
subacute cerebral infarct
gyriform enhancement
vascular territory
-
open ring enhancement




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.