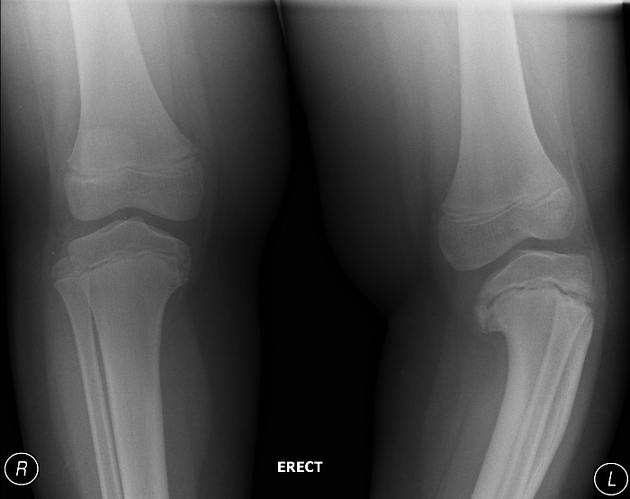
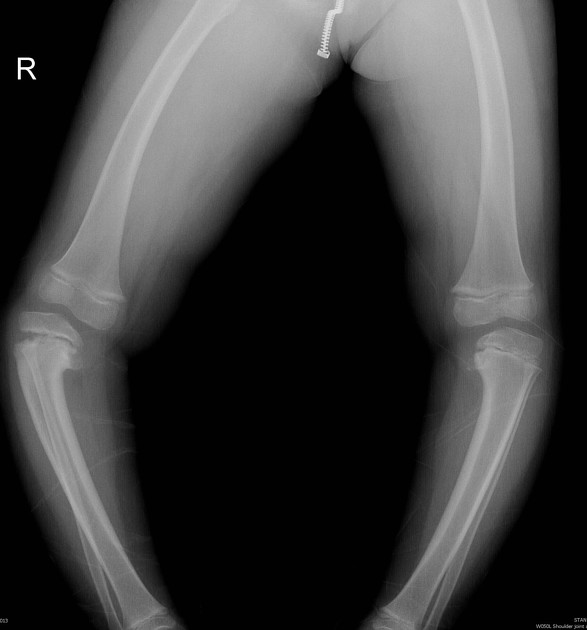
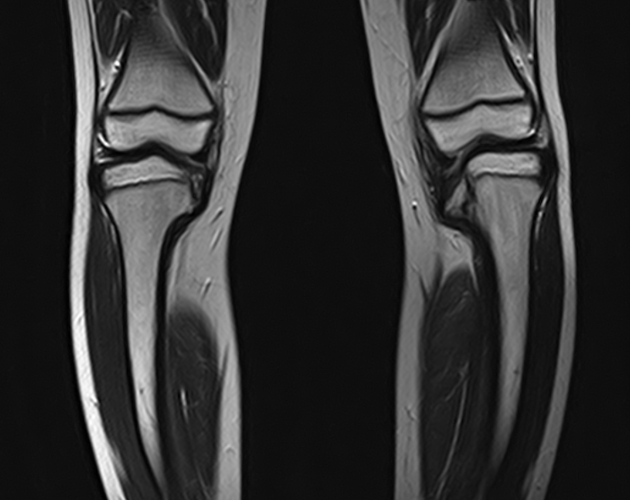
Blount disease refers to a local disturbance of growth of the medial aspect of the proximal tibial metaphysis and/or epiphysis that results in tibia vara. The condition is commonly bilateral. Somewhat confusingly, "tibia vara" has been used in the literature as a synonym for Blount disease.
On this page:
Epidemiology
Infantile Blount has male prevalence and is bilateral in up to 80% of cases 7.
Adolescent Blount is more likely unilateral and found to be associated with childhood obesity, among children of African and Scandinavian ancestry 4,7.
Clinical presentation
Clinically, the child often presents with leg bowing (tibia vara) with little or no associated pain.
Pathology
A relative lack of growth of the medial proximal tibial physis occurs, likely secondary to an increase in compressive forces on the proximal tibial physis from excessive overload at the posteromedial proximal tibial epiphysis and increased shear stress at the physis 5.
Subtypes
There are infantile, juvenile and adolescent forms. The infantile type is 5x more frequent than the others and is seen particularly in early walkers. It appears to be the result of abnormal compressive forces inhibiting growth at the medial growth plate and not from osteonecrosis.
The adolescent type occurs in older overweight children and is a milder disease. It is often unilateral and post-traumatic.
Classification
The condition can be classified into six stages according to the Langenskiold classification 2.
Genetics
There is no recognized inheritance pattern.
Radiographic features
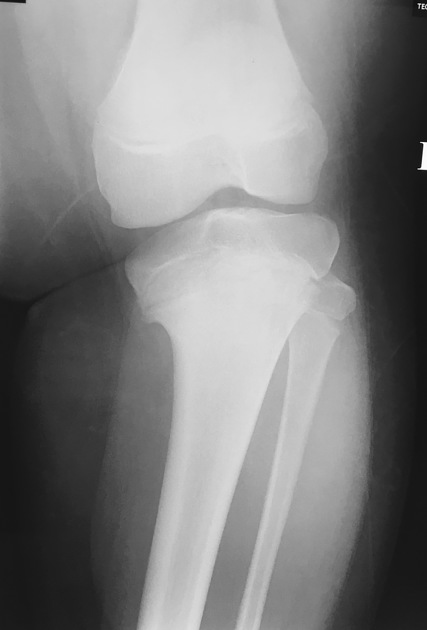
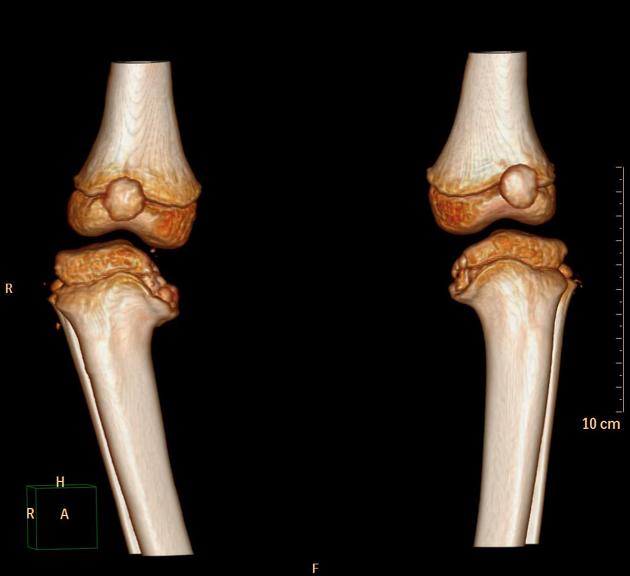
The tibial shaft is in the varus position, and the epiphysis is wedge-shaped, fragmented or can appear absent. The adjacent metaphysis is also depressed and has a beak-like protuberance of rarified bone oriented medially. This causes the metaphyseal-diaphyseal angle of Drennan to increase (typically more than 11º). The lateral cortical wall of the upper tibial metaphysis remains notably straight.
Pre-operative MRI can be used to detect physeal bone bars.
Treatment and prognosis
Treatment depends on the subtype and stage. As a general rule:
infantile or early stage: often conservatively managed
adolescent or late stage: a proximal tibial osteotomy is often considered
History and etymology
It was first described by Walter Putnam Blount (1900-1992), an American pediatric orthopedic surgeon, in 1932. He initially called it "osteochondrosis deformans tibiae" 6.
Differential diagnosis
Differentiation Points:
-
Blount's Disease:
Medial beaking and slanting of the proximal tibial metaphysis.
Irregularity and wedging of the medial epiphysis.
Lateral bowing of the tibia (varus deformity).
Growth plate slanted medially.
-
Scurvy:
Dense white line at the metaphysis (White line of Frankel).
Lucent zone below the white line (Trummerfeld zone).
Pelkan spurs (metaphyseal spurs from fractures).
Subperiosteal hemorrhages.
Generalized osteopenia.
Scorbutic rosary (sharp costochondral junctions).
-
Rickets:
Widening, fraying, and cupping of metaphyses.
Generalized osteopenia.
Rachitic rosary (bulging, rounded costochondral junctions).
Bowing of long bones.
-
Other Pathologies:
Infections: Periosteal reaction and bone destruction.
Osteogenesis Imperfecta: Diffuse osteopenia and multiple fractures.
Congenital Disorders: Variable metaphyseal and epiphyseal deformities specific to the condition.
For leg bowing consider: differential for leg bowing in children.















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.