Hydatid cyst, also known as echinococcosis, results from infection by the Echinococcus tapeworm species. It primarily includes two significant zoonotic diseases caused by tapeworms: cystic echinococcosis, resulting from Echinococcus granulosus, and alveolar echinococcosis, resulting from Echinococcus alveolaris/multilocularis 1,2.
On this page:
Epidemiology
The prevalence and primary endemic regions of alveolar echinococcosis and cystic echinococcosis differ:
cystic echinococcosis is more common and has a worldwide geographical distribution. Highly endemic areas for cystic echinococcosis include western China, Central Asia, South America, Mediterranean countries, and East Africa6,12.
alveolar echinococcosis is less common than cystic echinococcosis and is predominantly endemic in the northern hemisphere, particularly in North America, west-central Europe, the Near East, Siberia, Central Asia, Japan, and China12.
Pathology
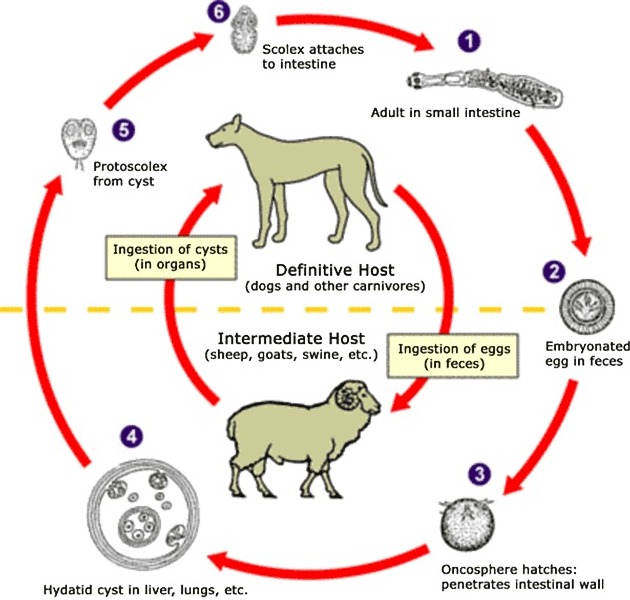
Echinococcosis is caused by the larvae of tapeworms (cestodes) of the genus Echinococcus (family Taeniidae).
The primary host is the dog or wolf for Echinococcus granulosus and the fox for Echinococcus alveolaris/multilocularis.
Echinococcosis in humans is primarily caused by the accidental ingestion of Echinococcus larvae. Humans act as incidental hosts3.
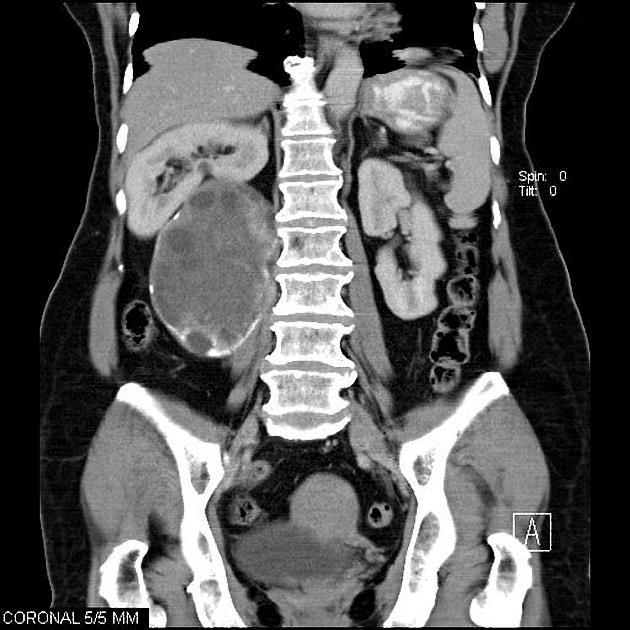
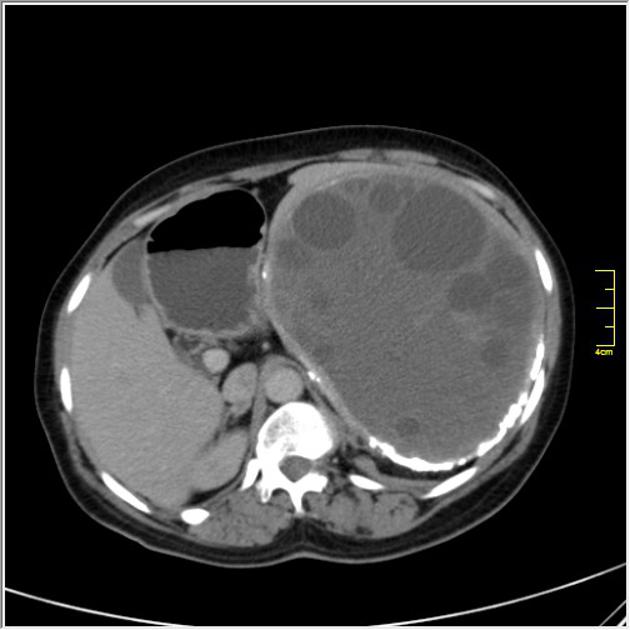
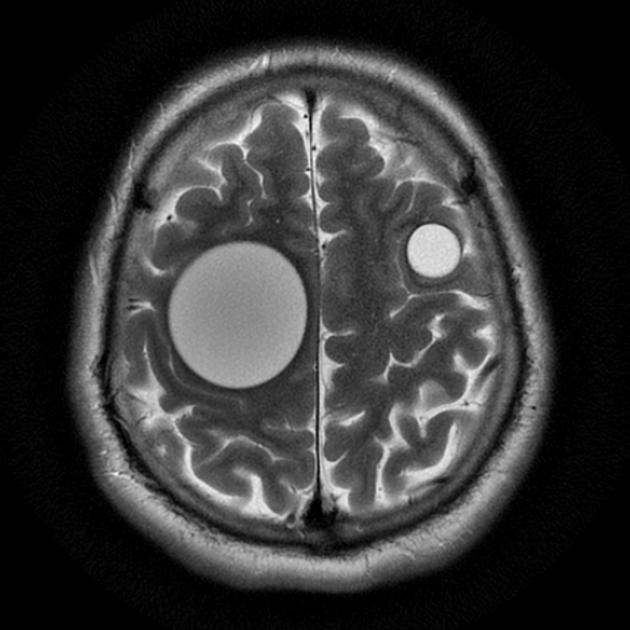
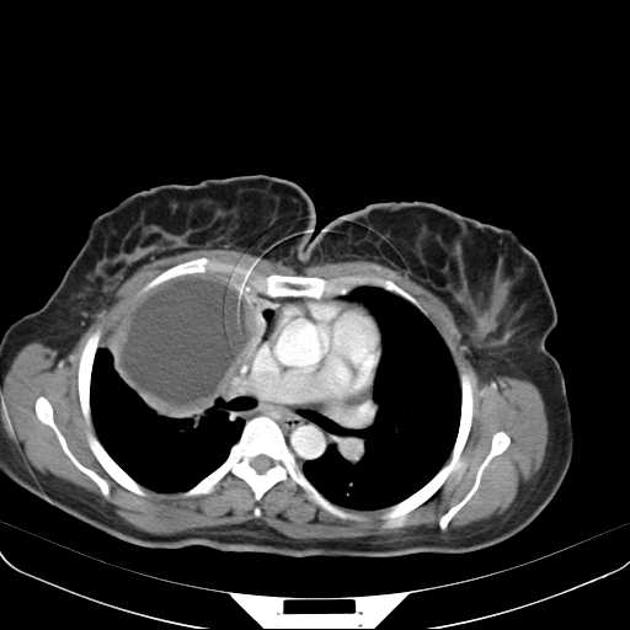
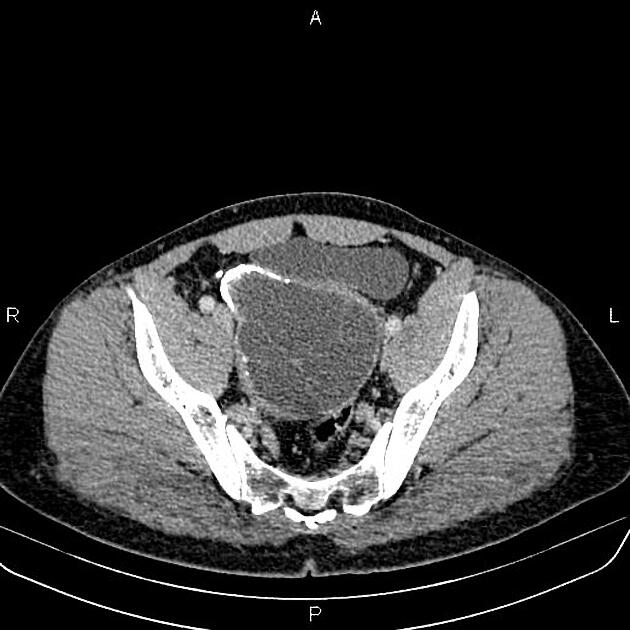
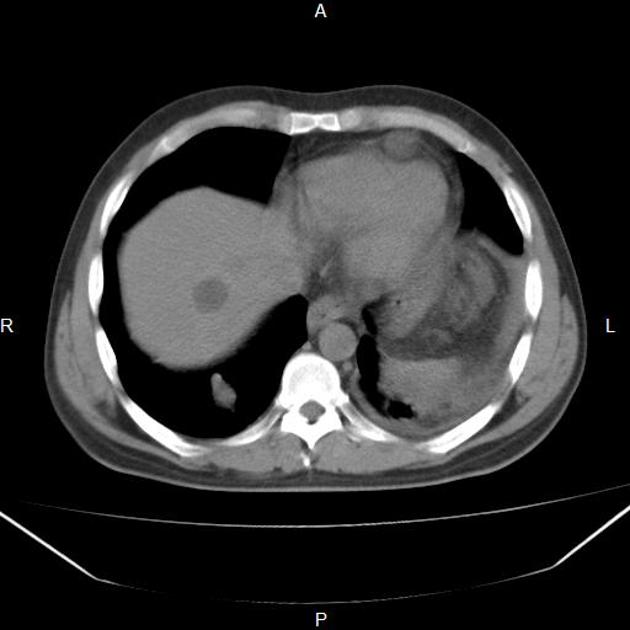
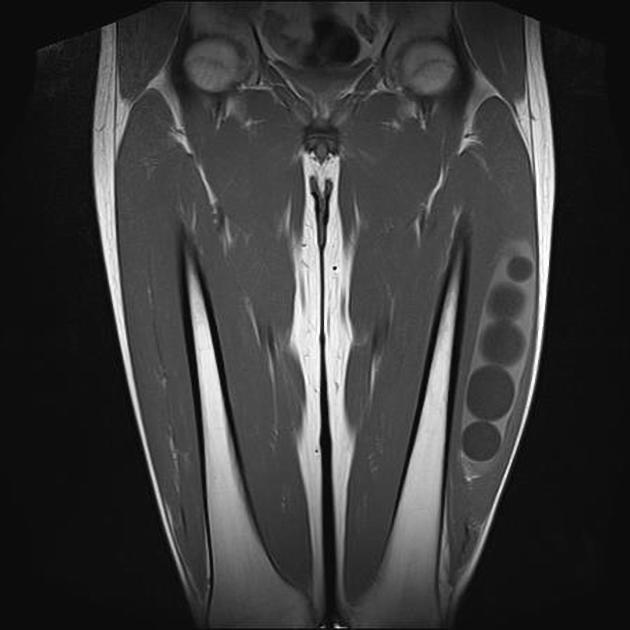
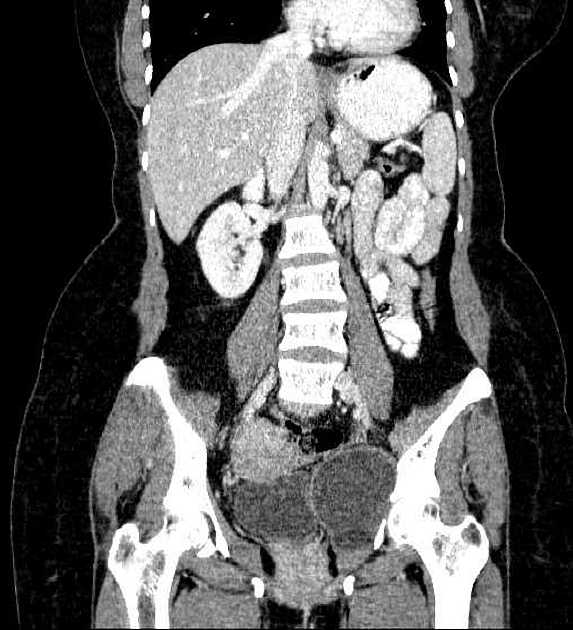
Location
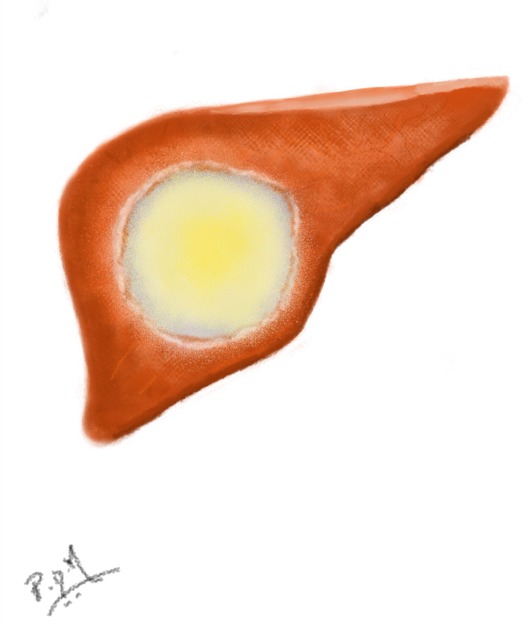
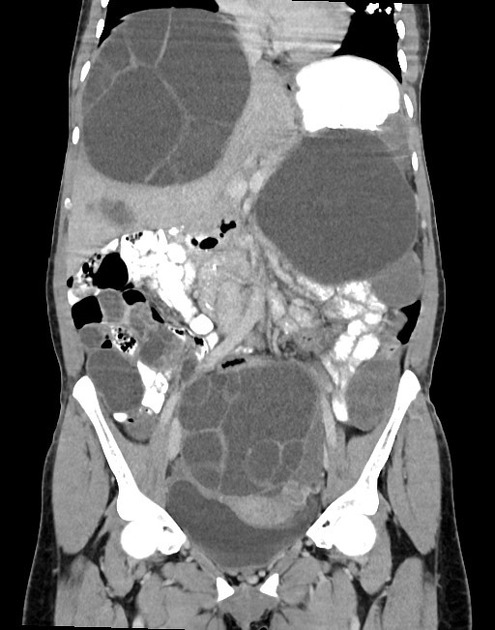
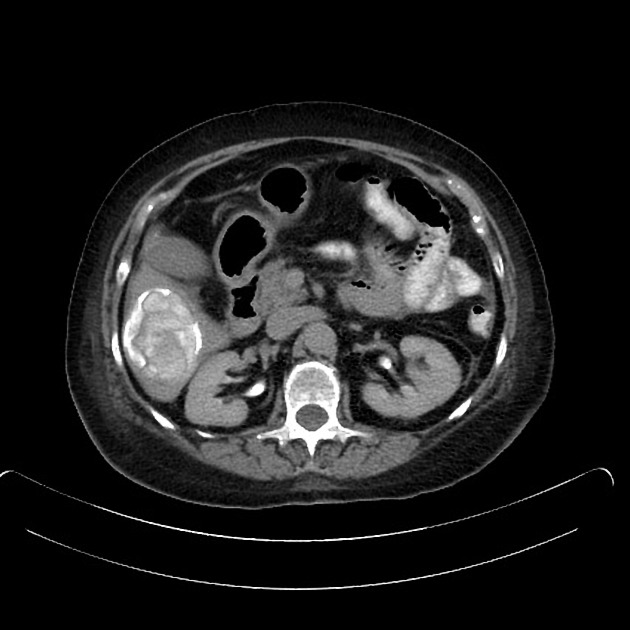
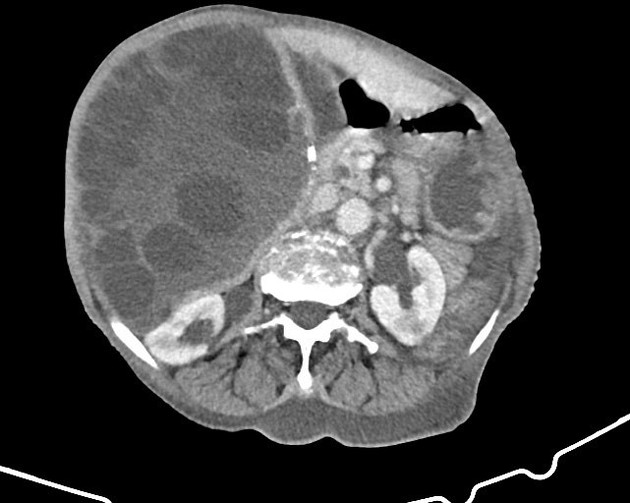
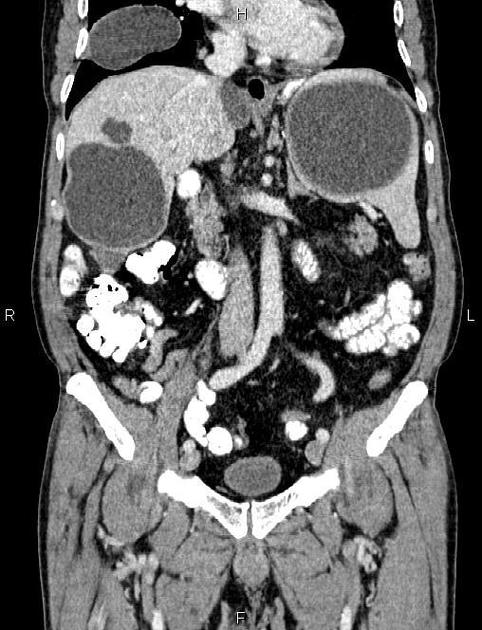
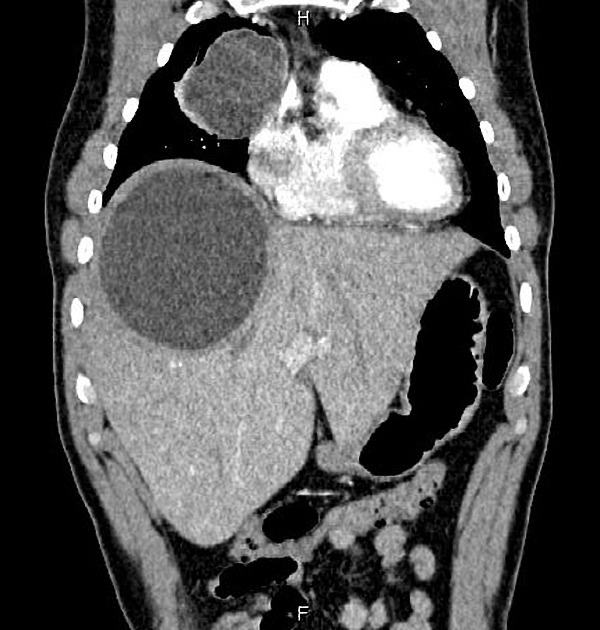
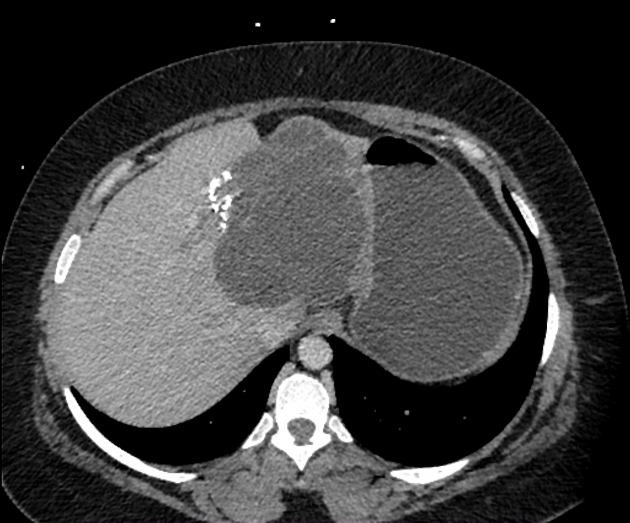
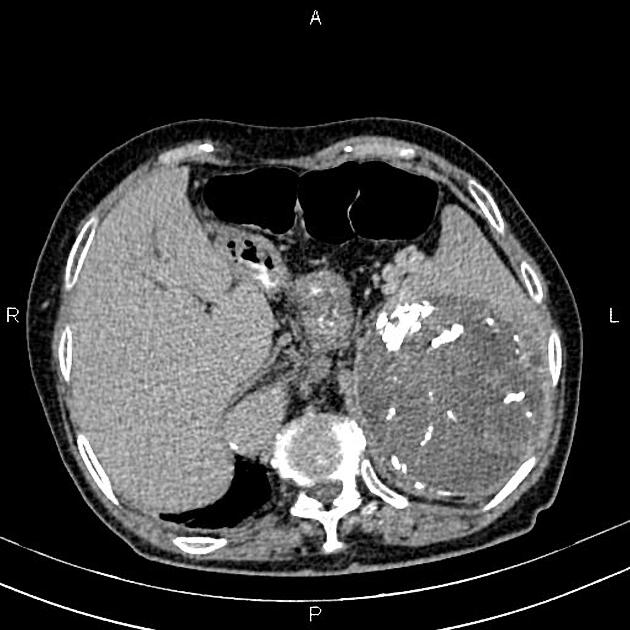
hepatic hydatid infection: most common organ (76% of cases) 1,5
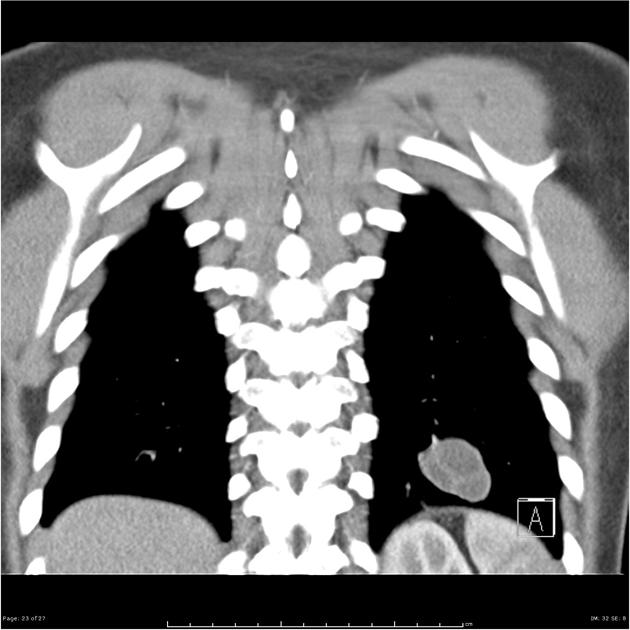
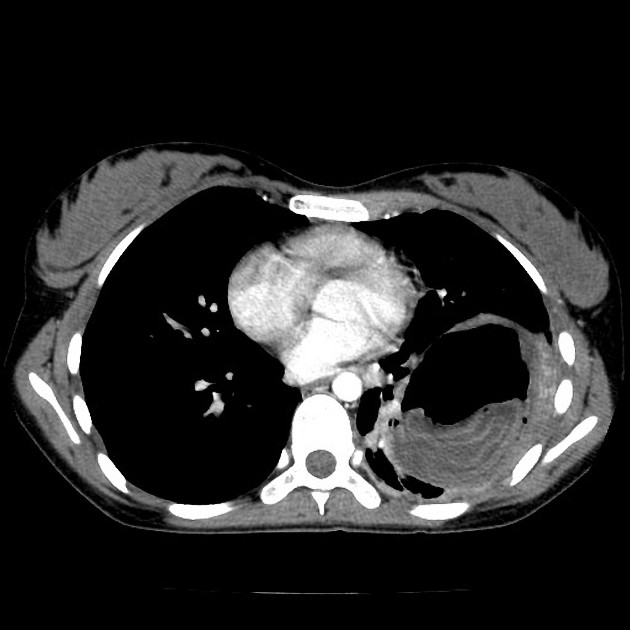
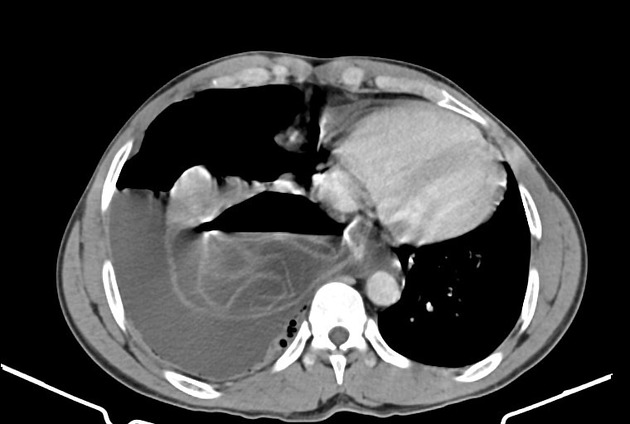
pulmonary hydatid infection: second most common organ (15% of cases)
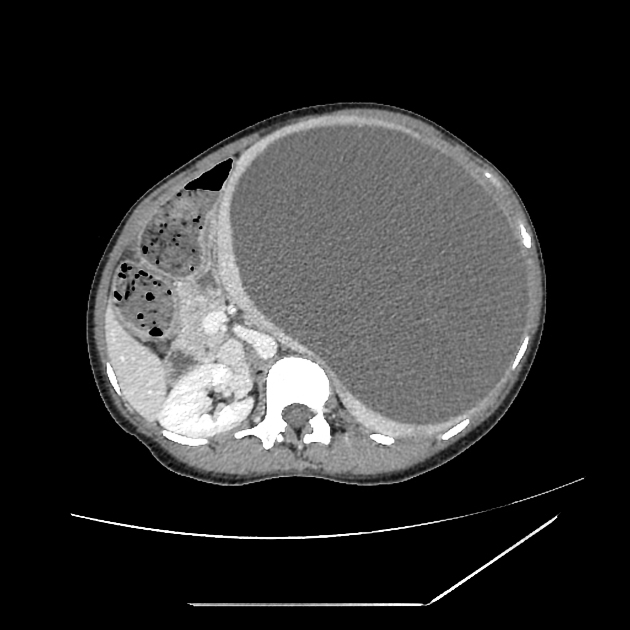
splenic hydatid infection: third most common organ (5% of cases) 8
mediastinal hydatid infection (very rare) 9
Cyst structure
The cysts usually have three components 1,2,10,11:
pericyst: dense fibrous capsule produced by the host
exocyst (laminated membrane): semi-permeable acellular mucin-based membrane produced by the parasite
endocyst: germinal layer of the parasite, which produces daughter cysts containing protoscolices (larval parasite) on its internal surface and laminated membrane on its outer surface
Cyst classification
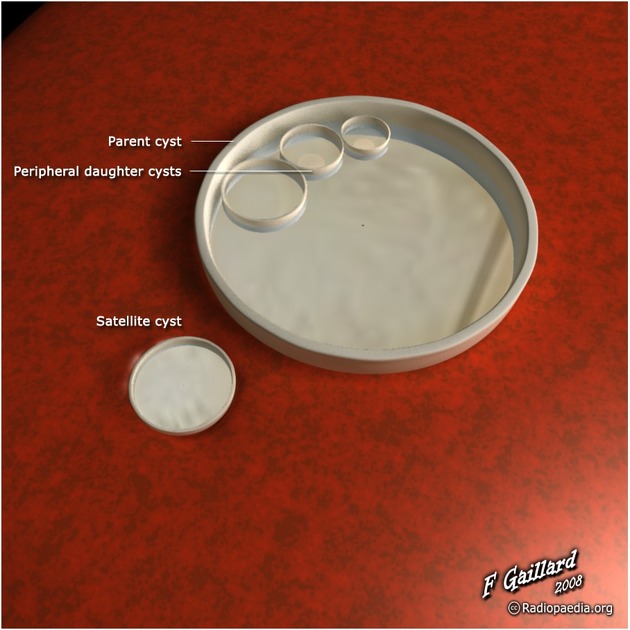
Based on morphology the cyst can be classified into four different types 2:
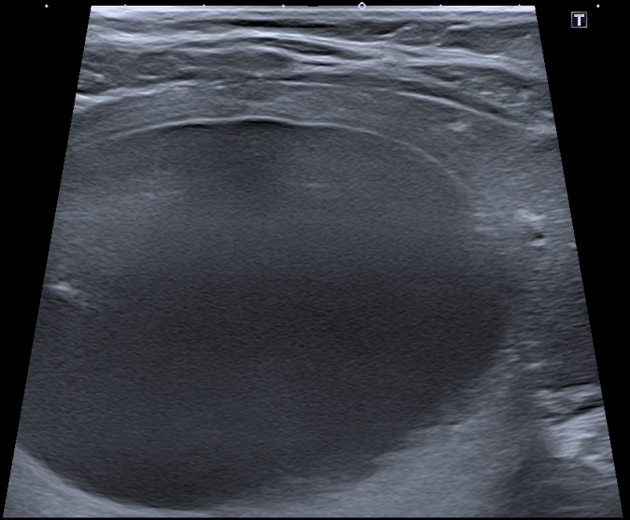
type I: simple cyst with no internal architecture
-
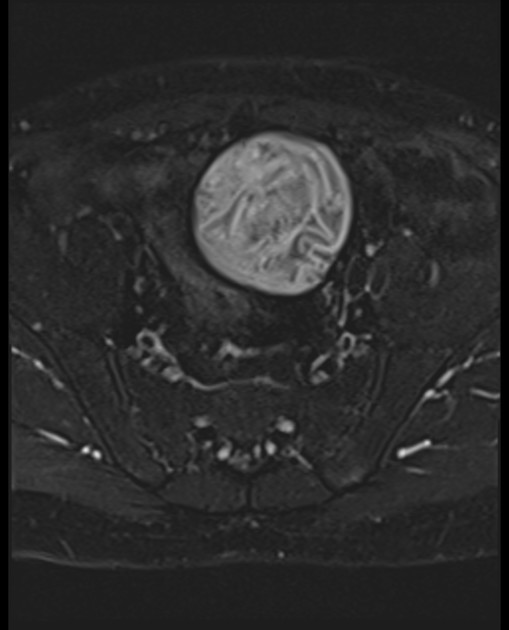
type II: cyst with daughter cyst(s) and matrix
type IIa: round daughter cysts at the periphery
type IIb: larger, irregularly shaped daughter cysts occupying almost the entire volume of the mother cyst
type IIc: oval masses with scattered calcifications and occasional daughter cysts
type III: calcified cyst (dead cyst)
type IV: complicated cyst, e.g. ruptured cyst
Markers
Radiographic features
A chest film or other plain films can be the first diagnostic modality when echinococcosis is suspected, depending on clinical indications.
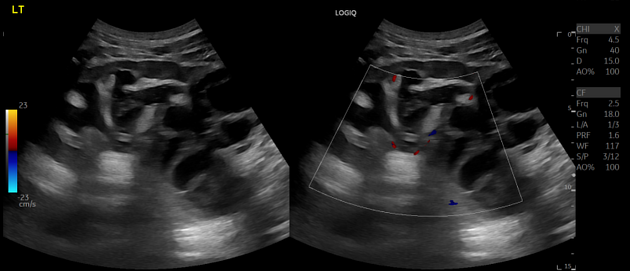
Ultrasound is commonly used to classify hepatic hydatid disease using either the Gharbi classification 4 or the WHO-IWGE classification.
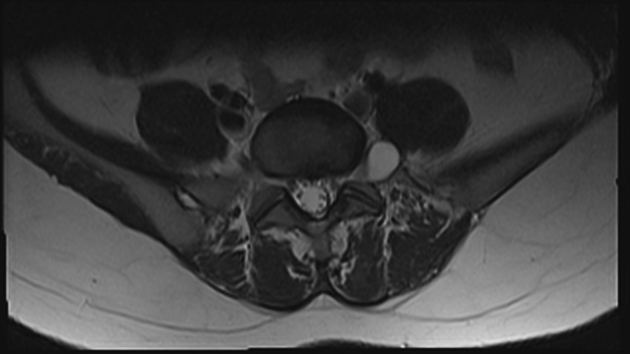
CT and MRI imaging are indicated when considering surgical treatment, particularly in regions like the brain, spine, and locations inaccessible for conventional radiography or ultrasound, or in case of diagnostic uncertainty.
Ultrasound
The Gharbi ultrasound classification consists of five stages 4:
stage 1: homogeneously hypoechogenic cystic thin-walled lesion
stage 2: septated cystic lesion
stage 3: cystic lesion with daughter lesions
stage 4: pseudo-tumor lesion
stage 5: calcified or partially calcified lesion (inactive cyst)
Treatment and prognosis
Four treatment options are available 7:
surgical excision
PAIR (puncture, aspiration, injection of protoscolicidal agent and reaspiration)
chemotherapy with an anti-helminthic agent (albendazole, mebendazole)
watch and wait for inactive and silent cysts
Treatment outcomes were improved when surgery or PAIR was combined with benzimidazole given before and after surgery 7. Regarding medical management, higher scolicidal and anti-cystic activity was seen in combination therapy with albendazole plus praziquantel and was more likely to result in cure or improvement 7.

































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.