Juvenile nasopharyngeal angiofibromas are a rare benign, but locally aggressive, vascular tumors that occur almost exclusively in young men; usually between the ages of 10 and 18.
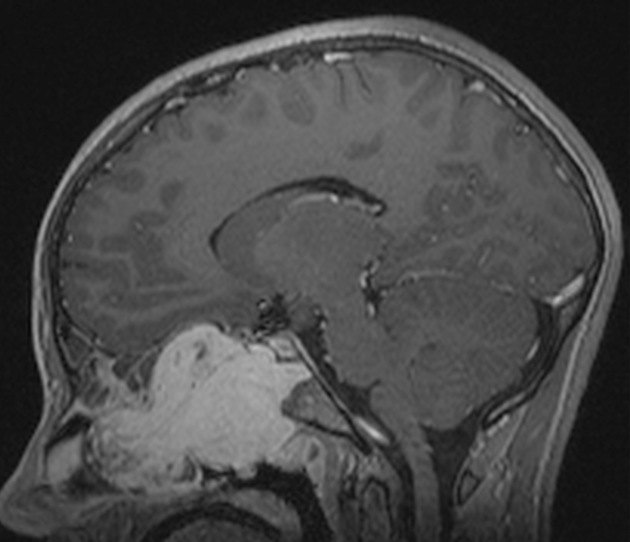
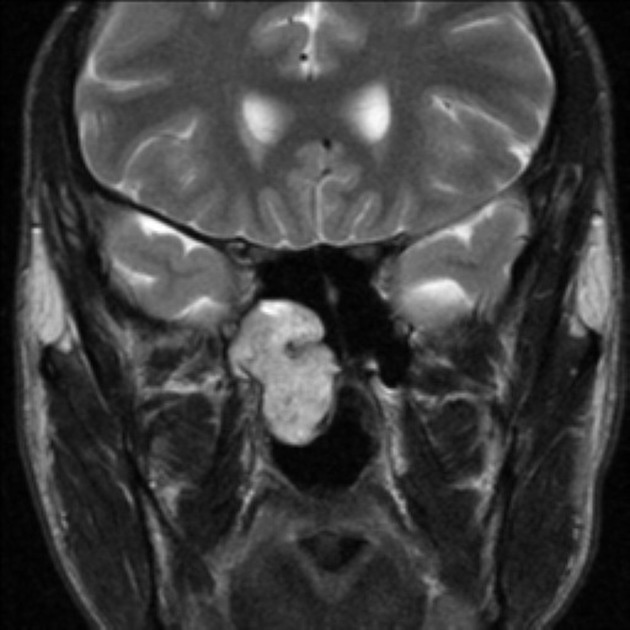
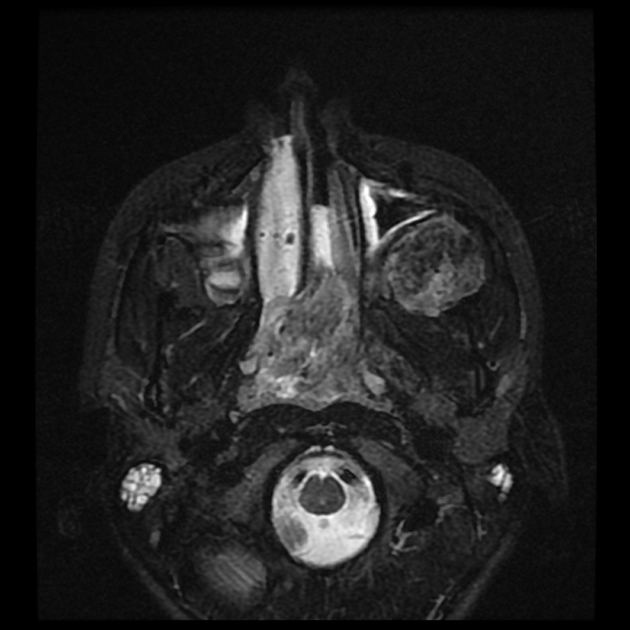
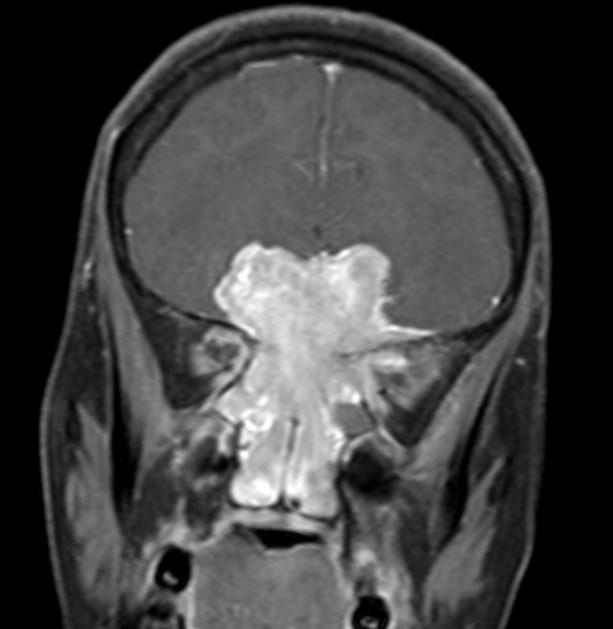
On imaging, they present as vividly enhancing soft-tissue masses centered on the sphenopalatine foramen. Given its vascularity, prominent flow voids are seen on MRI leading to a salt and pepper appearance.
On this page:
Epidemiology
Juvenile nasopharyngeal angiofibromas occur almost exclusively in males and usually in adolescence (~15 years) 16. They account for only 0.5% of all head and neck tumors 2 but are the most common of the benign nasopharyngeal neoplasms ref.
Associations
red hair and fair skin in White patients 14,15
familial adenomatous polyposis (rare) 11-13
Clinical presentation
The presentation is typical with obstructive symptoms, epistaxis, and chronic otomastoiditis due to obstruction of the Eustachian tube. Patients may present with life-threatening epistaxis. On examination, it may be seen as a pale reddish-blue mass. It is, as the name suggests, very vascular and a biopsy can sometimes be fatal.
Pathology
Juvenile nasopharyngeal angiofibromas are benign but highly vascular tumors which may be locally aggressive. The tumors express androgen receptors 17,18, which may explain their growth during puberty, regression after puberty or with estrogen administration, and occurring almost exclusively in males 15,16.
The exact site of origin is contentious as these masses usually present when they have reached a considerable size. However, most authors agree that they arise from the posterior choanal tissues in the region of the sphenopalatine foramen.
Staging
See staging of juvenile nasopharyngeal angiofibromas.
Radiographic features
Imaging plays an important role in diagnosis, as well as staging, as biopsies should be avoided due to the risk of brisk hemorrhage, due to the tumor's vascular nature.
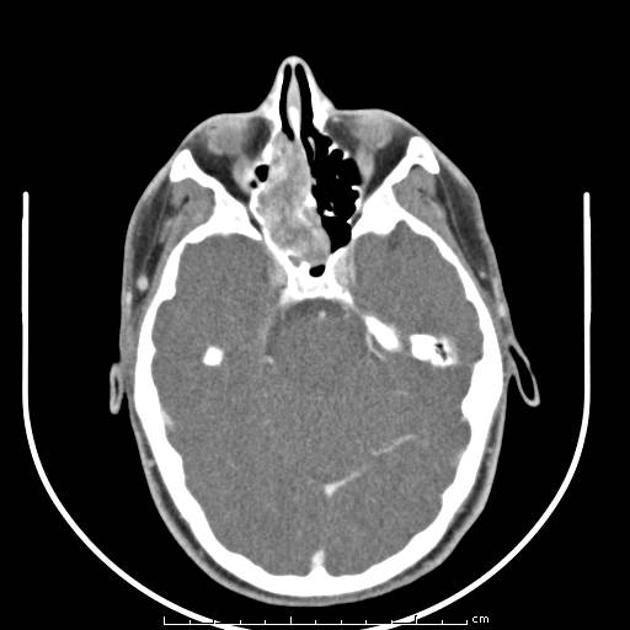
Although these masses are thought to arise from the region of the sphenopalatine foramen, they are usually sizable at diagnosis, frequently with extension medially into the nasopharynx, laterally into the pterygopalatine fossa and, over time, beyond into the orbit, paranasal sinuses, intracranial cavity and infratemporal fossa.
Plain radiograph
Plain radiographs no longer play a role in the workup of a suspected juvenile nasopharyngeal angiofibroma; however, they may still be obtained in some instances during the assessment of nasal obstruction or symptoms of sinus obstructions. Findings include 3:
visualization of a nasopharyngeal mass
opacification of the sphenoid sinus
anterior bowing of the posterior wall of the maxillary antrum (Holman-Miller sign) 7
widening of the pterygomaxillary fissure and pterygopalatine fossa
erosion of the medial pterygoid plate
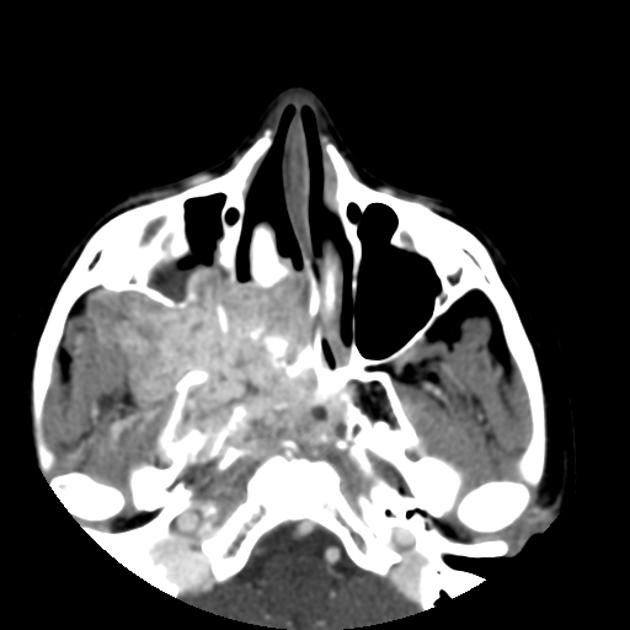
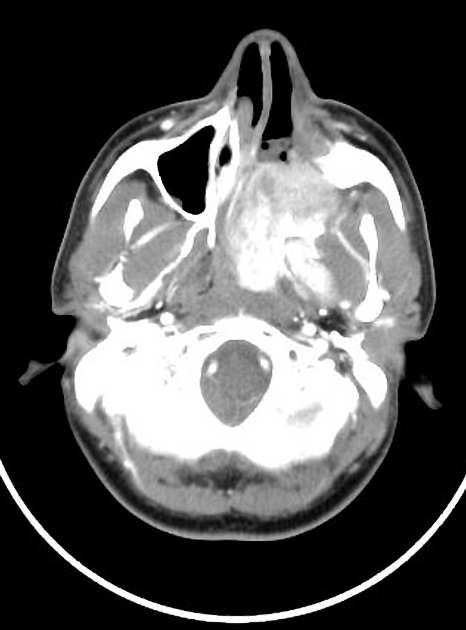
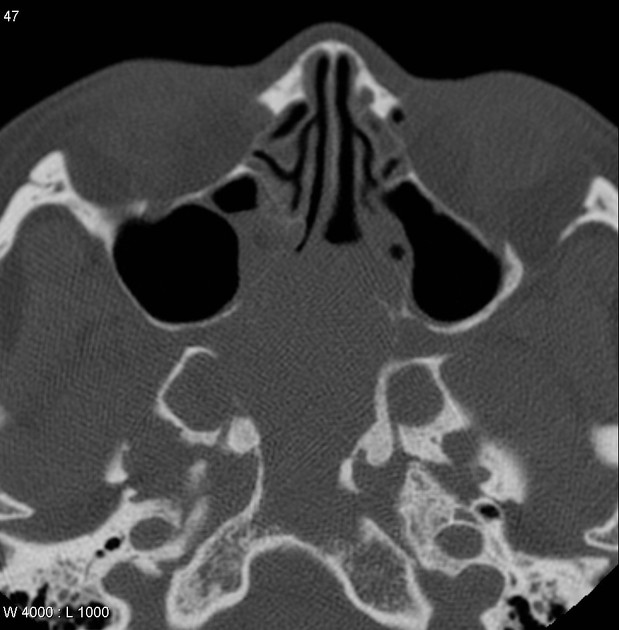
CT
CT is particularly useful at delineating bony changes. Findings are similar to those described above. Typically a lobulated non-encapsulated soft tissue mass is demonstrated centered on the sphenopalatine foramen (which is often widened) and usually bowing the posterior wall of the maxillary antrum anteriorly. There is marked contrast enhancement following administration of contrast, reflecting the prominent vascularity.
Extensive bony destruction is usually not a feature; bone is rather remodeled or resorbed. This feature may be helpful in differentiation from other, more aggressive, lesions. Intracranial extension can, however, occur.
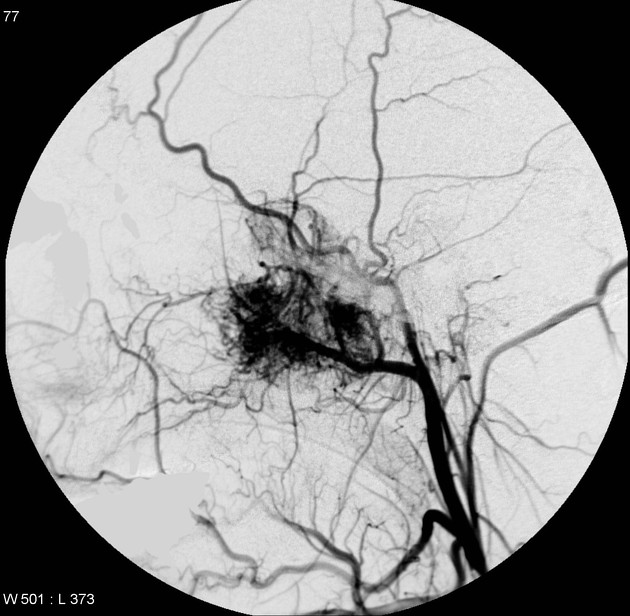
Angiography (DSA)
Angiography, although not essential, is often useful in both defining the feeding vessels and in preoperative embolization. Supply of these tumors is usually via 3:
-
external carotid artery: the majority
palatine arteries
-
internal carotid artery: less common, usually in larger tumors
sphenoidal branches
Of note, enlargement of feeding vessels is not a common finding 6.
MRI
MRI is excellent at evaluating tumor extension into the orbit and intracranial compartments.
T1: intermediate signal
T2: heterogeneous signal: flow voids appear dark
T1 C+ (Gd): shows prominent enhancement
The presence of prominent flow voids leads to a salt and pepper appearance on most sequences and are characteristic 5,6.
Treatment and prognosis
Surgical resection (either open or, increasingly, endoscopic) is the treatment of choice, usually performed after preoperative embolization to help with hemostasis. The embolization may be performed up to five days prior to surgery. Irradiation may be an option if surgery is not possible or only incomplete resection has been achieved 2,4,6.
In cases where there is skull base involvement, a high recurrence rate (up to 50%) has been reported 2,4.
Differential diagnosis
Imaging differential considerations include:
angiomatous polyp: variant of a sinonasal polyp, located toward ostium/hardly extend to the nasopharynx, elderly age, less vascularity
lymphangioma: no contrast enhancement
encephalocele: no contrast enhancement






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.