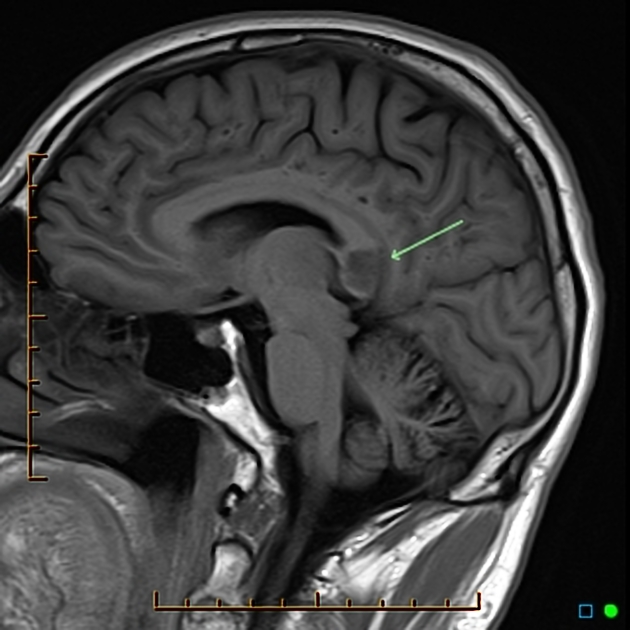
Lesions of the corpus callosum are uncommon and arise from multiple different etiologies. The lesions can be classified according to underlying pathophysiology 4-6.
Neoplasm
Typically, amongst neoplasms, only aggressive lesions can invade the corpus callosum as it is composed of very dense white matter tracts which act as a barrier to tumor spreading 1.
meningioma: secondary involvement from primary falx lesion
metastasis: rare, mainly from contiguous extension of lesion adjacent to corpus callosum
Vascular
aneurysm: can occasionally rupture into the corpus callosum
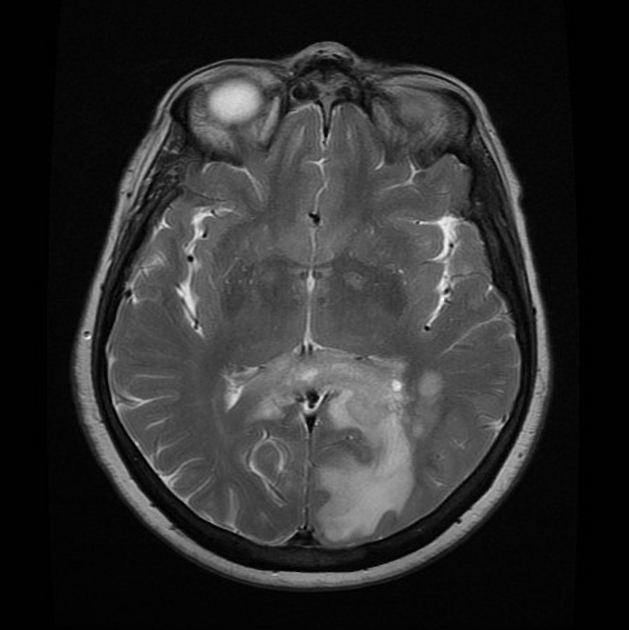
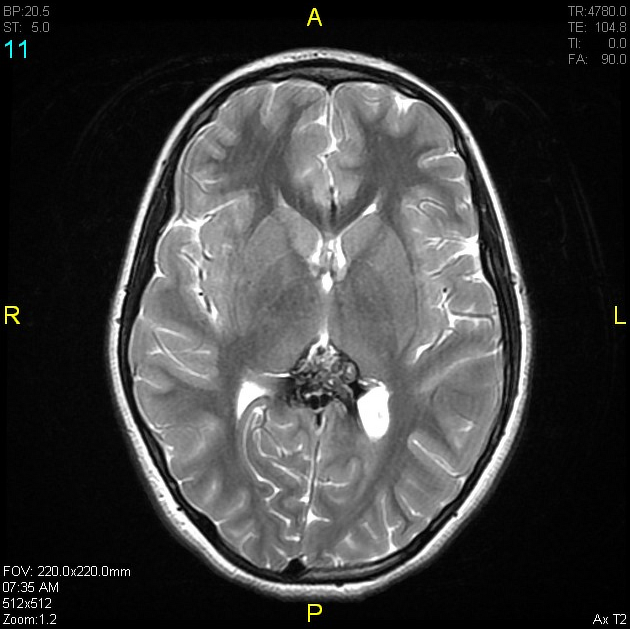
arteriovenous malformation: arising around the corpus callosum
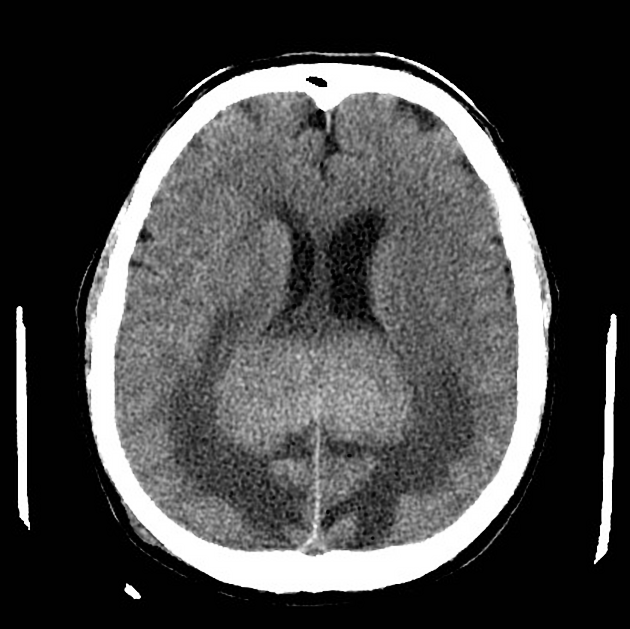
cavernous malformation (cavernoma)
-
gliosis: secondary to small vessel chronic ischemia, subcortical arteriosclerotic encephalopathy, radiation therapy and normal aging 11; histologically corresponds to subependymal gliosis
the subependymal splenium is typically affected with normal aging and after radiation therapy 11
hypoxic-ischemic encephalopathy: corpus callosum only involved in severe or advanced case
infarction: rare because of extensive collateral vascular supply, most often seen with emboli, major ischemic stroke, subfalcine herniation with mass effect and vasculitides 3
Infection
aspergillosis: can involve corpus callosum 7
transient lesions of the splenium: many underlying etiologies including infectious agents
subacute sclerosing panencephalitis: can involve the corpus callosum in advanced stages 8
tuberculosis: callosal tuberculomas have been reported, although rare 9
Demyelination
Marchiafava-Bignami disease: demyelination and necrosis, can appear as cystic lesions
Leukodystrophy
Congenital
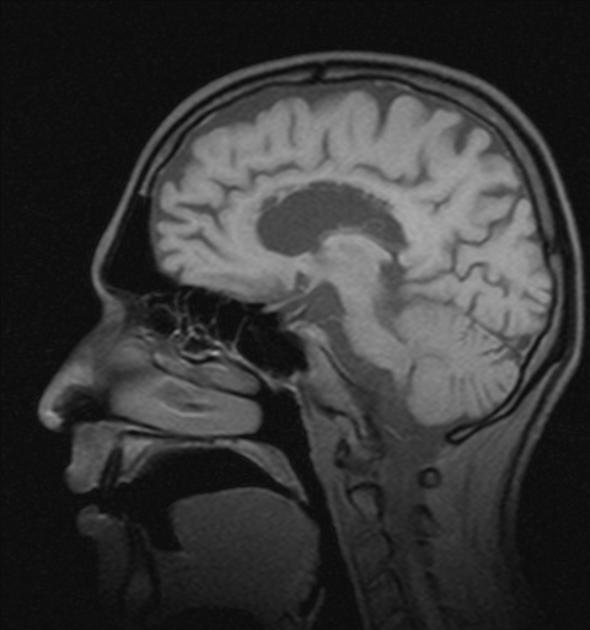
tubonodular pericallosal lipoma: associated with dysgenesis of the corpus callosum
Trauma
Other
cytotoxic lesions of the corpus callosum (CLOCCs): many underlying etiologies
posterior reversible encephalopathy syndrome (PRES): callosal involvement seen in up to 10% of patients, usually with associated parieto-occipital T2-hyperintensities 10
post shunt decompression: after placement of ventriculostomy in patients with chronic hydrocephalus





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.