Percutaneous liver biopsy, utilizing either ultrasound or CT guidance, allows for an accurate and reliable method of acquiring hepatic tissue for histopathological assessment. It is divided into two types:
non-focal or non-targeted liver biopsy (used in the assessment and staging of the parenchymal liver disease, e.g. MASH)
focal or targeted liver biopsy (i.e. directed to a focal parenchymal lesion)
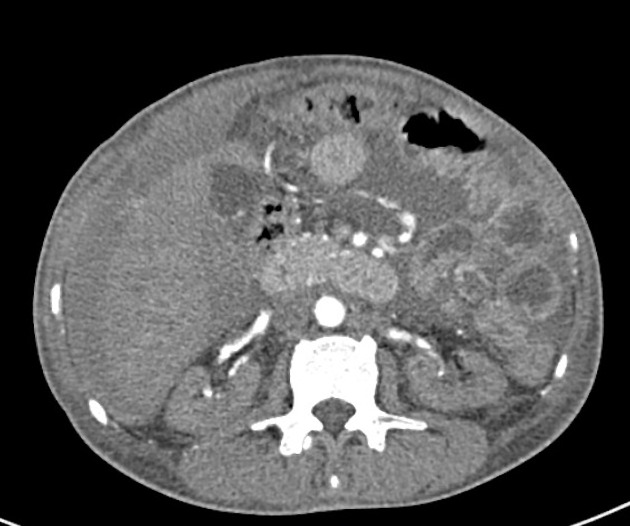
Ultrasound is the modality of choice for imaging guidance in the vast majority of cases, with CT nowadays mostly reserved for a conjoined assessment together with the US in focal/targeted biopsies of lesions not sonographically demonstrated.
An alternative option for percutaneous CT/US guidance, particularly used in patients with coagulopathy and ascites, is the transjugular liver biopsy.
On this page:
Indications
-
non-focal or non-targeted liver biopsy
-
staging of known parenchymal disease
abnormal liver function tests of unknown etiology
-
hepatic storage disorders
assessment of liver transplant rejection
-
-
focal or targeted liver biopsy
undetermined liver lesion
liver metastasis of unknown origin
Contraindications
The contraindications must be considered individually in each case. Overall, the most important contraindications are:
uncooperative patient
uncorrectable bleeding diathesis (abnormal coagulation indices)
-
relative contraindication that can be usually tapped before the biopsy
extrahepatic biliary obstruction 1
Procedure
Laboratory parameters for a safe procedure
Interventional procedures like liver biopsy require special attention to coagulation indices. There are widely divergent opinions about the safe values of these indices for percutaneous biopsies ref. The values suggested below were considered based on literature review, whose references are cited below:
-
complete (full) blood count
platelets >50,000/mm3 (some institutions determine other values between 50,000-100,000/mm3) 2
-
coagulation profile
-
some studies showed that having a normal INR or prothrombin time is no reassurance that the patient will not bleed after the procedure
international normalized ratio (INR) ≤1.5 2
normal prothrombin time (PT) / partial thromboplastin time (PTT)
-
Pre-procedure preparation
written informed consent
assessment of patient's cooperation for the procedure
Equipment
sterile procedure pack
sterile gloves
skin antiseptic
scalpel
-
single or co-axial needle set
calibers vary among institutional protocols and purpose of the biopsy, with commonly used core biopsy calibers being 14G, 16G, and 18G
16G core biopsy needle is recommended by many professional organizations 5
1% lidocaine
midazolam (for sedation): its use varies according to different institutional guidelines, and should always be considered case-by-case
histopathology department pot
Technique
As ultrasound is the most common imaging modality used to guide liver biopsy, that will be the technique approached in this article.
-
pre-procedure assessment of the liver with ultrasound should be performed for planning positioning and needle entrance point
-
supine, oblique, or total left lateral decubitus are the possible positioning of the patient - it is important to make sure that the patient is comfortable and can remain still in that position
wedge behind the patient's back helps for oblique positioning
assess if the procedure will be performed under breath held and practice this with the patient
marking of the entrance point on the skin is advised to aid the skin cleaning and dressing
-
hemodynamic monitoring in place is recommended
a time-out should be performed by this stage
skin site is prepped and draped to ensure asepsis
local anesthetic is infiltrated within the subcutaneous tissues, abdominal wall and down to the liver capsule
entrance point is created with a scalpel (usually number 11 blade)
-
using the freehand technique the needle is advanced under ultrasound guidance during the entire course of the biopsy
the needle tip must always cross the capsule prior to deploying the cutting device 1
documentation of the needle positioning after firing is advised
usually only one pass is required if an adequate sample is obtained but this depends on the reason for biopsy 5
after the procedure, a brief ultrasound examination for perihepatic or intraparenchymal hemorrhage is usually performed
Post-procedure care
Bed-rest is advised as well as regular observations (pulse, blood pressure, and SpO2 in those receiving sedation) depending on risk factors, active questioning of the patient of any pain, and inspection of the biopsy site for bleeding every 30 minutes 5.
The observation period should allow an ample opportunity to identify and treat a potential complication in a timely manner to prevent a serious or catastrophic outcome, this varies with each institution's protocol but is between 3-8 hours 5. Observations should be taken 5:
every 15 minutes for the first hour
every 30 minutes for the next two hours
every hour for the remainder of the observation period
The patient should only be discharged when there are stable observations with no evidence of hemodynamic instability or bleeding and new pain or shortness of breath 5.
Complications
Percutaneous liver biopsy remains a safe procedure.
Complications include:
post-procedure pain: pain radiated to the right shoulder 3
severe hemorrhage: ~1% (range 0.35-1.7%) 1
death related to hemorrhage is uncommon and numbers in the literature are variable, with the most commonly quoted mortality rate being of ≤1 in 10,000 liver biopsies 4






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.