Penetrating atherosclerotic ulcers (PAU) are pathologies that involve the aortic wall and along with aortic dissection and aortic intramural hematoma, form the spectrum of acute aortic syndrome.
On this page:
Epidemiology
Typically, penetrating atherosclerotic ulcers are seen in elderly male patients with a history of hypertension (up to 92%), smoking (up to 77%) and coronary artery disease (up to 46%) as well as chronic obstructive pulmonary disease (24-68%) 1.
Penetrating atherosclerotic ulcers account for ~7.5% (range 2.3-11%) of all cases of acute aortic syndrome 1. In ~50% (range 42-61%) of cases, there are concurrent aortic aneurysms, most often in the abdomen 1.
Clinical presentation
Typically patients present with symptoms of an acute aortic syndrome, namely acute intense chest pain, often described as tearing, ripping, migrating or pulsating 1,8.
One case series showed that 80% of patients had been symptomatic 2, but incidental diagnosis in asymptomatic patients is possible 20.
Pathology
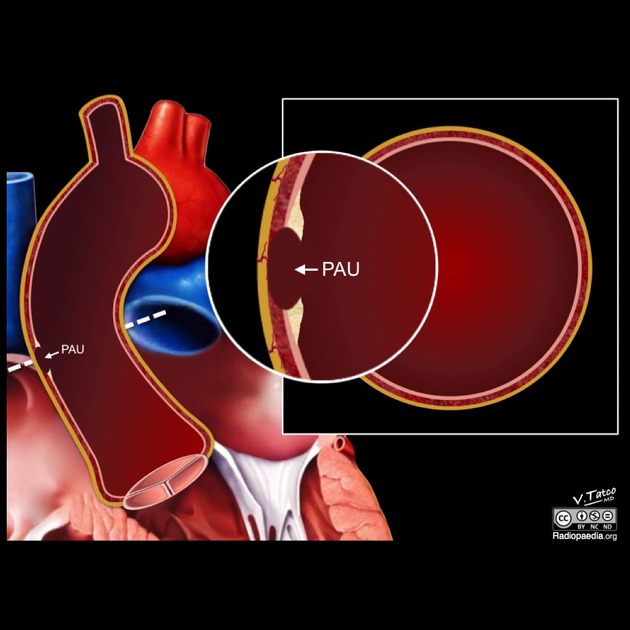
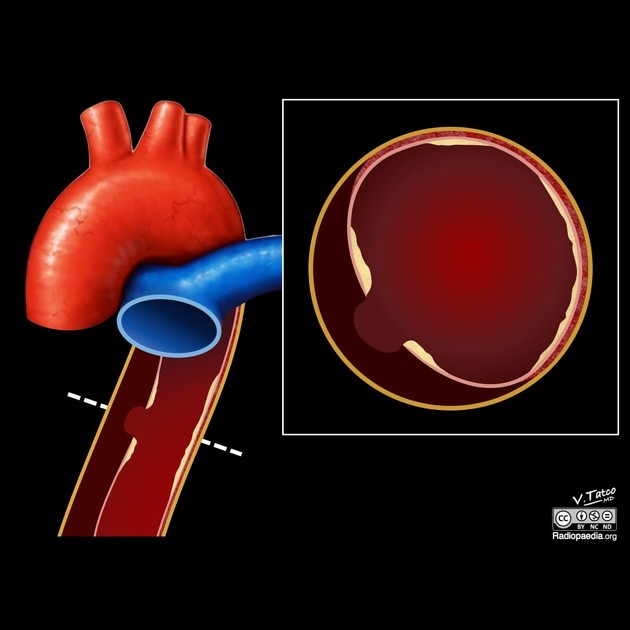
An ulcerating atherosclerotic lesion that penetrates the intima and progresses through the internal elastic lamina into the media, and can progress to cause an intramural hematoma of variable size 3,17. The early stages are often asymptomatic.
Penetrating atherosclerotic ulcers can resolve completely or stay stable, or they can also progress to aortic dissection, aortic saccular aneurysms, perforation and spontaneous aortic rupture. There are conflicting reports about the most common course of penetrating atherosclerotic ulcers 1.
Imaging modalities cannot reliably determine if an ulcer has penetrated the internal elastic lamina 17. Due to this limitation, it is also difficult to differentiate an ulcerated plaque from a penetrating atherosclerotic ulcer. Some features that may aid this differentiation are:
ulcerated plaques have an undulating interface with overlying thrombus whereas a penetrating atherosclerotic ulcer has a smooth interface with the intramural hematoma
contrast extends beyond intimal calcification in a penetrating atherosclerotic ulcer
intimal calcification occurs at the same site as an ulcerated plaque whereas intimal calcification is often remote to a penetrating atherosclerotic ulcer
Patients with penetrating atherosclerotic ulcers and aortic intramural hematomas have an increased risk of concomitant abdominal aortic aneurysm 17.
Location
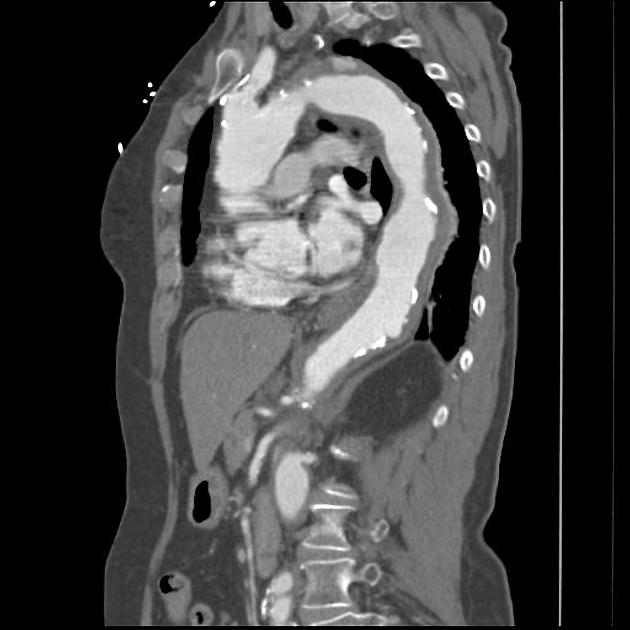
There is a greater predilection to involve the aortic arch and mid to distal thoracic aorta 6,22.
Size
Penetrating atherosclerotic ulcers with a depth >10 mm and width >20 mm are associated with a higher rate of progression to aortic dissection, aneurysm and rupture 17,21. Ulcer depth is the distance penetrated beyond the intima, and width is the maximal perpendicular dimension of the ulcer within the vessel wall 21. Increasing aorta diameter at the level of the ulcer is predictive of medical management failure 22.
Classification
As with classical aortic dissection, penetrating atherosclerotic ulcers are classified according to the Stanford scheme.
Radiographic features
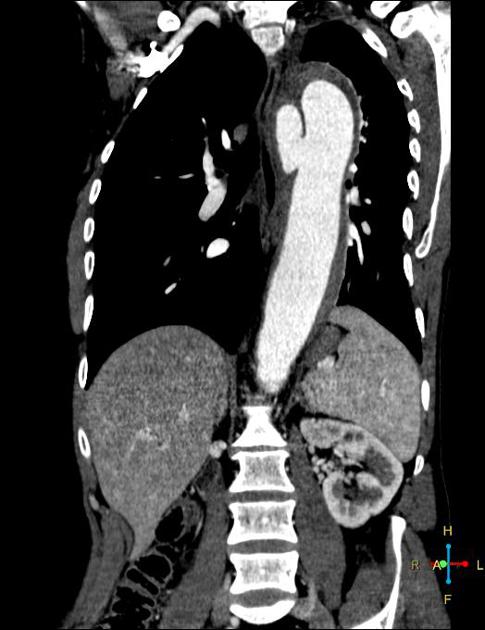
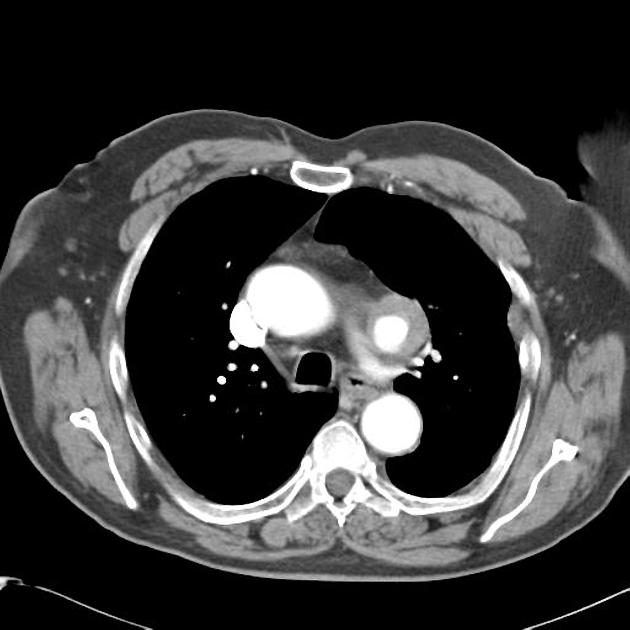
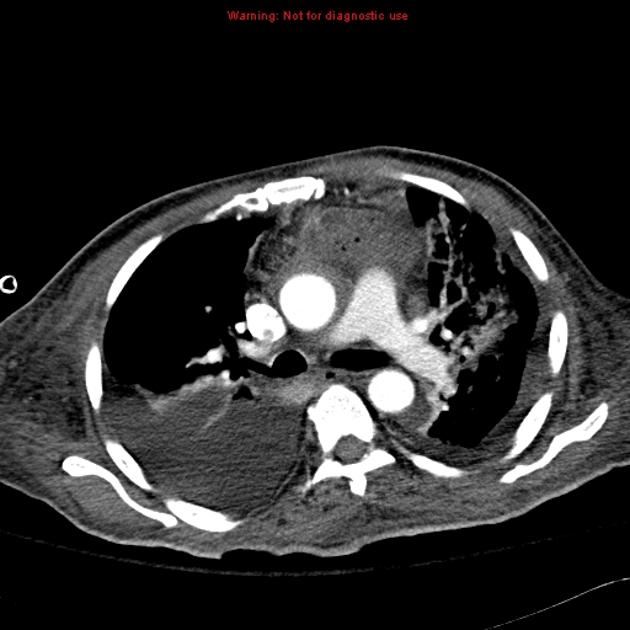
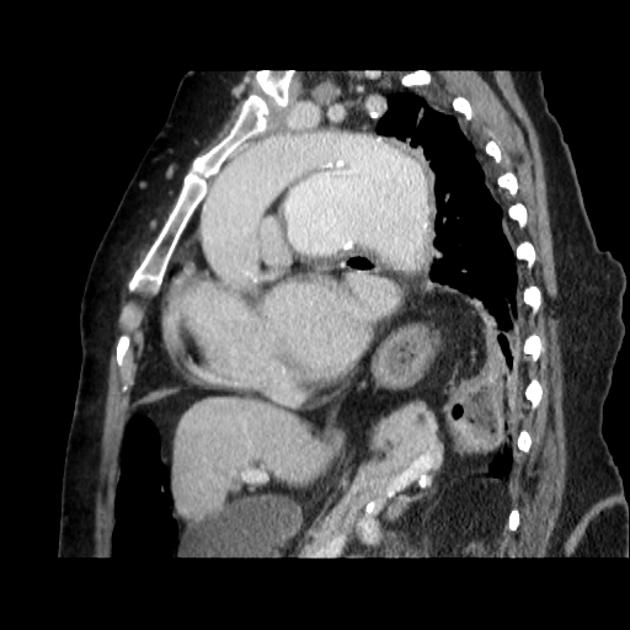
CT
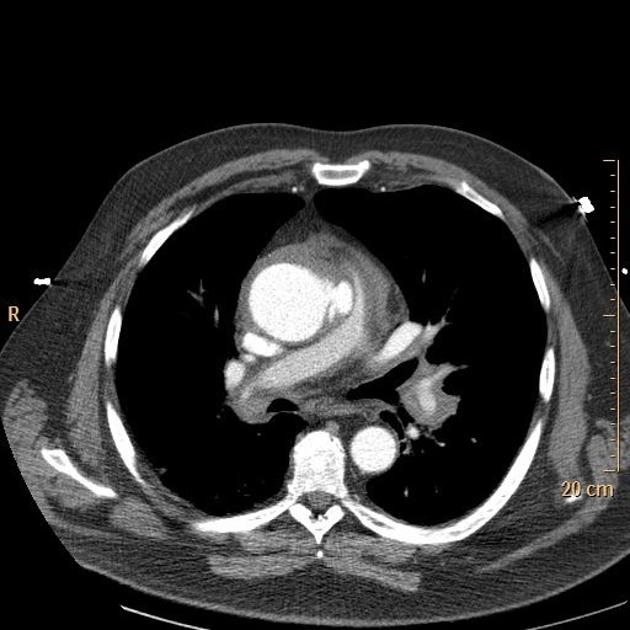
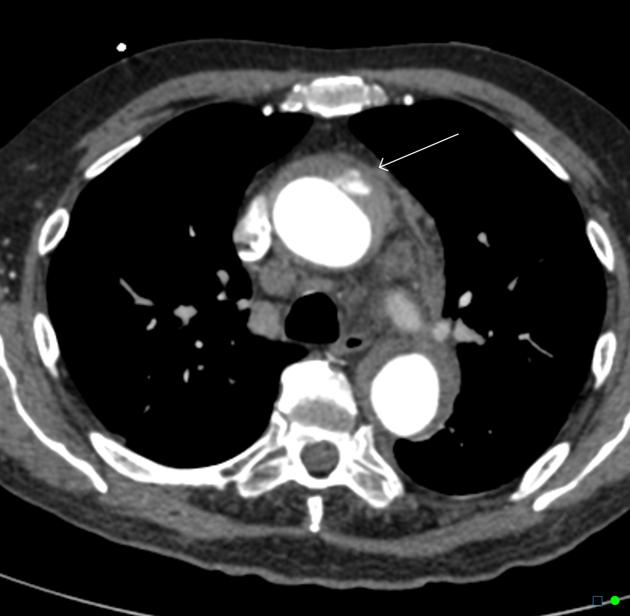
On CT aortography, the typical finding is a contrast-filled, out-pouching of the wall of the aorta or into the thickened aortic wall in absence of an intimal flap or a false lumen. The protrusion is said to resemble a mushroom 14 and can appear similar to an ulcerated plaque 17. These can progress to an intramural hematoma and often have an adjacent intramural hematoma. Often there are signs of extensive atherosclerosis in other sites remote to the ulceration 4.
Most commonly, penetrating atherosclerotic ulcers are located in the descending thoracic aorta. Ulcers of the aortic arch are less common, and rare in the ascending aorta 4.
Although associated pleural effusion correlates with clinical instability there are no validated imaging features for the prediction of the course of a penetrating atherosclerotic ulcer 1. It is often difficult to determine if a penetrating atherosclerotic ulcer is the source of a patient's pain or if it is an incidental finding.
In follow-up studies increasing maximum diameter and depth of the ulcer is an obvious sign of progression 1. However, there is no consensus for ulcer depth or diameter that warrants treatment 14.
A CTA radiology report of penetrating atherosclerotic ulcers should include 17, 23:
proximal and distal extent of the ulcer
ulcer saccular depth
presence and thickness of associated intramural hematoma
maximum diameter of the affected aortic lumen
Transesophageal echocardiography
usually, transesophageal echocardiography demonstrates a localized, crater-like protrusion of the aortic lumen into the thickened aortic wall 9
often there are signs of extensive atherosclerosis in other sites apart from the ulceration 9
MRI and MRA
T1-weighted SE sequences show a hyperintense hematoma in acute or subacute disease and can distinguish between hematoma and atherosclerotic plaque 9
otherwise similar findings to CTA 9
DSA
the typical finding is a contrast-filled, pouch-like protrusion of the aortic lumen 9
mostly several oblique projections are required 9
Treatment and prognosis
There are no set guidelines on when to treat and practices vary between hospitals, however general principles are as follows:
-
although the involvement of the ascending aorta in penetrating atherosclerotic ulcers is rare, the ulcers usually rupture
therefore early or emergent surgical intervention is recommended 4
-
-
asymptomatic:
-
may initially be managed with an aggressive (antihypertensive) medical therapy in combination with close clinical and radiographic follow-up
small neck width of the penetrating atherosclerotic ulcer and lack of associated aneurysmal change are associated with successful conservative management 18
annual CT imaging follow-up has been suggested 10
-
-
symptomatic or signs of progression:
higher risk for spinal cord ischemia
endovascular stent-grafting (TEVAR) 4
-
-
generally asymptomatic/incidental and slow-growing 15
mortality is determined by concurrent co-morbidities such as concurrent aortic aneurysm
Complications
Recognized complications include:
transmural aortic rupture
embolic phenomena
pseudoaneurysm formation
progressive aneurysmal dilatation
History and etymology
They were first described as a distinct clinical and pathological entity by Anthony Stanson et al. in 1986 19.
Differential diagnosis
General imaging differential considerations include:
focal indentation as part of irregularity along mural aortic plaque: could represent a non-penetrating atheromatous ulcer
saccular aneurysm










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.