Small bowel obstruction (SBO) refers to mechanical blockage of the transit of intestinal contents through the small bowel. CT in particular plays a key role in the diagnosis and can help identify the cause of obstruction and assess for potential complications.
On this page:
Terminology
The degree of obstruction can be described as complete or incomplete (alternatively high-grade or partial) depending on whether enteric contents can pass beyond the site of obstruction. This is often inferred based on the degree of upstream small bowel dilation, the severity of narrowing at the transition point, and the passage of oral contrast (if administered).
Closed-loop small bowel obstruction occurs when the bowel is obstructed at two points, typically close to one another, entrapping enteric contents in a closed-loop segment and leading to progressive vascular compromise with a high risk of developing ischemia and infarction. The importance of this distinction is discussed in detail below. Non-closed-loop obstruction is also known as open-loop or simple obstruction 11.
Epidemiology
The incidence of small bowel obstruction is variable depending on the etiology of the obstruction. The most common cause of SBO is adhesive disease, and the greatest risk factor for developing adhesions is prior surgery 1.
Diagnosis
The diagnosis is usually made through CT and can be confirmed during laparotomy if surgery is required ref. Abdominal radiographs can serve as a first step toward diagnosing an obstruction but do not provide information about the cause, grade, or complications of the obstruction, and thus a CT is appropriate in most cases to guide management ref.
Clinical presentation
The clinical presentation of small bowel obstruction varies according to its etiology. Gradual partial obstruction typically manifests with intermittent abdominal discomfort, decreased bowel movements, and vomiting. In contrast, closed-loop obstruction presents more acutely, often with sudden onset of abdominal pain and signs of shock due to rapid vascular compromise. Vomiting may be absent in such cases, as the proximal bowel may not have had sufficient time to dilate before vascular compromise leads to symptoms of severe pain.
Pathology
Simple obstruction (non-closed loop)
A simple (a.k.a. open loop or non-closed loop) obstruction is defined by the presence of a single transition point causing obstruction. This type of obstruction can be further classified into two categories: (1) complete or high-grade obstruction, where no fluid or gas passes beyond the obstruction site, and (2) incomplete or partial obstruction, where some fluid or gas can still traverse the obstructed area 2.
Extrinsic compression
adhesions (most common) ref
-
less common causes of extrinsic compression
serosal/peritoneal metastases: may extrinsically compress small bowel or cause abrupt kinking by limiting its mobility
inflammation secondary to peritoneal endometriosis, fistulas (e.g. fistulizing diverticulitis), abscess, or aneurysm may pull in and tether small bowel, causing kinking and obstruction by a similar mechanism to adhesive disease.
Primary bowel pathology
-
inflammatory conditions
vasculitis
radiation enteritis
-
malignancy
primary small bowel tumor, e.g. adenocarcinoma, neuroendocrine tumor (NET), gastrointestinal stromal tumor (GIST), lymphoma
-
small bowel metastases
hematogenous metastases (melanoma, lung, etc.)
serosal/peritoneal metastases (ovarian, colorectal, peritoneal mesothelioma, pseudomyxoma, etc.)
-
intraluminal conditions
gastric balloon migration
ingested foreign body (e.g. fish bone, tooth pick, grill brush bristle)
Closed-loop obstruction
Closed-loop small bowel obstruction occurs when the bowel is obstructed at two points, typically close to one another, entrapping enteric contents in a closed-loop segment and leading to progressive vascular compromise with a high risk of developing ischemia and infarction. The most common causes are adhesions, hernia (internal and external), and volvulus. The etiology is discussed in detail in the dedicated closed-loop article.
Radiographic features
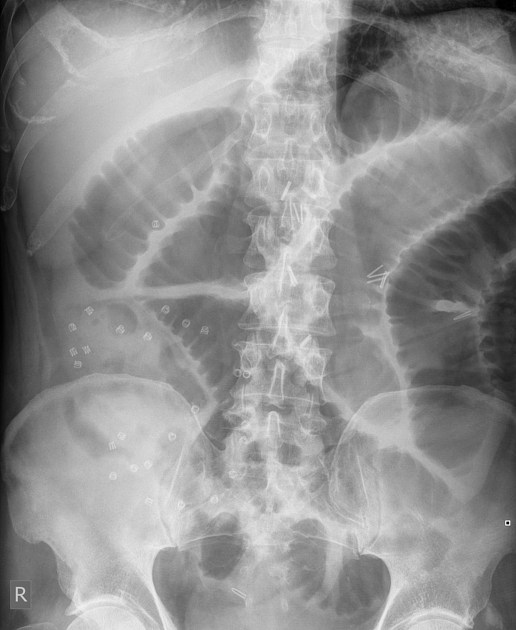
Plain radiograph
Abdominal radiographs have a sensitivity of ~55% (range 50-60%) for small bowel obstruction 3. In most cases, the abdominal radiograph will have the following features ref:
dilated loops of small bowel proximal to the obstruction (see 3-6-9 rule)
predominantly central dilated loops
multiple dilated loops of bowel
valvulae conniventes are visible
-
gas-fluid levels if the radiographic is erect, especially suspicious if 8
>2.5 cm in width
in the same loop of the bowel but at different heights (>2 cm difference in height)
However, obstruction (which may be high-grade mechanical obstruction) may also present with the following features ref:
gasless abdomen: gas within the small bowel is a function of vomiting, nasogastric tube placement, and level of obstruction
string-of-beads sign: small pockets of gas within a fluid-filled small bowel
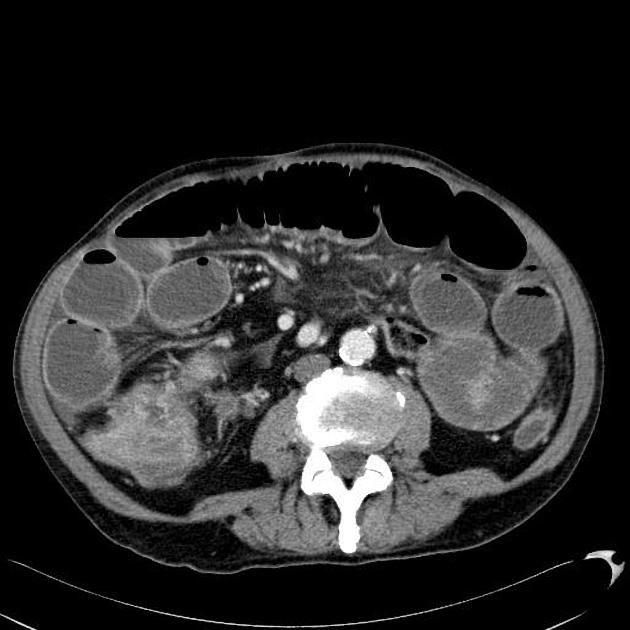
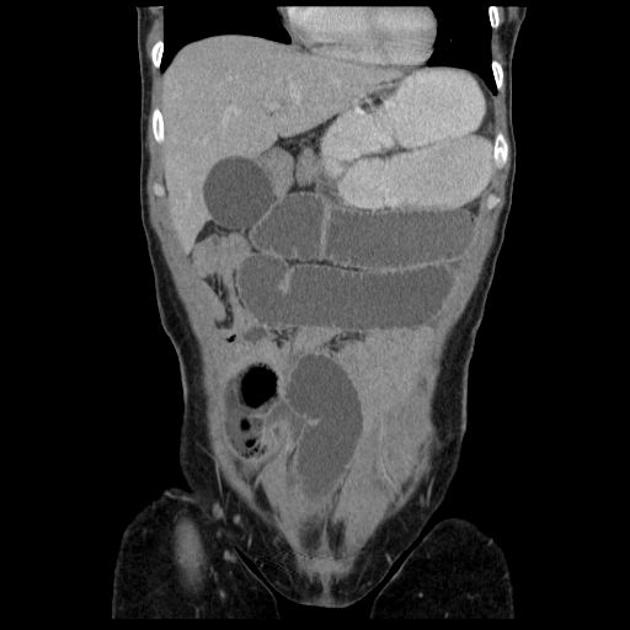
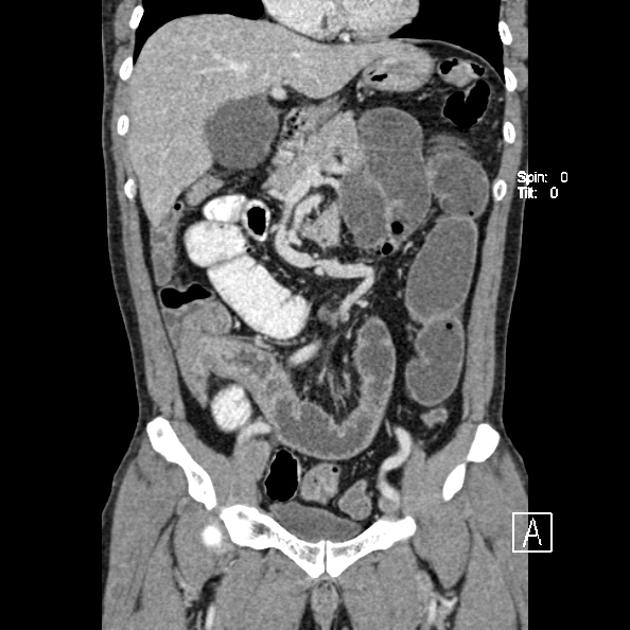
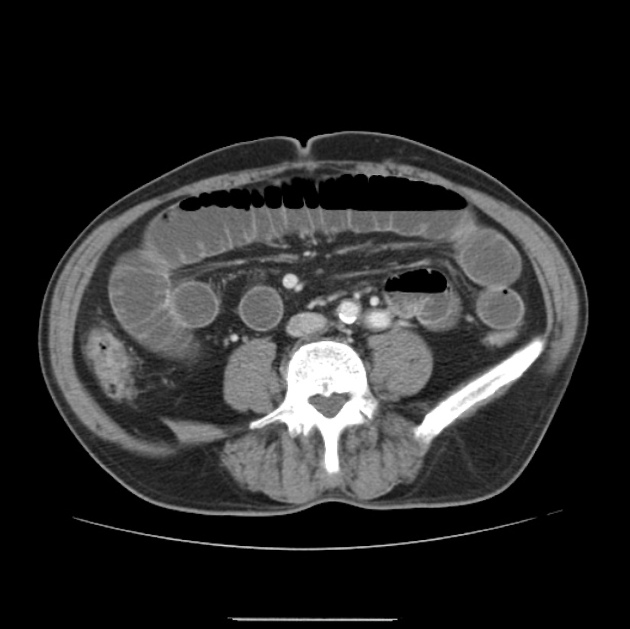
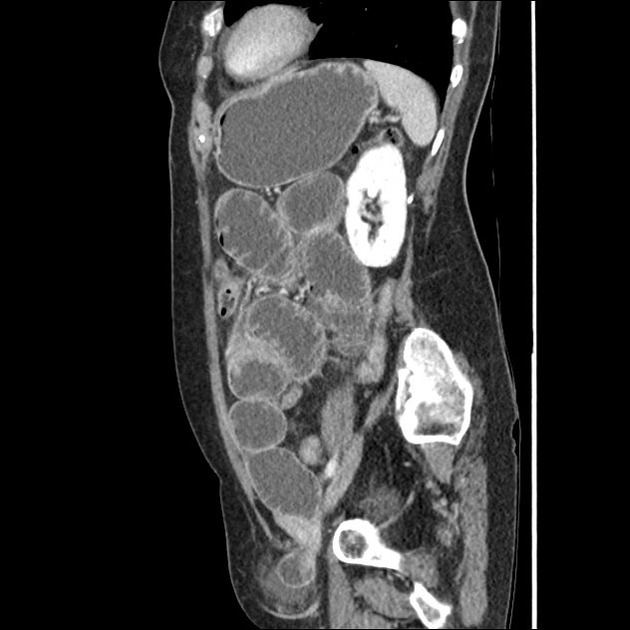
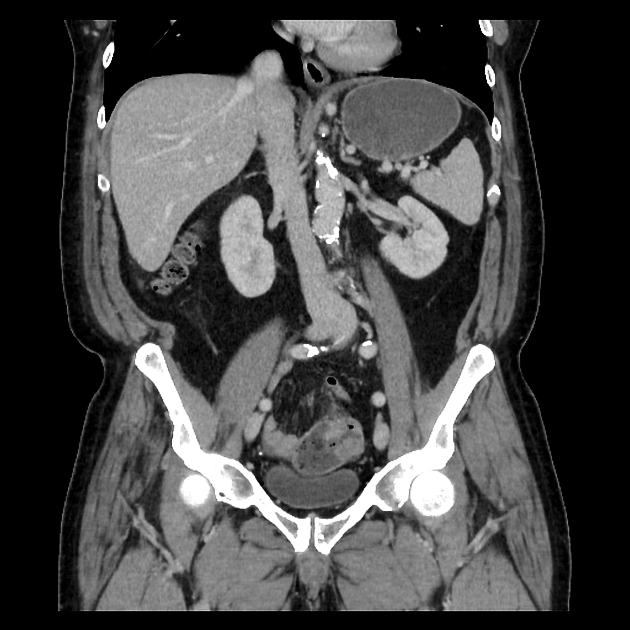
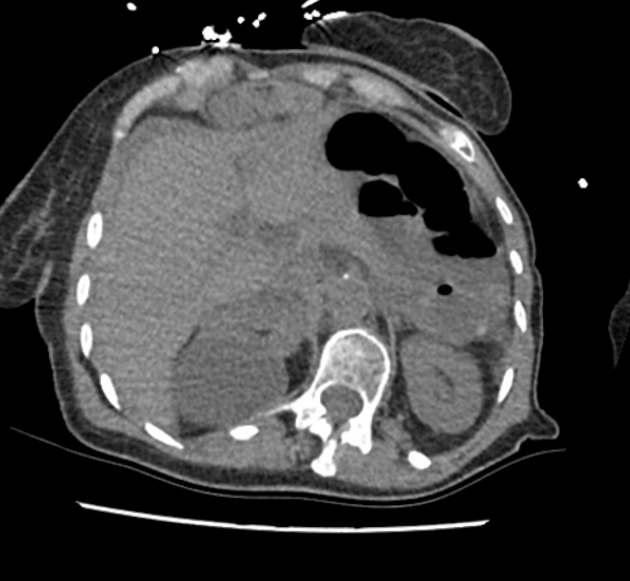
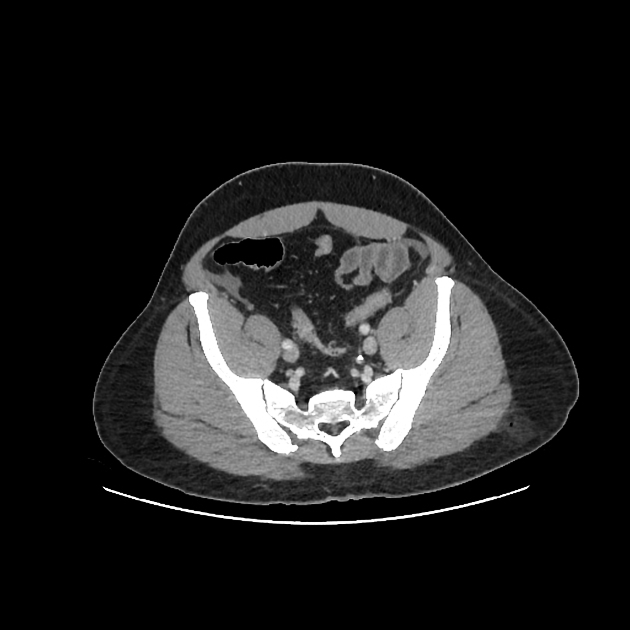
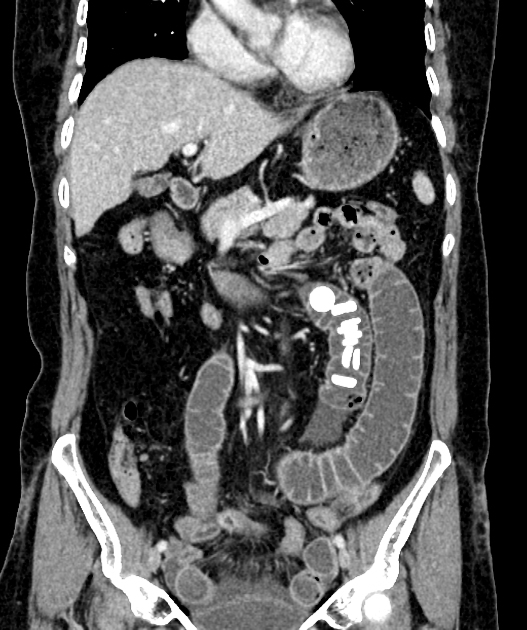
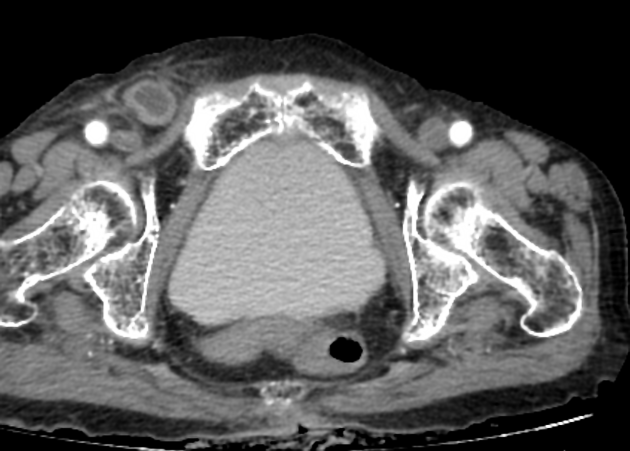
CT
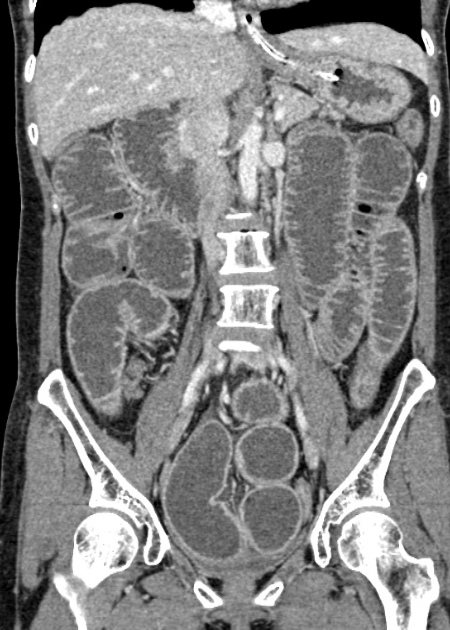
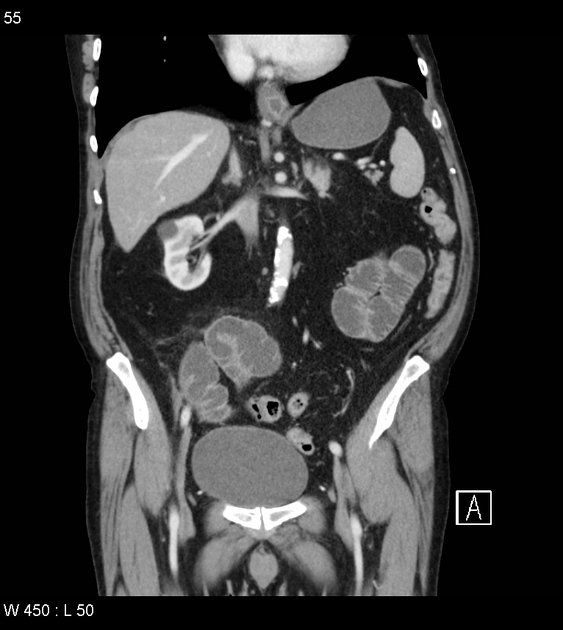
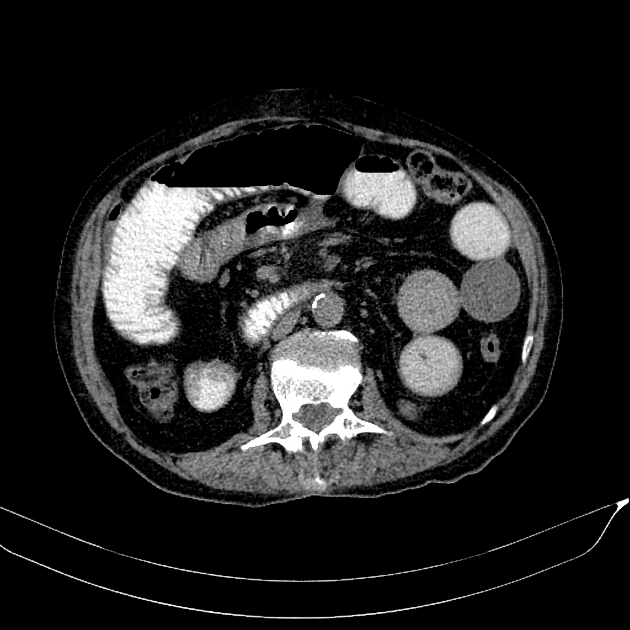
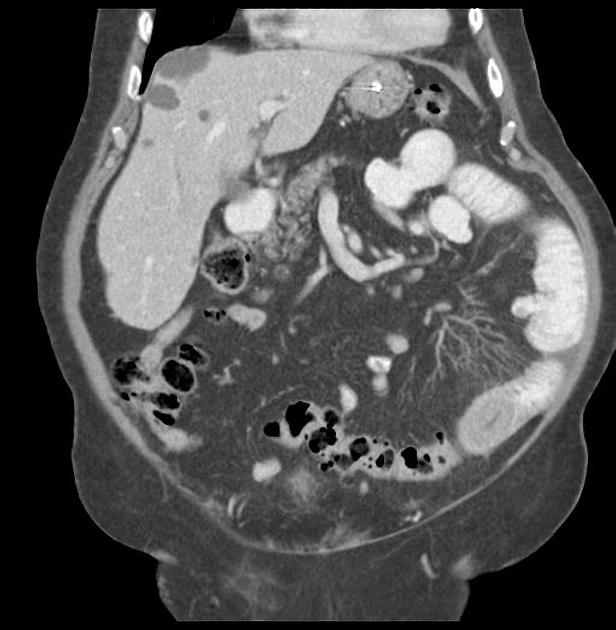
CT is more sensitive than radiographs and will demonstrate the cause in most cases. Features on CT may include:
dilated small bowel loops >2.5 cm up from outer wall to outer wall
normal caliber or collapsed loops distally
fat notch sign (typically indicates adhesive SBO) 11
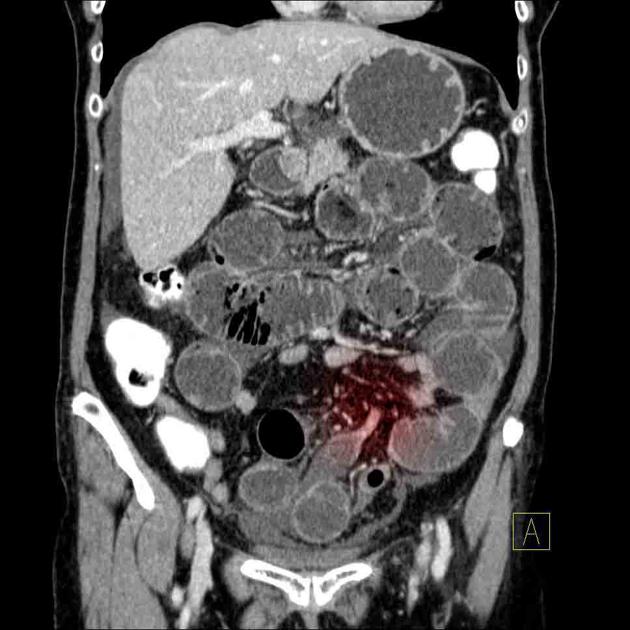
Closed-loop obstructions are diagnosed when a bowel loop of variable length is occluded at two adjacent points along its course, which may be partial or complete with characteristic features:
asymmetric mesenteric edema involving the closed-loop segment
stretching or sharp angulation/narrowing of the mesenteric vessels as they are distorted by the entrance/exit of the closed loop
radial distribution of several dilated, fluid-filled bowel loops
U-shaped or C-shaped configuration of the closed-loop, which often is best seen on the coronal reformats
beak sign at the site of fusiform tapering, involving both ends of the closed loop
whirl sign reflecting rotation of bowel loops around a fixed point
intramural hemorrhage: high-density fluid within the wall of the affected small bowel is most prominent on non-contrast imaging
Strangulation refers to impaired blood flow (decreased perfusion) to the small bowel caused by obstruction, which can lead to bowel ischemia. Closed-loop obstructions are at particular risk for ischemia and infarction. This is mainly seen when the diagnosis is delayed (up to 10% of small bowel obstructions) and associated with high mortality 1. Features are non-specific and include ref:
thickened and increased attenuation of the bowel wall
Increased attenuation of bowel contents due to hemorrhage
halo or target sign
pneumatosis intestinalis
portal venous gas
localized fluid or hemorrhage in the mesentery
Positive oral contrast is not usually necessary for the diagnosis of small bowel obstructions as it tends to dilute in the setting of SBO, does not reach the transition point, and may obscure the evaluation of the bowel wall (thereby limiting the evaluation of bowel ischemia) 4.
In uncomplicated cases of adhesional small bowel obstruction, where complications such as ischemia or perforation are absent, a water-soluble contrast challenge may be employed. This approach serves both diagnostic and therapeutic purposes 5.
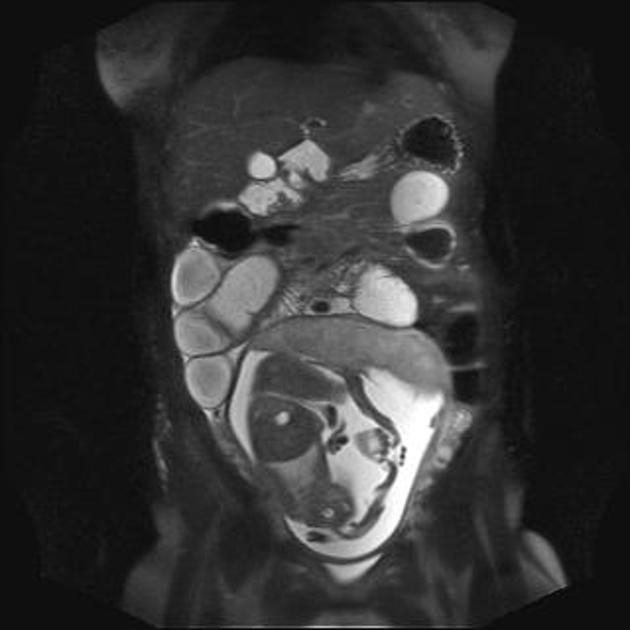
MRI
MRI is not commonly used for the diagnosis of small bowel obstruction, but has a role for the evaluation of pregnant patients for whom ionizing radiation is contraindicated.
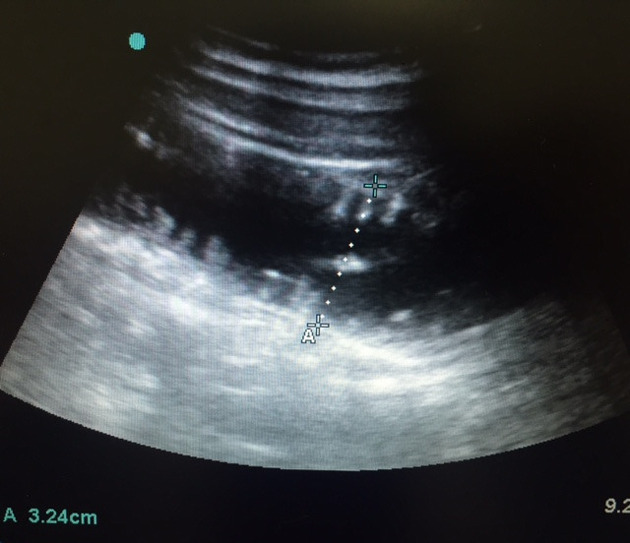
Ultrasound
Ultrasound is a bedside test that can help to diagnose small bowel obstruction. Findings suggestive of small bowel obstruction 6:
dilated bowel loop (diameter >3 cm)
-
ineffective peristalsis
results in "to-and-fro" or "whirling" appearance of intraluminal contents
-
prominence of the valvulae conniventes
present in dilated jejunal loops
The extent of obstruction is typically implied rather than sought directly based on the involvement of the ascending/descending colon, the morphology of the small bowel loops (high mucosal folds pattern present in the jejunum, absent in the ileum), and involvement of the stomach.
Findings suggestive of bowel ischemia/infarction ref:
extraluminal free fluid
the "pointy" triangular appearance of interloop free fluid is sometimes referred to as the tanga sign
loss of peristalsis
bowel wall thickening >3 mm
with effacement of mural architecture
mural gas
Radiology reporting
Key features to include in the radiology report:
whether the obstruction is a simple, single-point obstruction or closed-loop
location of obstruction and the appearance of the transition point
-
number of points of obstruction
especially in obstruction secondary to serosal disease or small bowel tethering by infective or malignant disease
favored etiology
presence of complications (e.g. perforation or ischemia)
Treatment and prognosis
Non-operative treatment of small bowel obstruction usually consists of gut rest and decompression via a nasogastric tube. Parenteral fluids or nutrition are typically given in conjunction with this ref.
Water-soluble contrast challenges are used as a diagnostic and therapeutic tool for non-closed loop small bowel obstruction. Various protocols exist, but typically involve the administration of around 100 mL of water-soluble contrast orally or via a nasogastric tube, followed by abdominal radiographs 6-12 hours later to assess for passage of contrast into the colon 7. If contrast has not passed into the colon at 24 hours after administration, this suggests the obstruction is unlikely to resolve spontaneously and is a relative indication for surgery 8-9. Traditionally Gastrografin was used, but other water-soluble agents are similarly effective 10.
Differential diagnosis
-
clinically, it may present similarly with nausea, vomiting, and abdominal pain
air in the sigmoid colon or rectum is more likely to represent ileus
diffusely dilated loops of bowel without a transition point (including colon) are more likely to represent ileus
recent or concurrent trauma, surgery, or infectious/inflammatory process is more likely to represent ileus
fecal bowel sign is more likely to represent small bowel obstruction
-
causes of small bowel dilation, but not necessarily obstruction
endometriosis
ischemia
-
enteritis
this often causes bowel wall thickening and mild dilation with mesenteric edema, but without a transition point. Involvement of the stomach and large bowel can also be seen.
-
medication-related
angioedema
chemotherapy
-
colon cancer
ileocecal tumor
pediatric small bowel atresia

































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.