Spinal compression fractures occur as a result of injury, commonly fall onto the buttock or pressure from normal activities, to the weakened vertebrae due to osteoporosis.
On this page:
Epidemiology
They have a reported incidence of 1.2 per 1000 person-years after 85 years of age in the United States. However, they are largely unreported and are probably more common radiographically (present up to 14% of women older than 60 years in one study 1).
Clinical presentation
Vertebral fractures present with pain and loss of mobility.
Pathology
Compression fractures can result from osteoporosis, trauma or represent a pathological fracture secondary to another process (e.g. infection, tumor) ref.
Common descriptors include 6:
wedge compression fracture: involvement of one endplate but not the posterior wall
pincer or split fracture: involvement of both endplates but not the posterior wall
burst fracture: involvement of one endplate (incomplete) or both endplates (complete) and the posterior wall
Classification
See: AO spine classification of thoracolumbar injuries.
Osteoporotic spine fractures can be graded with the Genant classification of vertebral fractures based on vertebral height loss as:
mild: up to 20-25%
moderate: 25-40%
severe: >40%
Radiographic features
Vertebral fractures require treatment when they are symptomatic, i.e. with pain and loss of mobility. This defines the role of the radiologist in making an accurate diagnosis.
The vertebral fracture should be diagnosed when there is a loss of height in the anterior, middle, or posterior dimension of the vertebral body that exceeds 20%. When in doubt, it is recommended that additional views or studies be advised for confirmation.
Acute vs chronic
Chronicity of the fracture indicates its temporal relationship with symptoms and hence is an important determination.
On conventional imaging, acute fracture signs include cortical breaking or impaction of trabeculae; in the absence of these signs fractures are chronic.
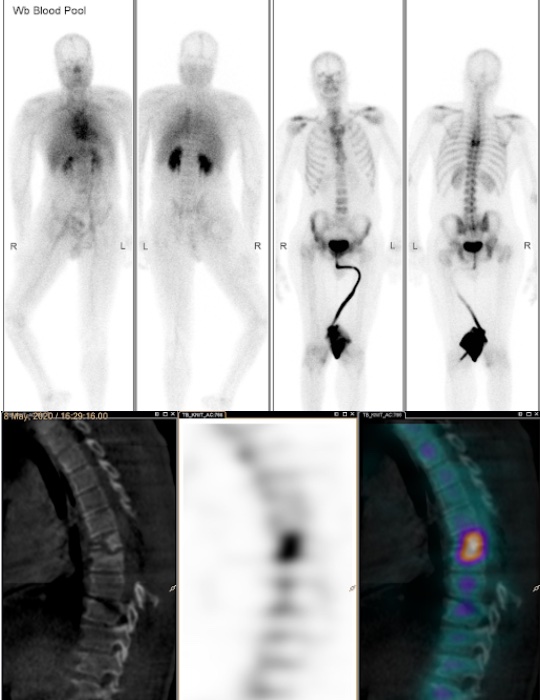
In uncertain cases, MRI signs of edema (acute) and the presence of radiotracer uptake on bone scintigraphy (acute) help decide the age of the fracture.
Osteoporotic vs pathological
Discriminating between acute osteoporotic fracture and pathological fracture is sometimes challenging.
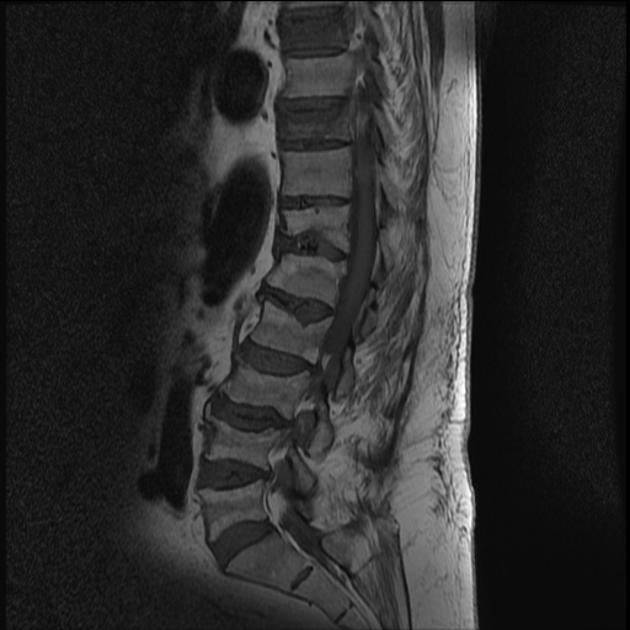
The following features favor the diagnosis of a benign compression fracture:
no bony destruction
preserved normal fatty bone marrow T1WI signal
low signal intensity band on T1WI and T2WI indicating a fracture line
retropulsion (not posterior bulging) of the posterosuperior cortex of the vertebral body
no epidural mass
multiple compression fractures
More details here
Treatment and prognosis
Management options include:
-
non-surgical
observation/bracing
medications: bisphosphonates for osteoporosis
-
surgical
kyphoplasty: balloon-assisted variant of vertebroplasty




















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.