Spondylolysis, commonly known as pars interarticularis defect or pars defect, is a defect in the pars interarticularis, the portion of the vertebral arch that connects the superior and inferior articular facets. It usually occurs in the lumbar spine.
A pars defect is one of the posterior vertebral fusion anomalies.
On this page:
Epidemiology
Spondylolysis is present in ~5% of the population 2 and higher in the adolescent athletic population. It is more common in men than in women 1. The vast majority of cases are located in the lumbar spine 11.
Associations
~65% of patients with spondylolysis will progress to spondylolisthesis 2, which is seen radiographically in ~25% 4; in most patients, this occurs before the age of 16 years
idiopathic scoliosis: ~5% 8
Clinical presentation
Spondylolysis is commonly asymptomatic. Symptomatic patients often have pain with extension and/or rotation of the lumbar spine. Approximately 25% of individuals with spondylolysis have symptoms at some time.
It is a common cause of low back pain in adolescents and may be the cause of low back pain in ~50% of adolescent athletes 7.
Pathology
Spondylolysis may be developmental or acquired. Developmental defects may develop in patients <10 years 7. Acquired defects have two main mechanisms:
repeated microtrauma, resulting in a stress injury and eventual fracture of the pars interarticularis; a dysplastic pars is usually present
traumatic pars defects result from high-energy trauma where there is hyperextension of the lumbar spine and are rare in a congenitally normal vertebra
Location
~90% of cases of spondylolysis occur at the L5 level and ~10% occur at the L4 level 1,2
unilateral or bilateral
Radiographic features
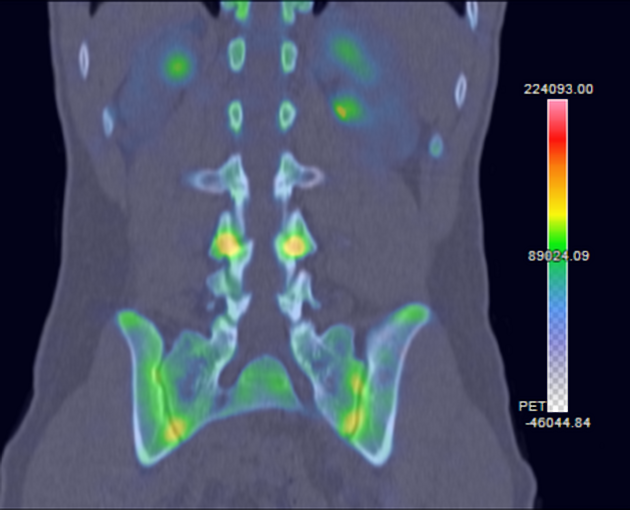
Imaging features depend on the age of the lesion. Plain radiographs and CT will only show established defects whereas SPECT-CT and MRI have the advantage of demonstrating stress response earlier through increased uptake or bone marrow edema signal respectively before a fracture has occurred.
CT has been considered the gold standard for investigating potential spondylolysis 7 although MRI should be considered with a similar sensitivity to other imaging modalities without exposure to ionizing radiation 9.
Plain radiograph
limited sensitivity compared to SPECT and CT 4
Scottie dog sign: on oblique radiographs, a break in the pars interarticularis can have the appearance of a collar around the dog's neck
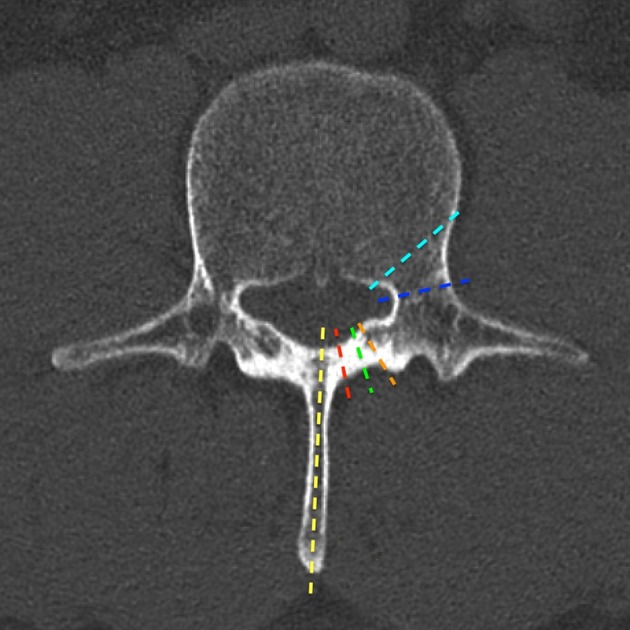
CT
wide-canal sign may be present on sagittal reformats when there is spondylolisthesis 3
deviation of the spinous process
sclerosis of the contralateral pedicle
Darth Vader sign on axial slices
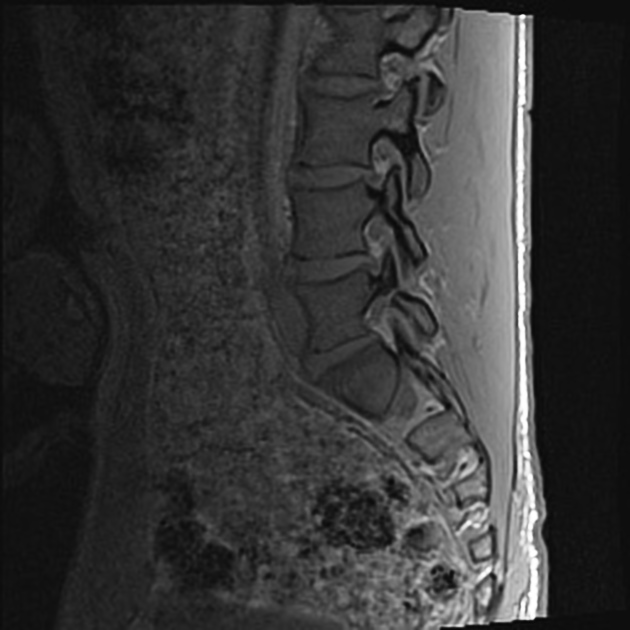
MRI
unilateral or bilateral bone marrow edema signal as a sign of stress response
-
fractures lines may be visible depending on sequence used
some sequences, e.g. T1 VIBE, have been shown equivalent to CT at detecting complete fractures 8
Classification
The Hollenberg classification system is based on MRI features but correlates well with SPECT-CT 6,7:
grade 0: normal pars interarticularis; MRI: no signal abnormality, pars interarticularis intact
grade I: stress reaction; MRI: marrow edema; intact cortical margins
grade II: incomplete stress fracture; MRI: marrow edema; incomplete cortical fracture or fissure
grade III: acute complete stress fracture; MRI: marrow edema; complete cortical fracture extending through pars interarticularis
grade IV: chronic stress fracture; MRI: no marrow edema; fractures completely extending through pars interarticularis
Treatment and prognosis
Surgery is only considered in rare circumstances as most cases respond to conservative management 2. Incomplete fractures demonstrate good healing rates with conservative management 7.













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.