Splenic abscesses, like abscesses elsewhere, are localized collections of necrotic inflammatory tissue caused by bacteria, parasites or fungi. They uncommonly affect the spleen due to its efficient reticuloendothelial system phagocytic activity and, consequently, are more likely seen in immunosuppressed patients.
On this page:
Epidemiology
Splenic abscesses are uncommon, and their incidence in various autopsy series is estimated at ~0.4% (range 0.14-0.7%) 2,15. The frequency may be rising due to an increase in the use of immunosuppressive agents and prevalence of immunosuppressive states, higher survival of leukemic patients, and a high incidence of intravenous drug use 13,15.
Clinical presentation
Splenic abscesses often present with vague, non-specific signs. Fever is common 3. Patients may present with left upper quadrant tenderness accompanied by rigors, chills, and vomiting. In most immunocompetent patients, a complete blood count will show marked leukocytosis with a left shift.
Pathology
Etiology
The main causes of splenic abscesses include:
immunodeficiency conditions (e.g. chemotherapy/transplant recipients, leukemia and AIDS): especially in those with multiple splenic abscesses 11,23
-
infection: anaerobes are thought to be the most common infective agents 8
-
metastatic infection
hematogenous bacterial dissemination, such as sepsis
contiguous infection, such as from a perinephric abscess or infected necrotic pancreatitis
-
splenic infarction with superimposed infection
Radiographic features
Plain radiograph
A plain abdominal radiograph is insensitive in the evaluation of splenic abscesses. Indirect signs include gas within the abscess, and a reactive left-sided pleural effusion 3.
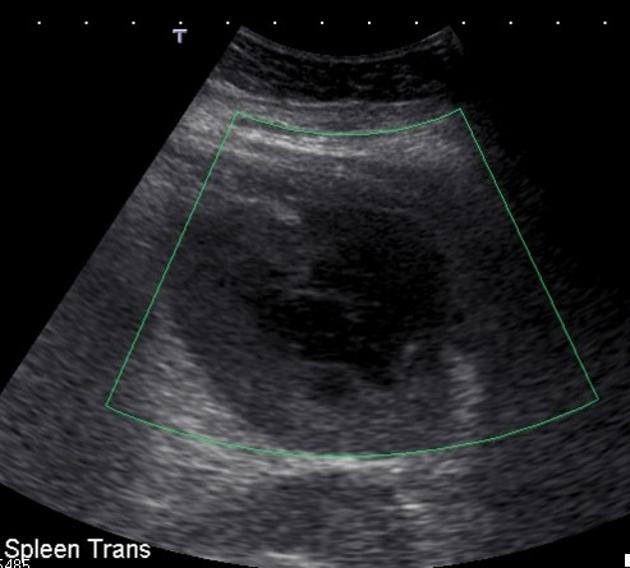
Ultrasound
Splenic abscesses are typically poorly-demarcated with a variable appearance, ranging from predominantly hypoechoic with some internal echoes to hyperechoic 23. They may contain septa of varying thickness. The presence of gas bubbles may also be seen with reverberation artifact, although the majority of splenic abscesses do not contain gas.
Ultrasound may also be used to guide abscess aspiration 22.
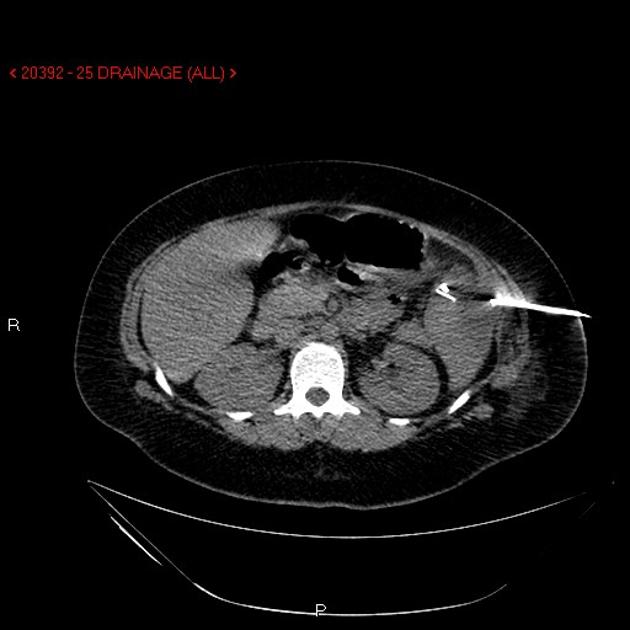
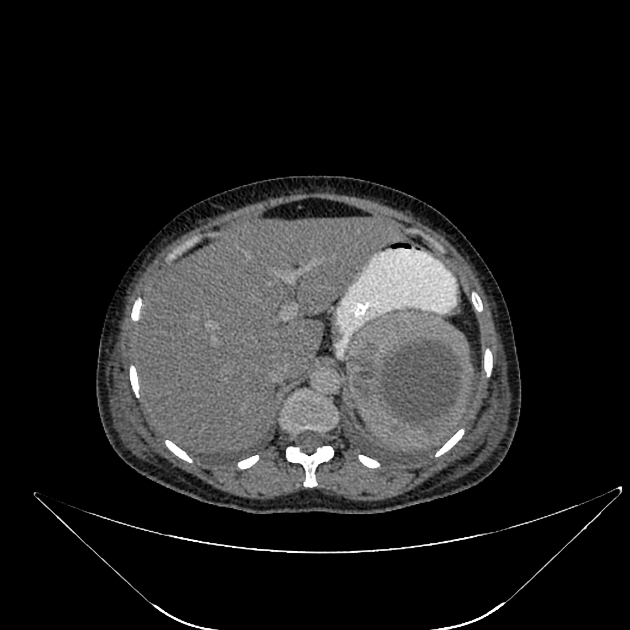
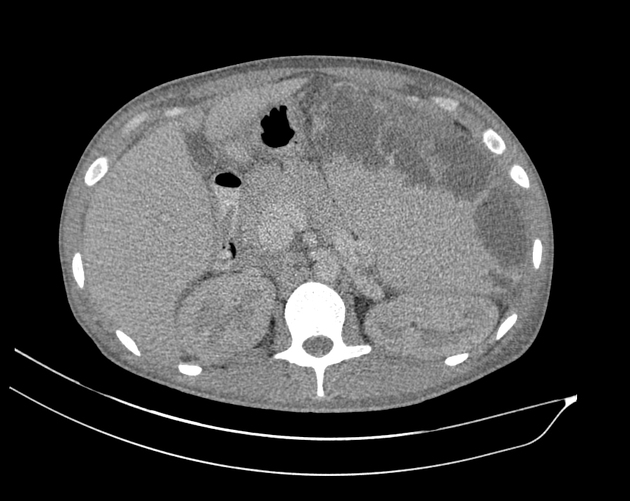
CT
Abscesses are normally seen as centrally low-density lesions (20-40 HU 17). Minimal peripheral contrast enhancement may be present once a capsule has developed. Ascites and adjacent pleural effusion can be seen.
MRI
May show solitary, multiple, or multilocular intrasplenic lesions. MR imaging characteristics can vary dependent on the size and infectious agent.
Usually, the abscesses are of fluid signal intensity 15,20:
T1: low signal (T1 signal may increase if there is proteinaceous content)
T2: high signal
-
T1 C+ (Gd)
there can be minimal peripheral enhancement once a capsule develops 15
larger lesions can also show peripheral and perilesional enhancement 16
Nuclear medicine
The clinical context is vital in interpreting nuclear medicine images.
In some cases, Tc-99m HMPAO leukocyte scans or Tc-99m HIG (human polyclonal immunoglobulin) scans may show one or more intrasplenic defects 5.
Indium-111 leukocyte scans and Ga-67 scans may also show a photopenic abscess cavity 19.
Treatment and prognosis
Traditional treatment for splenic abscess has been splenectomy and antibiotic therapy but image-guided percutaneous aspiration and drainage can also be considered. While many advocate image-guided drainage 9,10, several publications suggest that splenectomy has a better outcome than percutaneous drainage or intravenous antibiotics alone 3,4.
Differential diagnosis
As a broad differential for splenic abscesses, consider other splenic lesions.







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.