Subependymomas are uncommon, benign (WHO grade 1) tumors which are slow-growing and non-invasive. They tend to occur in middle-aged and older individuals and usually identified as an incidental finding.
On this page:
Terminology
These tumors were previously also known as subependymal astrocytomas, not to be confused with subependymal giant cell astrocytomas, which are both seen in association with tuberous sclerosis. They are also considered by some to be variants of ependymomas, with which they may co-exist (see below).
Epidemiology
Subependymomas tend to present in middle-aged to older individuals (typically fifth to sixth decades 3). There is a slight male predilection (M:F 2.3:1) 6,8. Rarely there is a genetic predisposition for these tumors 8.
Clinical presentation
Almost always an incidental finding on imaging done for another reason 9, as typically patients are asymptomatic. In some cases, especially when the tumors are larger, presentation is with symptoms of raised intracranial pressure due to obstructive hydrocephalus.
Pathology
Macroscopic appearance
Subependymomas are sharply demarcated nodules, usually no more than 2 cm in diameter, arising from the ependyma by a narrow pedicle 6,8. Size is the most important distinguishing feature compared to subependymal giant cell astrocytoma.
Microscopic appearance
The histopathology of subependymomas is distinct, consisting of a tumor arising from the subependymal glial layer with low cellularity and no high-grade features (no mitoses, Ki-67/MIBI index <1.5%, no necrosis). These lesions are hypovascular. Loose perivascular pseudorosettes are occasionally seen. They are a WHO grade 1 tumor (see WHO classification of CNS tumors) 8.
Occasionally, foci of cellular ependymoma are seen, although the effect on clinical behavior is unclear 4,5. They are graded according to the ependymoma component and, not surprisingly, behave similarly to the higher grade (ependymoma) component 6,8.
Immunophenotype
Cells express GFAP 4-6,8. Unlike ependymomas, EMA is usually negative 8.
Radiographic features
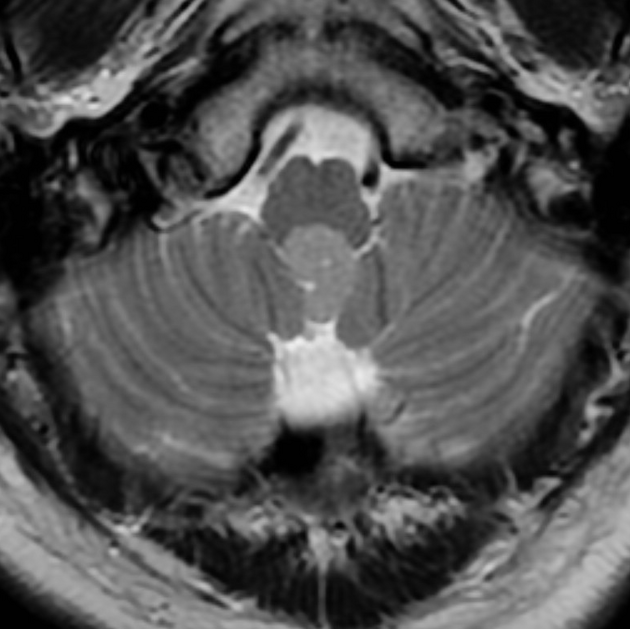
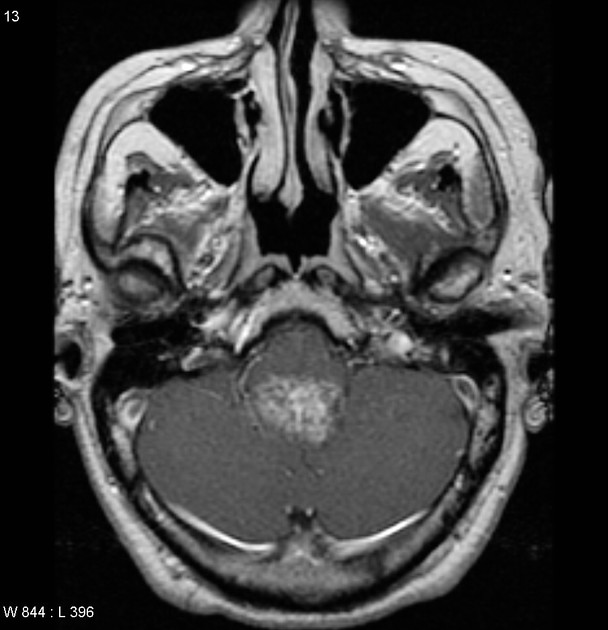
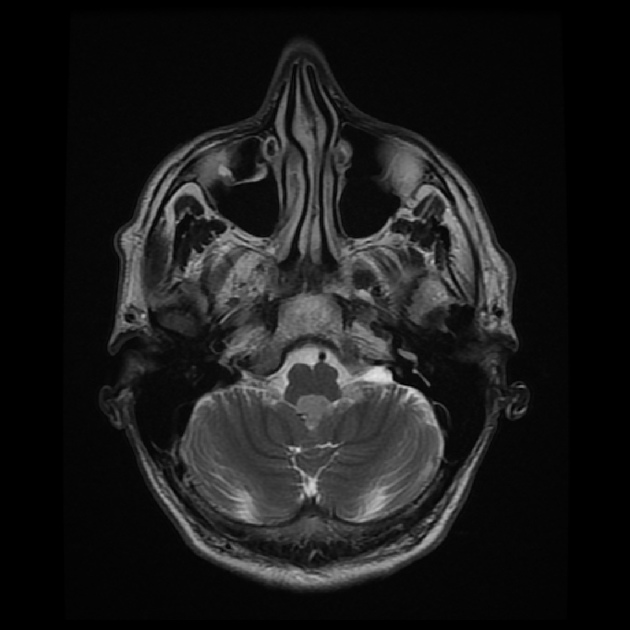
Subependymomas are most commonly seen in the fourth ventricle, but can arise anywhere where there is ependyma. They are, therefore, in the differential for other intraventricular masses. Distribution in the ventricular system is as follows 6,8:
fourth ventricle: 50-60%
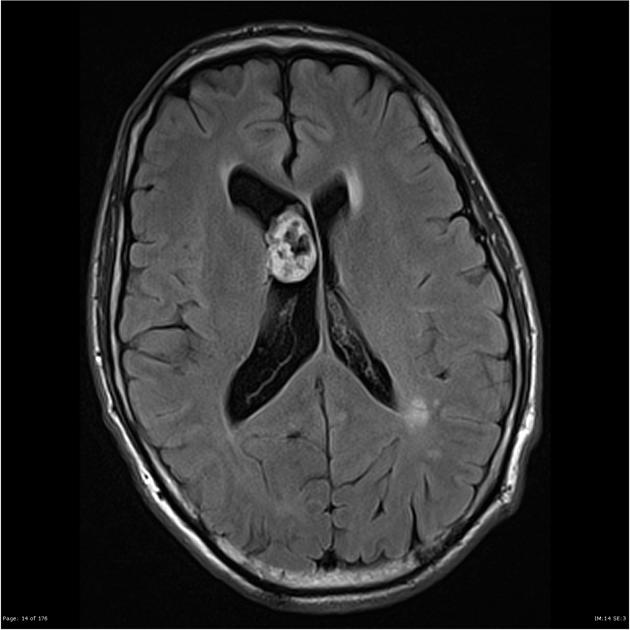
lateral ventricles (usually frontal horns): 30-40%
third ventricle: rare
central canal of the spinal cord: rare
They are usually small, typically less than 1-2 cm in size 6.
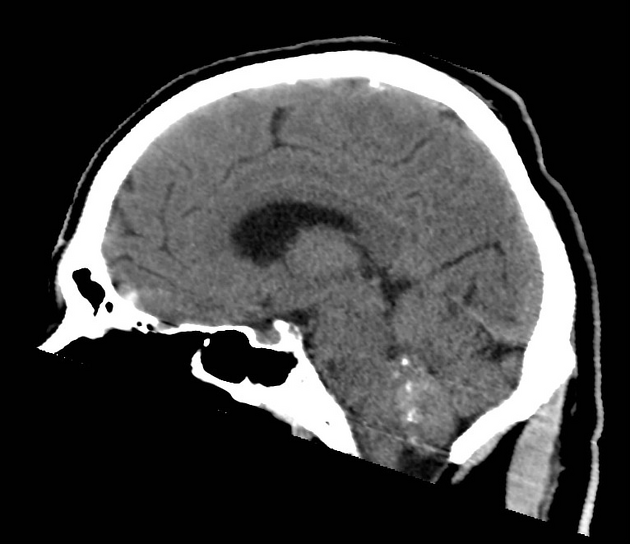
CT
Isodense to somewhat hypodense intraventricular mass compared to adjacent brain, which usually does not enhance. If large, it may have cystic or even calcific components (seen in up to half of cases 3). Surrounding vasogenic edema is usually absent.
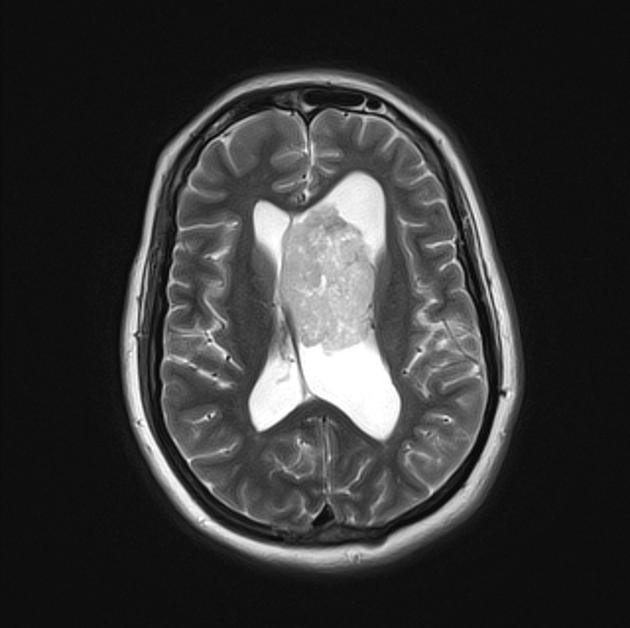
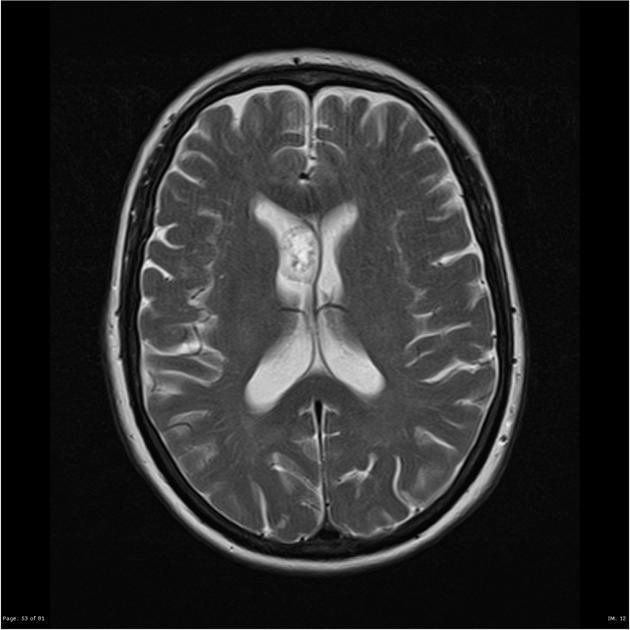
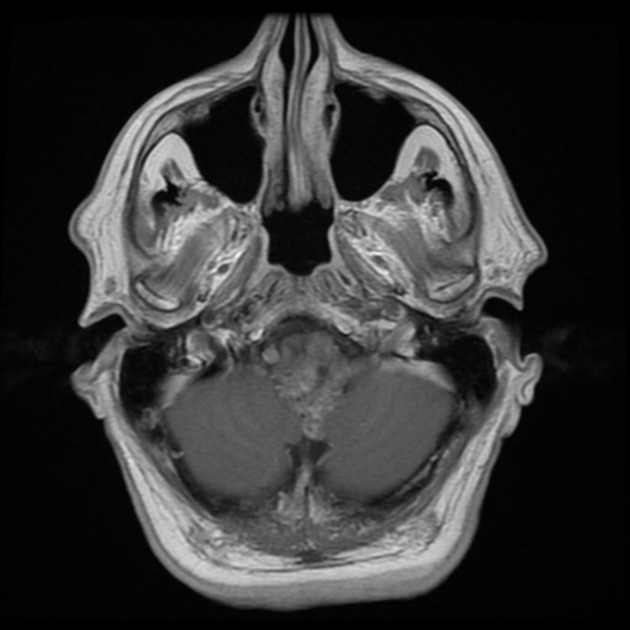
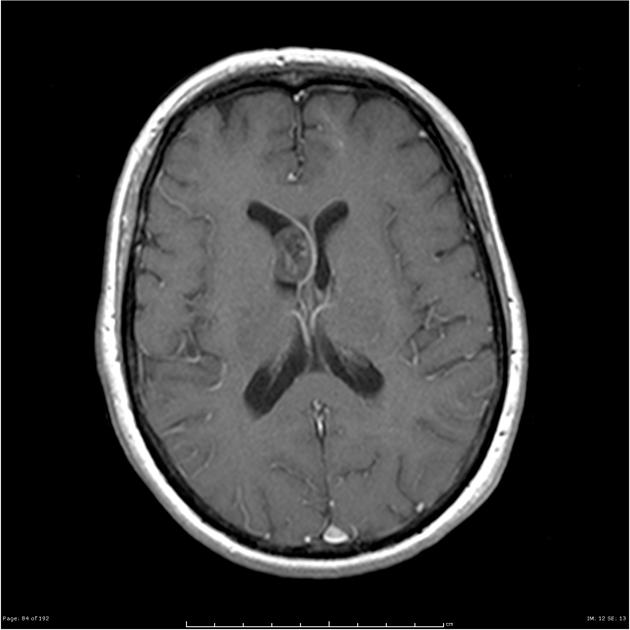
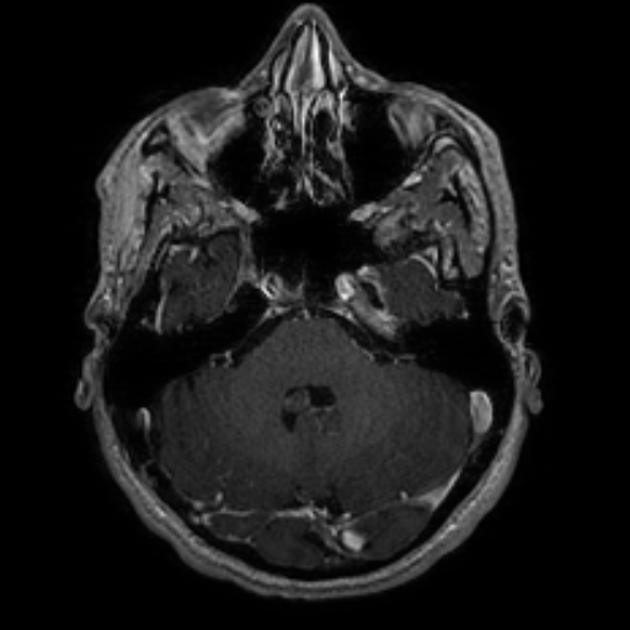
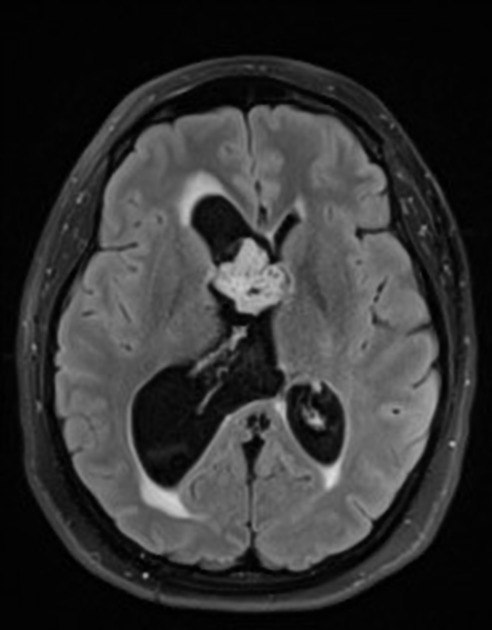
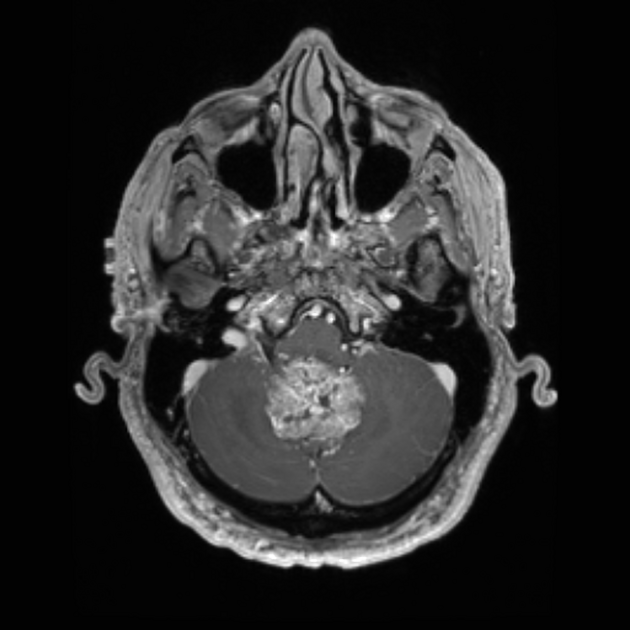
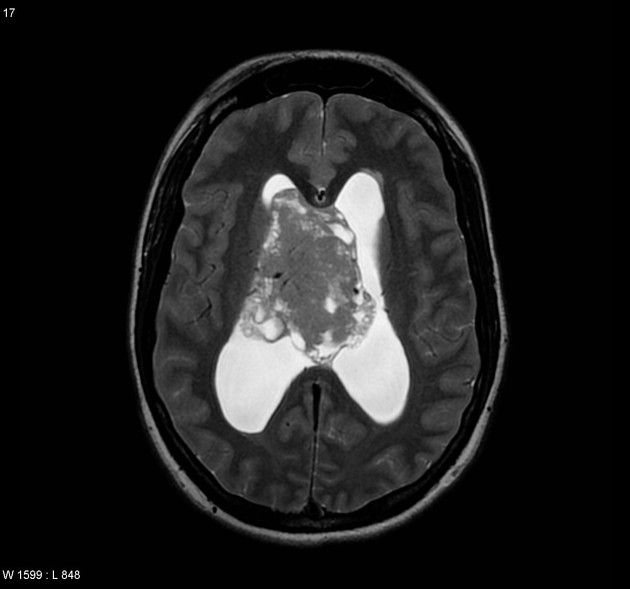
MRI
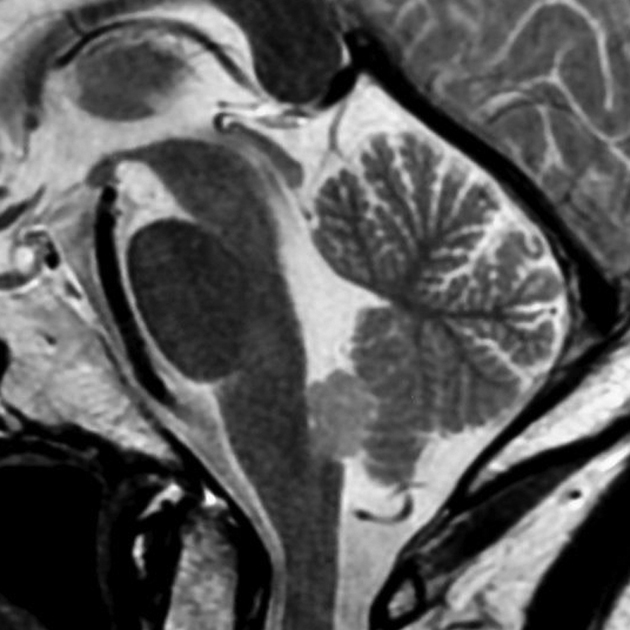
Well defined, round to oval shaped, lobulated contours; intratumoral cysts may be encountered 10.
-
T1
iso-to-hypointense to white matter
generally homogeneous but may be heterogeneous in larger lesions
-
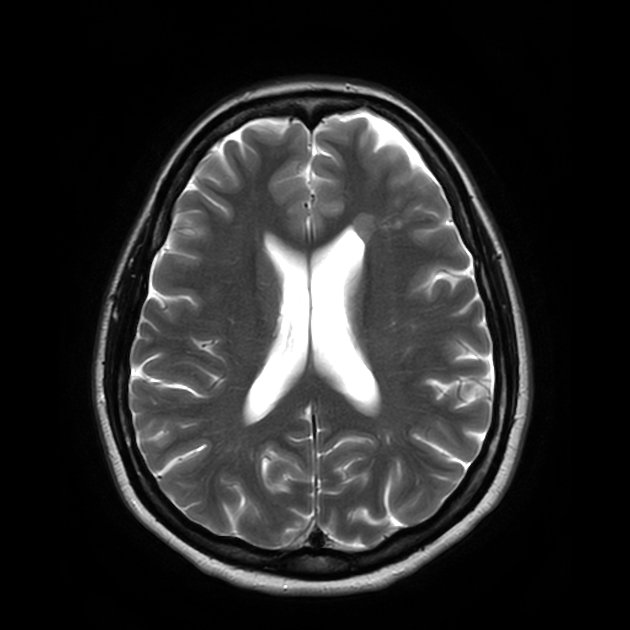
T2
hyperintense to adjacent white and grey matter
heterogeneity may be seen in larger lesions, occasionally with susceptibility-related signal dropout due to calcifications
no adjacent parenchymal edema or mass effect (as no brain invasion is present) 6
FLAIR: very bright signal 10
T1 C+ (Gd): usually no enhancement, although at times may demonstrate mild enhancement ref
DWI/ADC: facilitated diffusion with high ADC values 10
Angiography (DSA)
As expected from the histology, subependymomas show no or little vascularity 6.
Treatment and prognosis
If appearances are characteristic and the patient is asymptomatic, then follow up is a viable option.
Resection should be considered if the patient is symptomatic (hydrocephalus or mass effect), the mass has an atypical appearance or demonstrates growth. Local resection is curative and even debulking has an excellent outcome 8.
Differential diagnosis
General imaging differential considerations include other intraventricular neoplasms and lesions. A few specific lesions to consider include ref:
-
usually in children, or younger adults
heterogeneous enhancement
-
vividly enhancing
usually in children, or younger adults
in adults more common in the 4th ventricle
-
particularly if close to the septum pellucidum
overall less common
typically seen in younger patients (20-40 years of age)
ring-shaped lateral ventricular nodules: small lesions with a diameter <10 mm
subependymal giant cell astrocytomas and subependymal nodules: seen almost exclusively in patients with tuberous sclerosis






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.