 The Diagnostic Imaging Pathways App is an offline decision-support tool designed to help clinicians make appropriate medical imaging choices. This free resource is based upon the popular website of the same name. It's currently available for iOS, with an android version expected soon.
The Diagnostic Imaging Pathways App is an offline decision-support tool designed to help clinicians make appropriate medical imaging choices. This free resource is based upon the popular website of the same name. It's currently available for iOS, with an android version expected soon.
The App is divided into 12 subspecialty categories under which specific clinical pathways can be accessed to guide the user towards the most appropriate imaging test. An overview button allows each pathway to be visualised in its entirety at any time.
There are many things to like about this App, particularly the fact that it is a free resource made available globally. Trying to cover every single clinical scenario is however an impossible task and keeping pathways up to date and evidence based is going to prove a constant challenge.
In order to get an idea of the current status of this App and its potential for the future, we invited a group of radiologists on Twitter to take a look for us. We'd love to get your feedback too, which you can send to us through the comments section or via social media.
@DrAndrewDixon
Review:
This mobile application is a very useful tool which every hospital-based physician should have at hand in order to help them choose the most appropriate diagnostic approach. The form is very attractive but some of the content runs a bit behind, which is a little disappointing. The information in some pathways would benefit from more detailed and updated information.
The prostate pathway in particular seems very old fashioned. The initial recommended imaging modality is TRUS biopsy although many cancers are being missed using this technique. MRI is really of great added value in case of negative TRUS biopsies as tumours in the transition zone are easily missed, and this is not reflected in the pathway. And who is still performing endorectal MRI? The most appropriate pathway is normal (transabdominal) prostate MRI (preferably 3T).
Rating:


Review:
The app covers a broad selection of presentations across a number of paediatric specialties. The topics covered are representative of the majority of the presentations I see on a daily basis and the suggestions for imaging are relevant for the UK as well as Australia & New Zealand. The ability to see an overview of the guidance as well as having a pathway that requires interaction is helpful to gain an understanding of the whole pathway as well as the arm that you are using. Overall, I think that this will be a helpful resource for any healthcare professional who uses radiological services.
Rating:


Review:
A good start, but there’s a lot more work to do! The app was easy to use and graphics were cute. Overview of pathways was great to have. I do worry that this app could be perceived as evidence-based guidelines when there are actually major deficiencies. I found many of the head and neck pathways to be incomplete, too simplified or out of date.
I particularly disagree with the incidental thyroid nodule pathway which recommends either US or thyroid scintigraphy for all nodules depending on TSH. This approach is not cost-effective and can lead to harm from over-investigation and overdiagnosis. The approach in the ACR White Paper on Incidental Thyroid Findings should be used instead. There is also no mention of the use of 4D-CT in the hyperparathyroidism pathway and the radiation dose from parathyroid scintigraphy is much more than the 1-5mSv listed.
Rating:


Review:
The Diagnostic Imaging Pathways (DIP) app is visually pleasing and easy to navigate, with the pathway overview in particular being a handy feature. Some key guidelines are missing (e.g. anal cancer staging) and some take a path quite different to that in most UK centres (e.g. recommending both abdominal AXR and CT if acute diverticulitis is suspected, or contrast enhanced CT in renal colic if the patient is aged over 50). However, the concept is sound, and the app is technically well designed so I can see this being "spun off" in different countries to suit local needs.
Rating:


Review:
The diagnostic imaging pathways app has a very user friendly, easy and fast on the go interface. I tried various clinical scenarios, which I come across in day to day radiology practice. Some pathways work along the same line as we use India. Some of the pathways need updating, like the criteria for multiple sclerosis. The stroke pathway matches our evaluation steps. We use the ASPECTS score for MCA infarction and CT perfusion most often in the proper clinical scenario followed by extracranial carotid angiography. Overall I think the pathways are useful but further additions and updating are required.
Rating:


Review:
The DIP website and smartphone app are designed assist clinicians with a) choosing the best imaging tests for their patient, and b) adjusting patient management depending of the test result. Among the sixteen pathways in the O&G section, there are some that achieve this very well. For example, “Adnexal masses” and “Bleeding in early pregnancy” are excellent, detailed and current pathways. Several others however are less satisfying because they’re either too brief, or do not clearly define the role of imaging. Interestingly, the website flags many of these as “due for review October 2015”. I am looking forward to seeing the updates.
The transition from website to app is a great idea, and the app menu interface is nicely presented. I would have liked to see more focus on the “Pathway Overview”, rather than multi-page decision making tool, which is a little clumsy. The best bits on the website are the pearls of wisdom in the hover boxes on the pathway overview page, and these are lost in the app version. Overall – great concepts, impressive breadth – with room for improvement for content and app usability.
Rating:




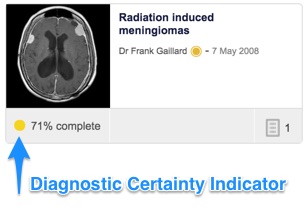






 We have instituted a unique radiopaedia ID (rID) for all cases and exposed this in our case information box (to the right of the case images).
We have instituted a unique radiopaedia ID (rID) for all cases and exposed this in our case information box (to the right of the case images). 






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.