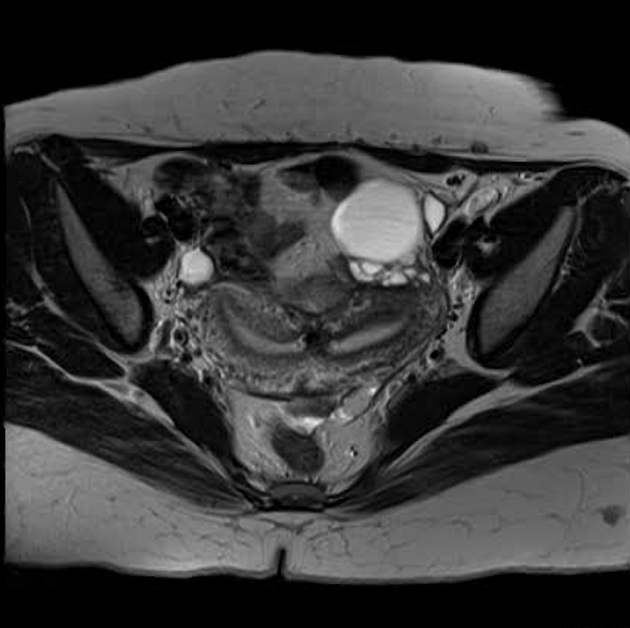
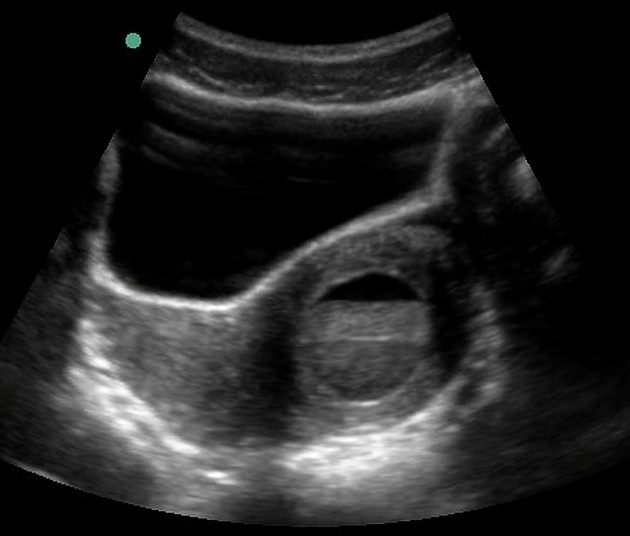
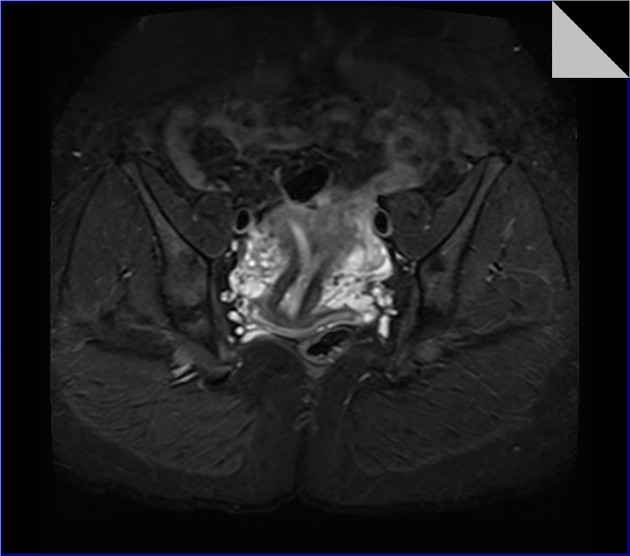
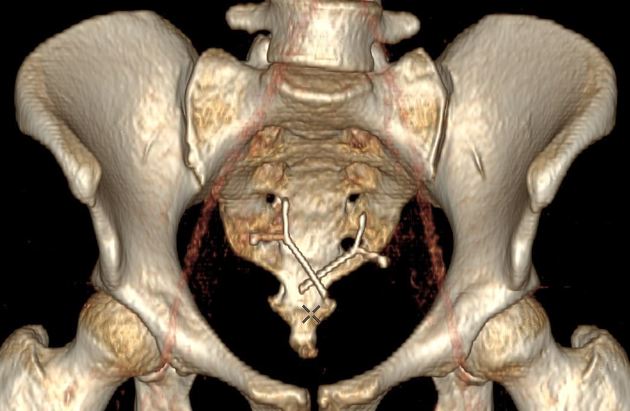
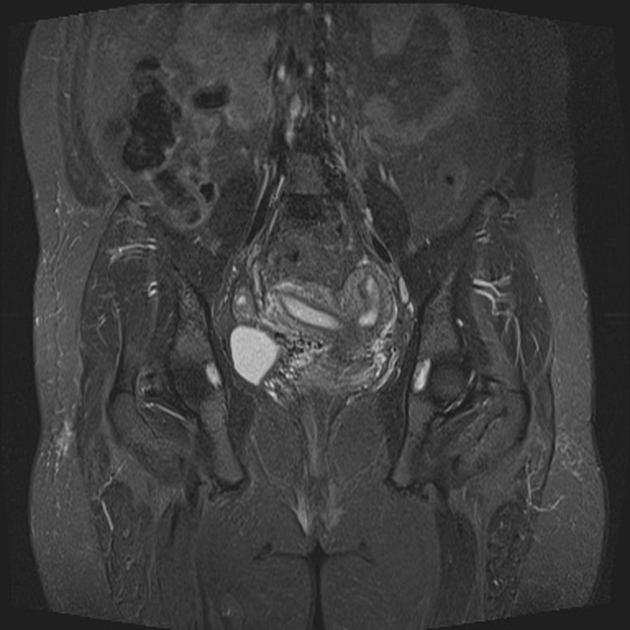
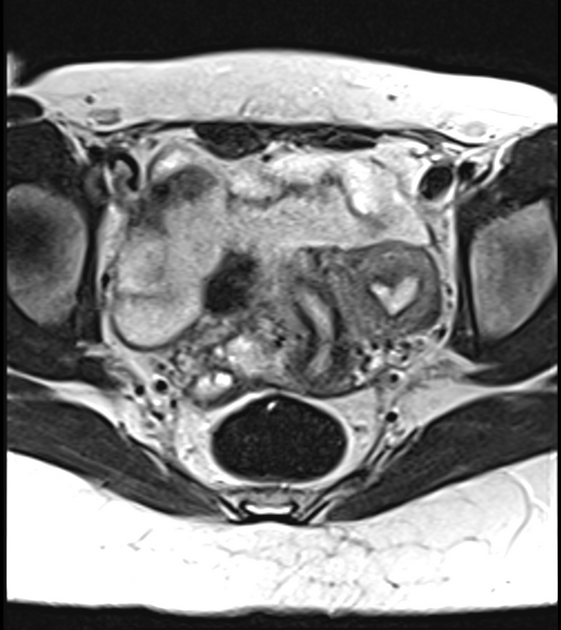
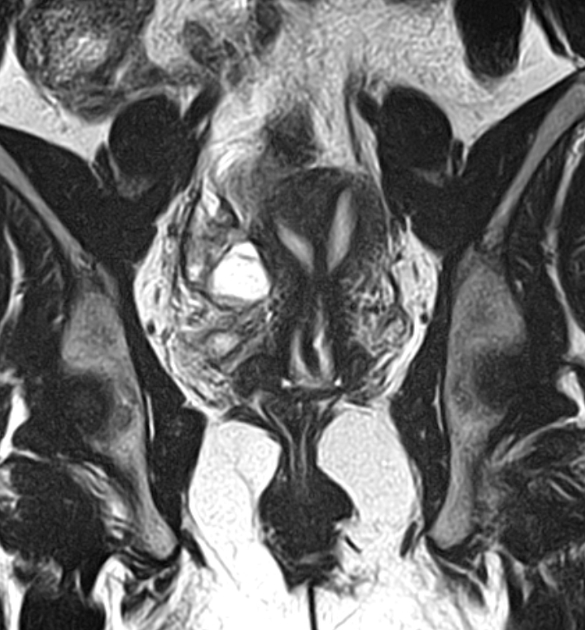
Bicornuate uterus
Citation, DOI, disclosures and article data
At the time the article was created Frank Gaillard had no recorded disclosures.
View Frank Gaillard's current disclosuresAt the time the article was last revised Arlene Campos had no financial relationships to ineligible companies to disclose.
View Arlene Campos's current disclosures- Bicornuate uteri
- Bicornuate womb
A bicornuate uterus is a type of uterine duplication anomaly. It can be classified as a class IV Mullerian duct anomaly.
On this page:
Epidemiology
Overall, congenital uterine anomalies occur in ~1.5% of females (range 0.1-3%). Bicornuate uteri are thought to represent ~25% (range 10-39%) of Mullerian duct anomalies 6,9.
Associations
a longitudinal vaginal septum may be present in ~25% of cases
as with other Mullerian duct anomalies, abnormalities of the renal tract may also be present
Clinical presentation
In most cases, a bicornuate uterus is incidentally discovered when the pelvis is imaged. The most common symptomatic presentation is with early pregnancy loss and cervical incompetence 6. Infertility is not usually a problem with this type of malformation because implantation of the embryo is not impaired.
Pathology
A bicornuate uterus results from abnormal development of the paramesonephric ducts. There is a partial failure of fusion of the ducts, resulting in a uterus divided into two horns.
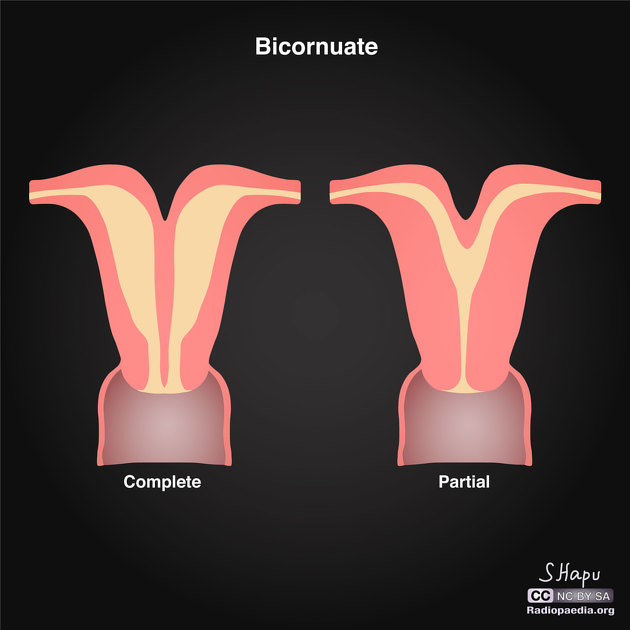
Subtypes
A bicornuate uterus is divided according to the involvement of the cervical canal:
bicornuate bicollis: two cervical canals; central myometrium extends to the external cervical os
bicornuate unicollis: one cervical canal; central myometrium extends to the internal cervical os
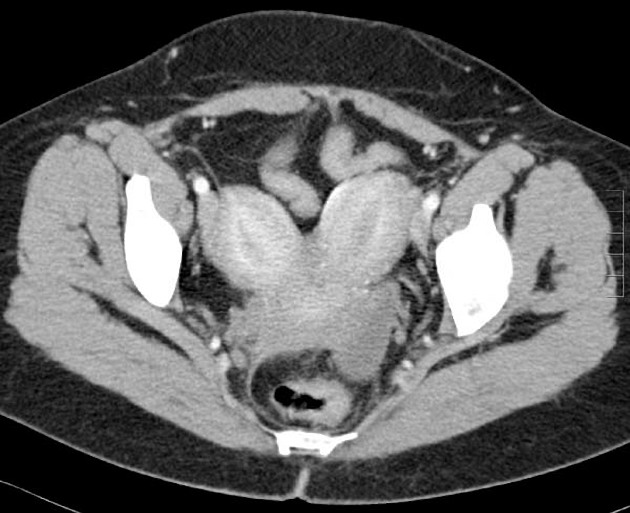
Radiographic features
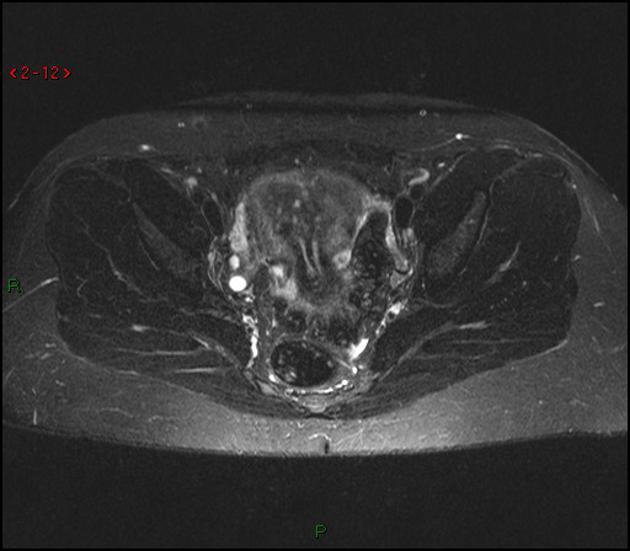
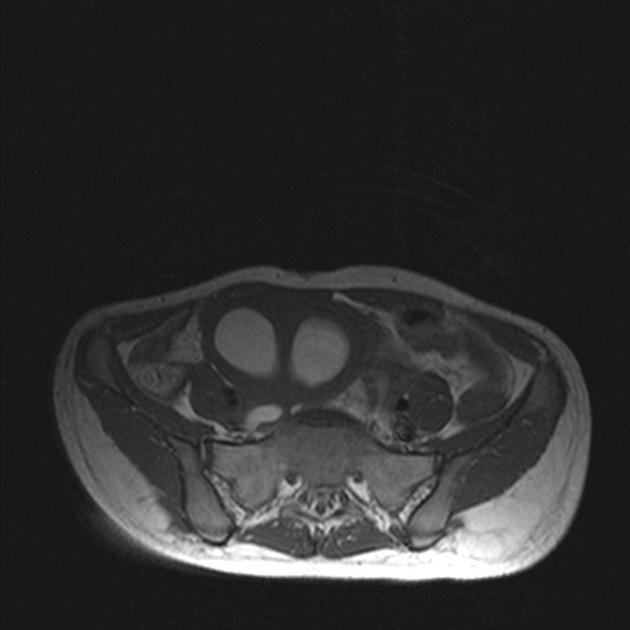
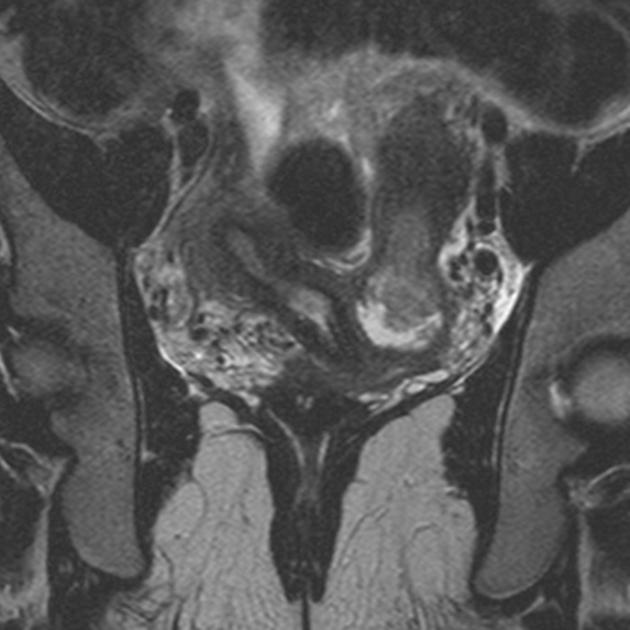
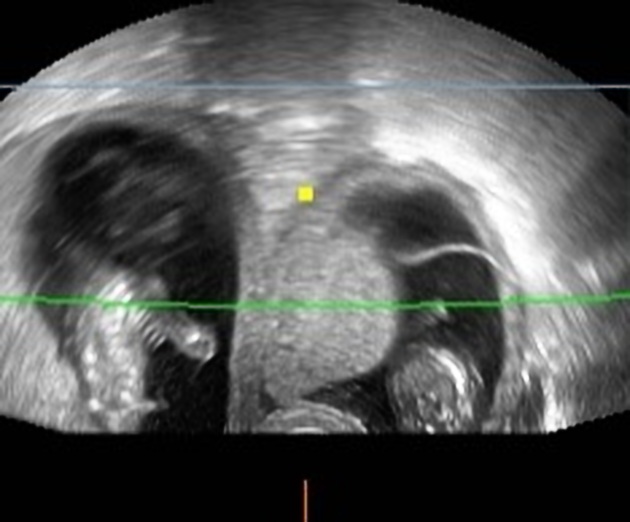
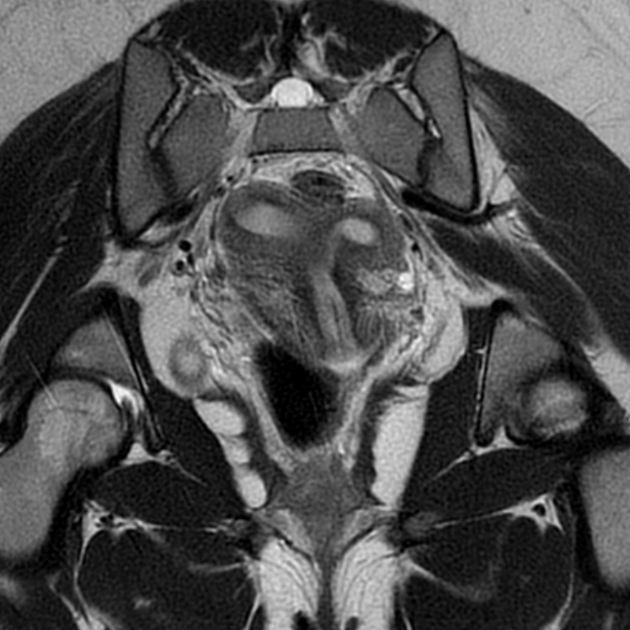
The preferred methods of imaging uterine anomalies are ultrasound, hysterosalpingogram or MRI. The external uterine contour is concave or heart-shaped, and the uterine horns are widely divergent. The fundal cleft is typically more than 1 cm deep and the intercornual distance is widened.
The uterus is seen as comprising caudally fused symmetric uterine cavities with some degree of communication between the two cavities (usually at the uterine isthmus). Although not a specific finding, the angle between the horns of the bicornuate uterus is usually more than 105° 3.
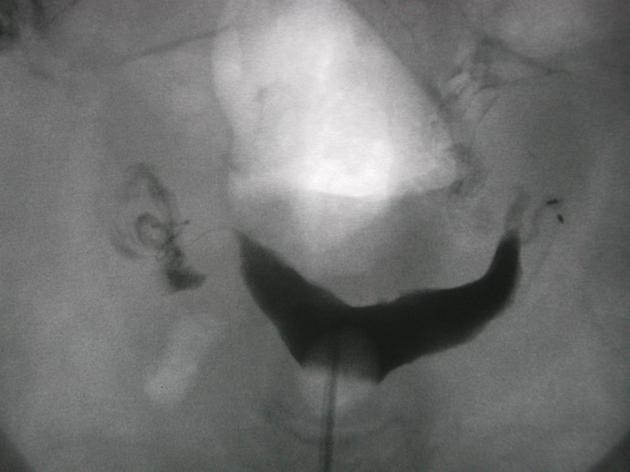
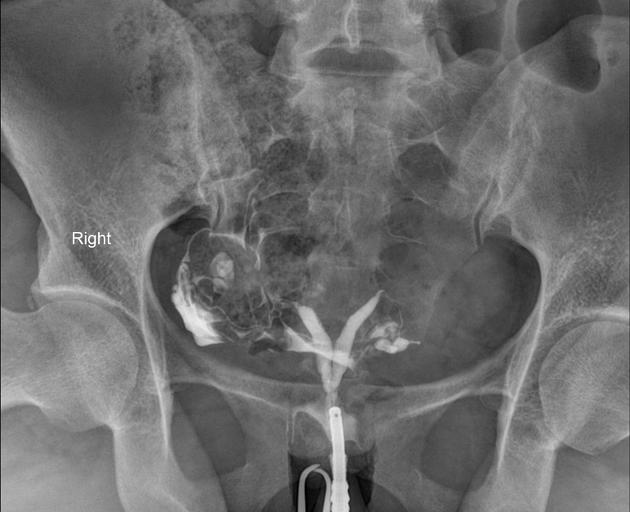
Fluoroscopy
A divided uterus can be seen on hysterosalpingogram (HSG), but it is difficult to differentiate between septate and bicornuate anomalies since the uterine fundal contour is not visible 5. Accuracy of hysterosalpingogram alone is only 55% in differentiation between both entities. An angle of less than 75° between the uterine horns is suggestive of a septate uterus while an angle of more than 105° is more consistent with a bicornuate uterus.
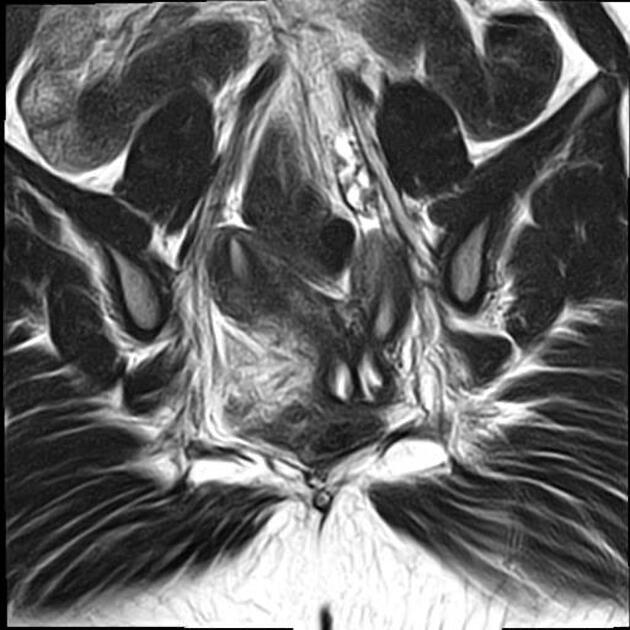
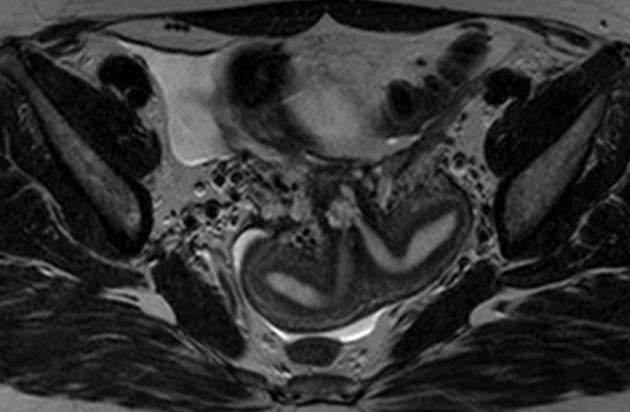
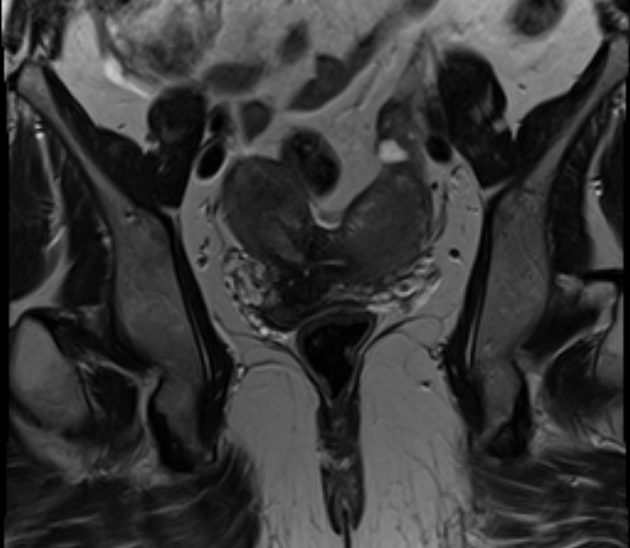
MRI
May help confirm anatomy by showing a deep (>1 cm) fundal cleft in the outer uterine contour and an intercornual distance of >4 cm. The uterus demonstrates normal uterine zonal anatomy.
Treatment and prognosis
Surgical intervention is usually not indicated in the absence of reproductive difficulties.
In women with a history of recurrent pregnancy loss and in whom no other infertility issues have been identified a Strassman metroplasty can be considered.
In patients with cervical incompetence, placement of a cervical cerclage may increase fetal survival rates 9. Indeed, the association between cervical incompetence and a bicornuate uterus is so high, that prophylactic cerclage may be appropriate in some instances.
Differential diagnosis
uterus didelphys: complete failure of fusion occurs during the development of the paramesonephric ducts with duplication of the uterus, cervix and vagina
septate uterus: has a normal fundal contour but is characterised by a persistent longitudinal septum that partially divides the uterine cavity 12
Practical points
Septate uterus increases the risk of early pregnancy loss, and hysteroscopic intervention to resect the septum is sometimes pursued. In this situation, differentiation between a septate uterus or a bicornuate uterus is critical. This is mostly a problem with HSG preoperative evaluation. Attempted resection of a bicornuate uterus "septum" leads to a poor outcome.
Quiz questions
References
- 1. Wolfgang Dähnert. Radiology Review Manual. (2003) ISBN: 9780781738958 - Google Books
- 2. Karen L. Reuter, T. Kemi Babagbemi. Obstetric and Gynecologic Ultrasound. (2007) ISBN: 0323039766 - Google Books
- 3. Ly JQ. Rare bicornuate uterus with fibroid tumors: hysterosalpingography-MR imaging correlation. AJR Am J Roentgenol. 2002;179 (2): 537-8. AJR Am J Roentgenol (full text) - Pubmed citation
- 4. Mueller G, Hussain H, Smith Y et al. Müllerian Duct Anomalies: Comparison of MRI Diagnosis and Clinical Diagnosis. AJR Am J Roentgenol. 2007;189(6):1294-302. doi:10.2214/AJR.07.2494 - Pubmed
- 5. Steinkeler J, Woodfield C, Lazarus E, Hillstrom M. Female Infertility: A Systematic Approach to Radiologic Imaging and Diagnosis. Radiographics. 2009;29(5):1353-70. doi:10.1148/rg.295095047 - Pubmed
- 6. Troiano R & McCarthy S. Mullerian Duct Anomalies: Imaging and Clinical Issues. Radiology. 2004;233(1):19-34. doi:10.1148/radiol.2331020777 - Pubmed
- 7. Dykes T, Siegel C, Dodson W. Imaging of Congenital Uterine Anomalies: Review and Self-Assessment Module. AJR Am J Roentgenol. 2007;189(3_supplement):S1-S10. doi:10.2214/ajr.06.0821
- 8. Mintz M, Thickman D, Gussman D, Kressel H. MR Evaluation of Uterine Anomalies. AJR Am J Roentgenol. 1987;148(2):287-90. doi:10.2214/ajr.148.2.287 - Pubmed
- 9. Nahum GG. Uterine anomalies. How common are they, and what is their distribution among subtypes? J Reprod Med. 1998;43 (10): 877-87. - Pubmed citation
- 10. Chan Y, Jayaprakasan K, Zamora J, Thornton J, Raine-Fenning N, Coomarasamy A. The Prevalence of Congenital Uterine Anomalies in Unselected and High-Risk Populations: A Systematic Review. Hum Reprod Update. 2011;17(6):761-71. doi:10.1093/humupd/dmr028 - Pubmed
- 11. Imaoka I, Wada A, Matsuo M et-al. MR imaging of disorders associated with female infertility: use in diagnosis, treatment, and management. Radiographics. 23 (6): 1401-21. doi:10.1148/rg.236025115 - Pubmed citation
- 12. Chaudhry S. AJR Teaching File: infertility in a young woman. AJR Am J Roentgenol. 2007;189 (3): S11-2. doi:10.2214/AJR.07.7019 - Pubmed citation
- 13. Abo Dewan K, Hefeda M, ElKholy D. Septate or Bicornuate Uterus: Accuracy of Three-Dimensional Trans-Vaginal Ultrasonography and Pelvic Magnetic Resonance Imaging. The Egyptian Journal of Radiology and Nuclear Medicine. 2014;45(3):987-95. doi:10.1016/j.ejrnm.2014.04.001
- 14. Zakarin Safier L & Rackow B. Bicornuate Uterus. Congenital Müllerian Anomalies. 2016;:95-104. doi:10.1007/978-3-319-27231-3_8
Incoming Links
- Hand-foot-genital syndrome
- Uterine duplication anomalies
- Asplenia syndrome
- Anterior sacral meningocele
- Septate uterus
- Bicornuate uterus
- Müllerian duct anomalies
- AFS classification of Müllerian anomalies
- Cornual ectopic pregnancy
- Haematometrocolpos
- Interstitial ectopic pregnancy
- Unicornuate uterus
- Bands in gestational sacs
- Incarcerated uterus
- Arcuate uterus
- Ectopic ovary
- Congenital utero-vaginal anomalies
- Uterus didelphys
- Alphabet inspired signs
- Abnormally eccentric gestational sac
- Septate uterus
- Septate uterus
- Bicornuate uterus
- Bicornuate uterus
- Bicornuate uterus
- Partial bicornuate uterus
- Septate uterus
- Bicornuate uterus
- Bicornuate uterus
- Subseptate uterus
- Bicornuate uterus
- Bicornuate vs septate uterus (hysterosalpingogram)
- Bicornuate uterus with pregnancy
- Bicornuate uterus
- Bicornuate unicollis uterus
- Bicornuate, unicollis uterus
- Arcuate uterus
- Bicornuate uterus
- Bicornuate uterus
- Septate uterus
Related articles: Anatomy: Abdominopelvic
- skeleton of the abdomen and pelvis
- muscles of the abdomen and pelvis
- spaces of the abdomen and pelvis
- anterior abdominal wall
- posterior abdominal wall
- abdominal cavity
- pelvic cavity
- perineum
- abdominal and pelvic viscera
- gastrointestinal tract
- spleen
- hepatobiliary system
-
endocrine system
-
adrenal gland
- adrenal vessels
- chromaffin cells
- variants
- pancreas
- organs of Zuckerkandl
-
adrenal gland
-
urinary system
-
kidney
- renal pelvis
- renal sinus
- avascular plane of Brodel
-
variants
- number
- fusion
- location
- shape
- ureter
- urinary bladder
- urethra
- embryology
-
kidney
- male reproductive system
-
female reproductive system
- vulva
- vagina
- uterus
- adnexa
- Fallopian tubes
- ovaries
- broad ligament (mnemonic)
- variant anatomy
- embryology
- blood supply of the abdomen and pelvis
- arteries
-
abdominal aorta
- inferior phrenic artery
- coeliac artery
- superior mesenteric artery
- middle suprarenal artery
- renal artery (variant anatomy)
- gonadal artery (ovarian artery | testicular artery)
- inferior mesenteric artery
- lumbar arteries
- median sacral artery
-
common iliac artery
- external iliac artery
-
internal iliac artery (mnemonic)
- anterior division
- umbilical artery
- superior vesical artery
- obturator artery
- vaginal artery
- inferior vesical artery
- uterine artery
- middle rectal artery
-
internal pudendal artery
- inferior rectal artery
-
perineal artery
- posterior scrotal artery
- transverse perineal artery
- artery to the bulb
- deep artery of the penis/clitoris
- dorsal artery of the penis/clitoris
- inferior gluteal artery
- posterior division (mnemonic)
- variant anatomy
- anterior division
-
abdominal aorta
- portal venous system
- veins
- anastomoses
- arterioarterial anastomoses
- portal-systemic venous collateral pathways
- watershed areas
- arteries
- lymphatics
- innervation of the abdomen and pelvis
- thoracic splanchnic nerves
- lumbar plexus
-
sacral plexus
- lumbosacral trunk
- sciatic nerve
- superior gluteal nerve
- inferior gluteal nerve
- nerve to piriformis
- perforating cutaneous nerve
- posterior femoral cutaneous nerve
- parasympathetic pelvic splanchnic nerves
- pudendal nerve
- nerve to quadratus femoris and inferior gemellus muscles
- nerve to internal obturator and superior gemellus muscles
- autonomic ganglia and plexuses
Related articles: Pathology: Genitourinary
- obstetrics
-
first trimester
- ultrasound findings in early pregnancy
- embryo/fetus
- beta-hCG levels
- confirming intrauterine gestation
- pregnancy of unknown location (PUL)
- first trimester vaginal bleeding
- early structural scan
- aneuploidy testing
-
second trimester
- fetal biometry
- amniotic fluid volume
- fetal morphology assessment
- soft markers
- amnioreduction
- Doppler ultrasound
- nuchal translucency
- 11-13 weeks antenatal scan
- chorionic villus sampling (CVS) and amniocentesis
- other
- placenta
- placental anatomy
- placental developmental abnormalities
- placenta praevia
- spectrum of abnormal placental villous adherence
- abnormalities of cord insertion
- abruptio placentae
- placental pathology
- vascular pathologies of placenta
- placental infections
- placental masses
- molar pregnancy
- twin placenta
- miscellaneous
-
first trimester
- gynaecology
- acute pelvic pain
- chronic pelvic pain
- uterus
- ovaries
- ovarian follicle
- ovarian torsion
- pelvic inflammatory disease
- ovarian cysts and masses
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervix
- fallopian tube
- other
- male genital tract
- prostate gland
- transrectal ultrasound
- prostate tumours
- infections of the prostate
-
prostatitis
- acute bacterial prostatitis
-
chronic prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- granulomatous prostatitis
- emphysematous prostatitis
- prostatic abscess
-
prostatitis
- benign prostatic hypertrophy
- cystic lesions of the prostate
- prostatic calcification
- prostatic infarction
- testes
-
unilateral testicular lesion
- testicular torsion
- orchitis
- testicular trauma
-
germ cell tumours of the testis
- testicular seminoma
-
non seminomatous germ cell tumours
- mixed germ cell tumour
- yolk sac tumour (endodermal sinus tumour)
- embryonal cell carcinoma
- choriocarcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumour
- sex cord / stromal tumours of the testis
- testicular cyst
- testicular lymphoma
- bilateral testicular lesion
- paratesticular lesions
- epididymis
- other
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord
- fibrous pseudotumour of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumours (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
-
unilateral testicular lesion
- penis
- prostate gland
- KUB
- kidneys
- normal renal anatomy
- hydronephrosis
- urolithiasis
- renal masses
- renal cystic disease
- renal infection
- vascular
- trauma
- ureter
- normal ureter anatomy
- ureteral stricture
- ureteral dilatation
- ureteral anomalies
- ureteral tumours
- ureteral trauma
- other
- bladder
- kidneys























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.