Deep vein thrombosis (DVT) most commonly occurs in the lower limbs, however, are not uncommon in the upper limb and neck deep veins. Other types of venous thrombosis, such as intra-abdominal and intracranial, are discussed in separate articles.
On this page:
Terminology
The term indeterminate (equivocal) DVT is preferred over subacute DVT when the ultrasound features are of neither acute DVT nor chronic post-thrombotic change (although subacute DVT can be used in the follow-up of a known acute DVT). The term chronic post-thrombotic change is preferred over chronic or residual DVT to prevent overtreatment with anticoagulation 7,8.
Epidemiology
1.6 new cases per 1000 per year
2.5-5% of the population is affected
>50% have long terms symptoms of post-thrombotic syndrome
6% of DVT patients report eventual venous ulcers (0.1% general population)
Risk factors
age (relative risk increase ~2 per 10-year increase)
surgery (orthopedic patients at highest risk: hip 48%, knee 61%)
trauma
history of venous thromboembolism (2-9% increase)
-
primary hypercoagulable states
factor V Leiden (heterozygous 8-fold increased risk, homozygous 80-fold increased risk)
estrogen replacement (2-4-fold increased risk)
immobilization (2-fold increased risk)
-
pregnancy (0.075% of pregnancies)
greatest risk is in the postpartum period, risk returns to baseline 6 weeks after delivery 9
malignancy (4-6-fold increased risk)
in-dwelling vascular device (e.g. PICC (line) and upper limb DVT) 6
Clinical presentation
In the lower limbs, patients often present with unilateral leg pain, swelling, and erythema. On physical examination, the affected leg is often tender and warm, and there may be dilation of superficial veins. Additionally, some patients may have a positive Homan sign on physical examination, whereby there is pain on forceful dorsiflexion while the knee is extended.
The Wells score for DVT, a clinical decision rule, can help to stratify risk in patients presenting with symptoms of acute DVT 8,10.
Pathology
The majority of lower extremity DVTs develop in the veins of the calf, namely the peroneal veins, posterior tibial veins and the veins of the gastrocnemius and soleus muscles 10,11. The soleal veins are effectively valveless and are the likely site of origin of relatively asymptomatic free-floating propagating thrombus that can detach to cause massive pulmonary embolus 13.
Thromboembolic disease is now regarded as a systemic disease promoted by age, diabetes and other factors and caused by endothelial dysfunction which allows clot to form, as well as inflammation and flow disturbance.
Markers
In patients deemed to "unlikely" have a DVT via the Wells score, a negative d-dimer can safely exclude acute DVT 8,10.
Radiographic features
Complete duplex ultrasound is the imaging modality of choice 8.
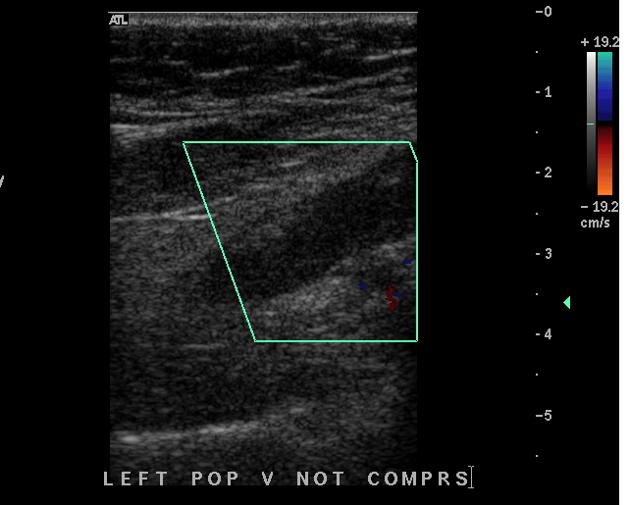
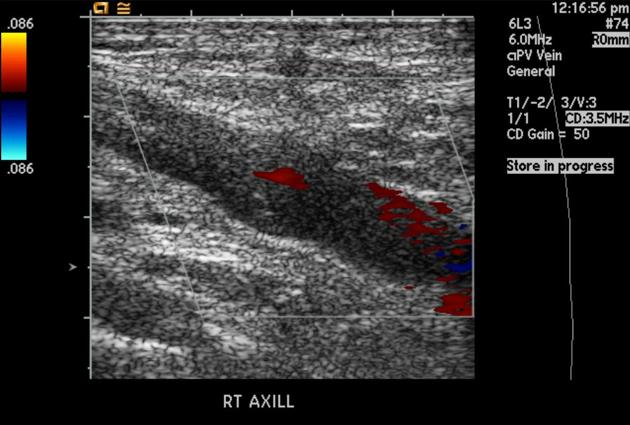
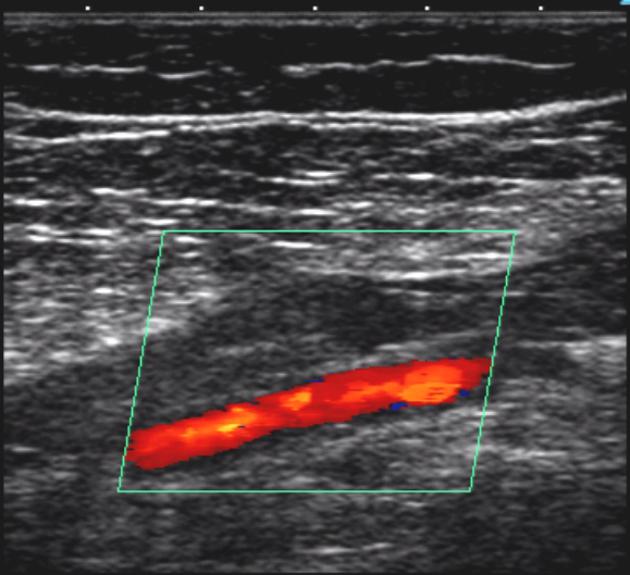
Ultrasound
-
general features
non-compressible venous segment
loss of phasic flow on Valsalva maneuver
absent color flow if completely occlusive
lack of flow augmentation with calf squeeze
increased flow in superficial veins
-
acute thrombus
increased venous diameter
soft/deformable intraluminal material
smooth surface
occasionally free-floating proximal propagation at risk of detachment
-
chronic post-thrombotic change
normal or decreased venous diameter
rigid intraluminal material
irregular surface
synechiae or bands
calcifications (rare)
+/- acute thrombus
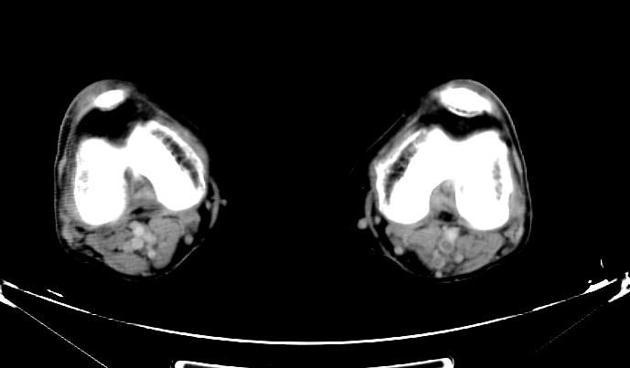
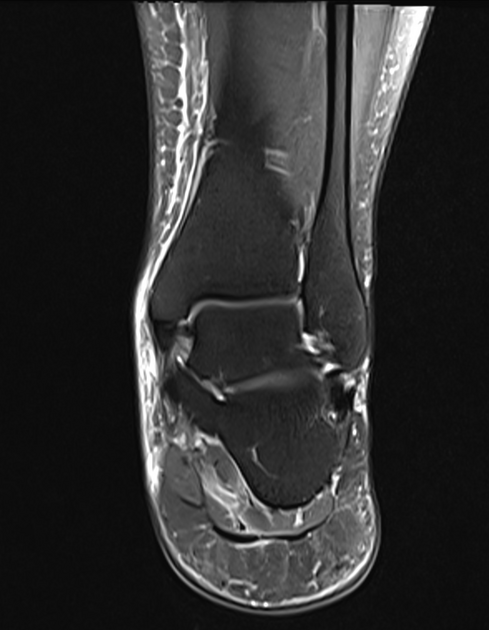
MRI
Vascular structures should always be interrogated during routine assessment of the peripheries and pelvis. Incidental DVT has a prevalence of around 0.3% on routine outpatient knee MRI 4:
luminal abnormalities (abnormal flow voids or filling defects)
vein wall thickening
perivascular edema
perifascial edema
local intramuscular T2/PD hyperintensity
subcutaneous edema
dermal thickening (related to venous obstruction)
Treatment and prognosis
Treatment is with anticoagulation, often for at least 3 months in duration 5.
Complications
Practical points
"above knee DVT", or proximal DVT, is a lower limb DVT involving the popliteal vein or more proximal veins 5
upper limb/extremity DVT involves the radial, ulnar, brachial, axillary, subclavian, internal jugular and/or brachiocephalic veins 12








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.