Haemangioblastomas are tumours of vascular origin and occur both sporadically and in patients with von Hippel Lindau disease. They are WHO grade 1 tumours, which can occur in the central nervous system or elsewhere in the body, including kidneys, liver, and pancreas.
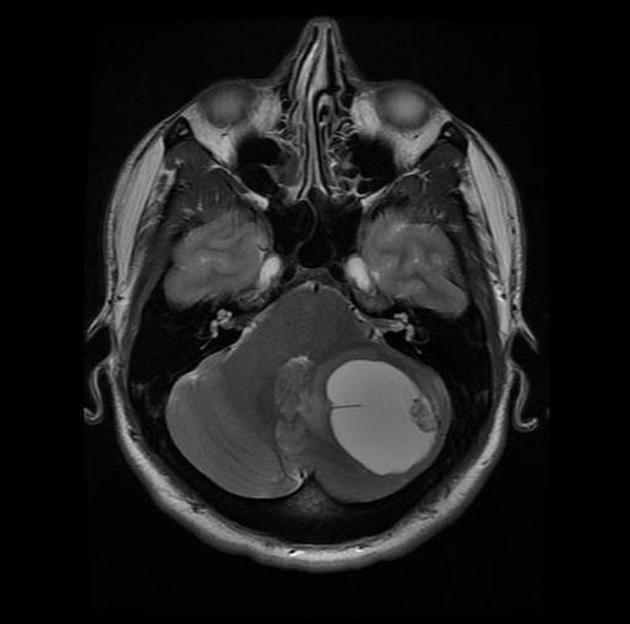
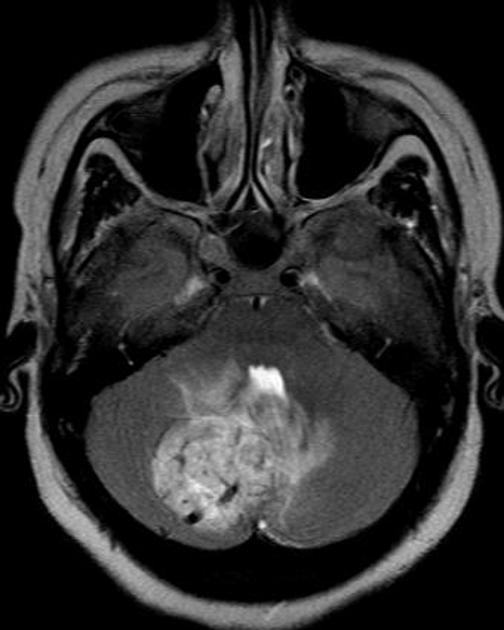
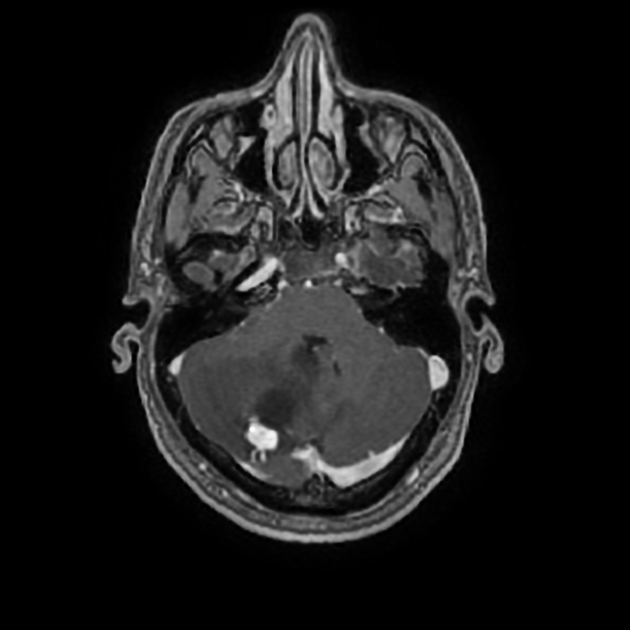
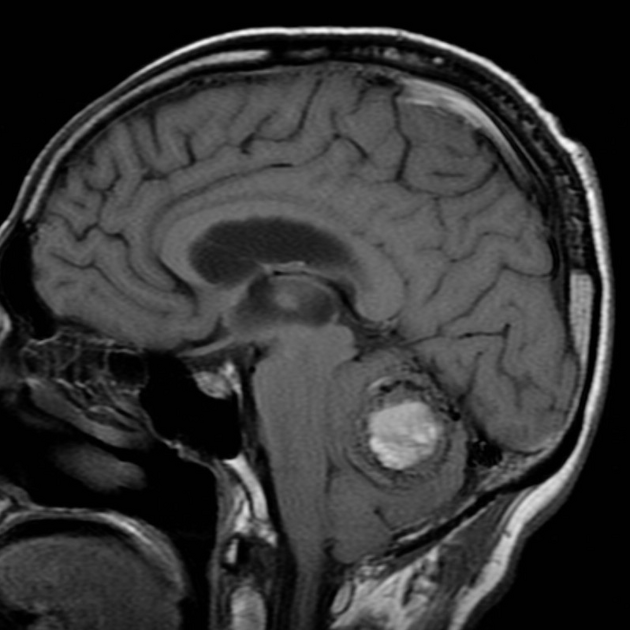
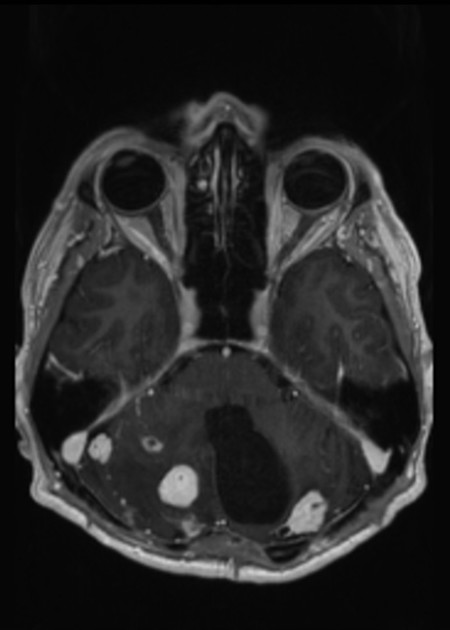
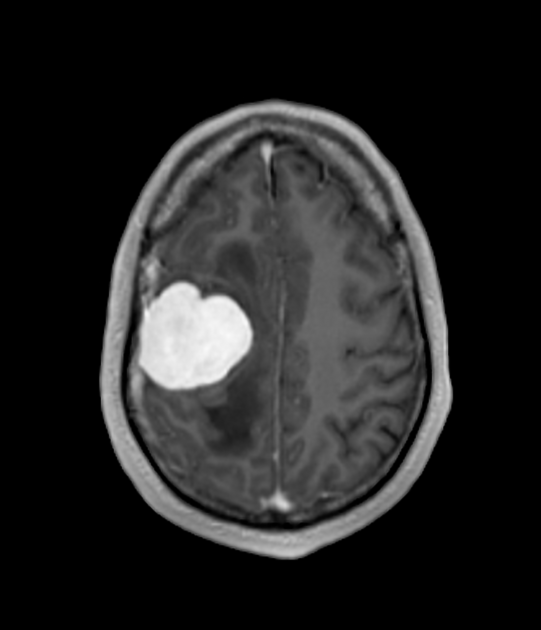
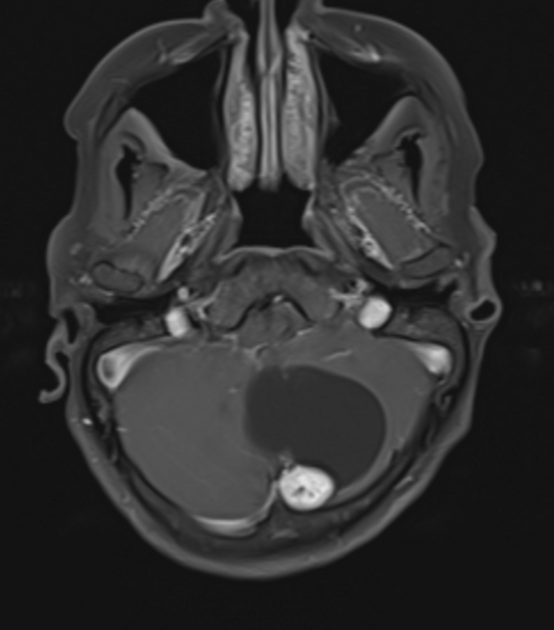
These tumours generally present on imaging as sharply demarcated homogeneous masses comprising a cyst with non-enhancing walls and a mural nodule which vividly enhances, often with prominent serpentine flow voids.
On this page:
Epidemiology
Haemangioblastomas typically occur in young to middle-aged adults and, although they are the most common primary intra-axial infratentorial tumour in this demographic, they are nonetheless uncommon in absolute terms. They are estimated to account for only 1-2.5% of all intracranial tumours 3,4 and approximately 10% of all posterior fossa tumours 4:
slight male predilection in adults: M: F ratio of 1.3-2.6:1 4
peak incidence at around 30-60 years of age, but earlier in patients with von Hippel Lindau disease
sporadic cases make up approximately 75-80%, with the remainder being found in patients with von Hippel Lindau disease
Clinical presentation
Most frequently present with symptoms relating to:
headaches: 70% 4
hydrocephalus and symptoms of raised intracranial pressure: 50% 4
cerebellar dysfunction: ~50-60% 3
altered mental state: 10%
polycythaemia due to erythropoietin production occurs in ~20% (range 5-40%) of cases 3,4
One study showed that in patients with von Hippel Lindau disease, the onset of symptoms usually coincides with the development of the cystic component, and that solid cerebellar nodules were mostly well-tolerated. They suggested repeat imaging at this stage to document the size of the cyst and to plan tumour excision 7.
Acute presentation due to significant haemorrhage is uncommon and tends to be seen in larger tumours (>1.5 cm) 5,6.
Pathology
A haemangioblastoma is actually a capillary haemangioma and, despite the name with the suffix of "blastoma", it is a low grade (WHO grade 1) lesion. The tumour is usually a well-circumscribed, highly vascular nodule almost always abutting the pial layer.
Cystic components are common, and can either be peritumoural or intratumoural. Cyst fluid is similar to plasma and most likely arises by exudation from the vascular component of the solid nodule, likely driven primarily by vascular endothelial growth factor (VEGF) that is secreted by the tumour and has a powerful effect on vascular permiability 4,9,13,14.
Peritumoural cysts, lacking any peripheral enhancement, are usually lined by reactive gliosis rather than tumour and are not actually part of the tumour 13. It has, therefore, been suggested that resection of the wall of these peritumoural cystic components need not be carried out. This has not been supported in a number of other studies, however 8,9 (a similar discussion is present in the pilocytic astrocytoma literature).
Cysts that are within the solid nodule, or seemingly peritumoural cysts but that have peripheral enhancement, are presumably part of the tumour and should, therefore, be resected. The origin of thse intratumoural cysts is unclear. It may represents a sequelae of intramedullary haematopoiesis within haemangioblastomas 13 and may account for the xanthochromic appearance of the cyst fluid 4.
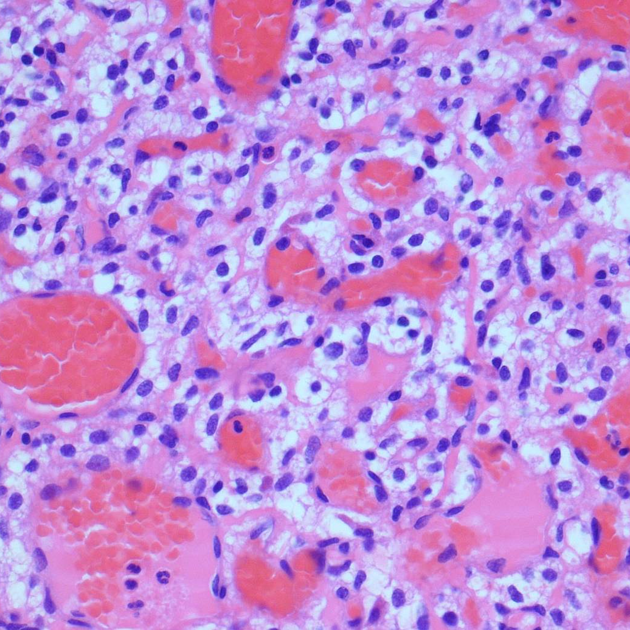
Microscopic appearance
Microscopy reveals a very vascular tumour composed of two components: neoplastic stromal cells and reactive vascular cells 10. The proportion of these two components is variable. A typical and characteristic finding is of thin-walled vessels with surrounding stroma of connective tissue and polygonal lipid-laden 'stromal cells' 4.
Location
Haemangioblastomas can arise in all parts of the central nervous system, however, they have a strong predilection for the cerebellum and spinal cord 4,12.
cerebellum: 45-65%
spinal cord: 3-36%
cauda equina: 11%
brainstem: 5%
supratentorial: 1% (mostly patients with von Hippel-Lindau disease)
Associations
multiple renal cell carcinomas
-
von Hippel Lindau (vHL) disease
~45% of those with von Hippel Lindau disease develop haemangioblastomas
~20% of those with haemangioblastoma have von Hippel Lindau disease
polycythaemia: due to secretion of erythropoietin from lesions
Radiographic features
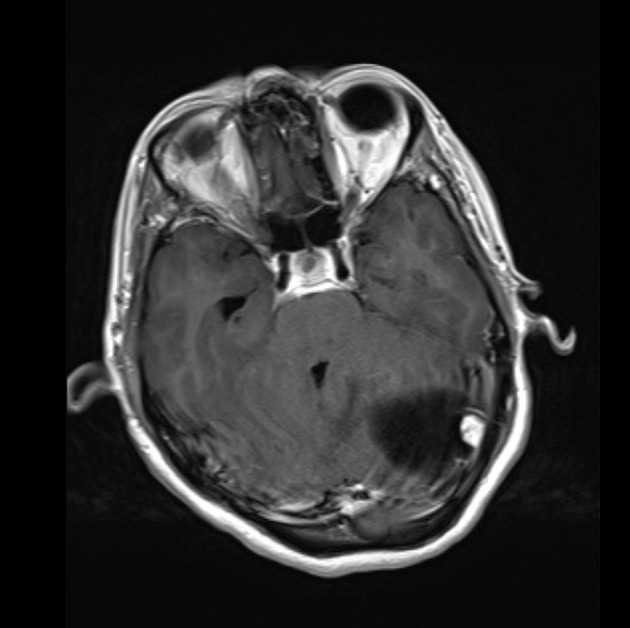
Haemangioblastomas can present with a variety of morphologies. Most commonly (60%) they consist of a large cyst with a vividly enhancing mural nodule which often has prominent serpentine flow voids 2,11. Somewhat less commonly (40%) tumour is solid with no associated cyst 4. The solid component may have smaller cystic spaces within it and often abutts the pia mater.
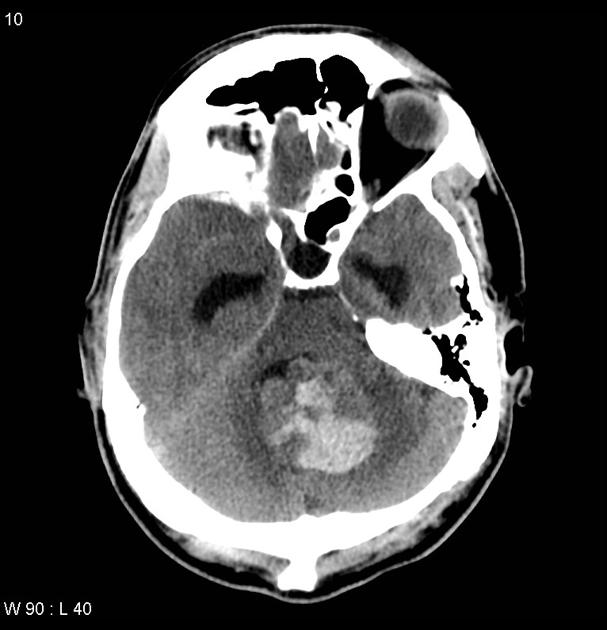
CT
the mural nodule is isodense to the brain on non-contrast scans, with fluid density surrounding cyst
postcontrast intense homogeneous enhancement of the mural nodule
the cyst walls usually do not enhance
calcification is not present
MRI
-
T1
hypointense to isointense mural nodule
CSF signal cyst content
-
T1 C+ (Gd)
mural nodule vividly enhances 2,4
cyst wall usually does not enhance, but enhancement may occasionally be present 4,11
-
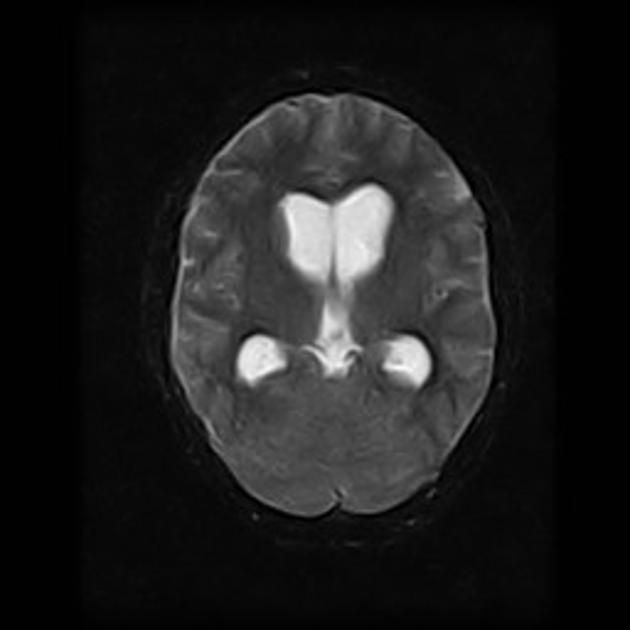
T2
hyperintense mural nodule
flow voids due to enlarged vessels may be evident, especially at the periphery of the cyst; seen in 60-70% of cases 4
fluid-filled cyst, similar to CSF
MR perfusion imaging: high rCBV ratios
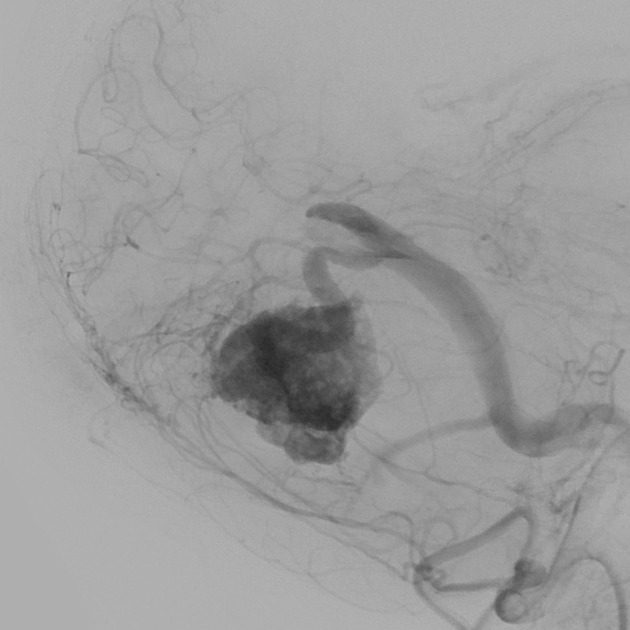
Angiography (DSA)
Enlarged feeding arteries and often dilated draining veins are demonstrated, with a dense tumour blush centrally 4.
Treatment and prognosis
Surgical resection is usually curative, and with large lesions may be facilitated by preoperative embolisation. Simple cyst drainage appears to be insufficient for definitive management. Adjuvant radiotherapy may be used in patients with incomplete resections. Recurrence is seen in up to 25% of patients 3.
In tumours that have a cyst, provided the cyst wall does not enhance, only resecting the mural nodule is generally considered preferable. If the cyst wall enhances, then resection of this component also is necessary to avoid recurrence 11.
It is important to screen for von Hippel Lindau disease and if positive, screen other organ systems for associated pathologies.
Differential diagnosis
General imaging differential considerations include:
brain metastases: although single posterior fossa metastases are uncommon they are still the most common diagnosis if the patient is middle-aged or older
-
mostly in children
can appear very similar
more likely to have enhancing cyst wall
less likely to have flow voids
glioblastoma or high-grade astrocytoma with piloid features in adults
-
vascular lesions
arteriovenous malformation with subacute bleed
cavernoma with subacute bleed
subacute infarction
-
more common in childhood
usually solid without cysts
restricted diffusion (small round blue cell tumour)
less likely to have flow voids























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.