Herpes simplex encephalitis
Updates to Article Attributes
Herpes simplex (HSV) encephalitis is the most common cause of fatal sporadic fulminant necrotizing viral encephalitis and has characteristic imaging findings.
Two subtypes are recognised which differ in demographics, virus and pattern of involvement. They are 1:
- neonatal herpes encephalitis
- childhood and adult herpes encephalitis
This article concerns itself with the latter. For a discussion of the former, please refer to the article neonatal herpes simplex encephalitis.
Epidemiology
Childhood and adult herpes encephalitis is usually due to HSV-1 (90%) with the rest due to HSV-2 5. There is no particular age, sex or seasonal predilection.
Clinical presentation
Presentation is unfortunately relatively non-specific consisting of fever, headaches, focal neurological deficits, seizures, and altered or decreased level of conciousness.
Diagnosis is established with PCR of CSF, although the combination of clinical scenario, CSF demonstrating pleocytosis and elevated protein, and appropriate imaging is usually highly suggestive and permits commencement of treatment.
Pathology
HSV is an obligatory intracelluar virus which enters via infecting nasopharyngeal cells into sensory branch of lingual nerve then ascends to trigeminal ganglion and remains latent for lifetime. ReactivasionReactivation in case of immunosuppression, trauma, or other stresses can result in fulminant haemorrhagic necrotizing encephalitis. HSV has strong affinity for limbic systems with bilateral but asymmetrical involvement.
Histology
Perivascular cuffs of lymphocytes, large inclusions in neurons and glial cells called "owl's eye", neurophagia, necrosis and haemorrhage are characteristics of HSE.
Radiographic features
In the adult immunocompetent patient the pattern is quite characteristic and manifests as bilateral asymmetrical involvement of the limbic system, medial temporal lobes, insular cortices and inferolateral frontal lobes. The basal ganglia are typically spared, helping to distinguish it from a middle cerebral artery infarct. Extralimbic
Extralimbic involvement is more common in children than in adult, seen most commonly in the parietal lobe, with sparing of basal ganglia.Eventually. Eventually, it results in marked cystic encephalomalacia and volume loss in affected areas.
In immunocompromised patients, involvement can be more diffuse, and more likely to involve the brainstem 5.
CT
Early diagnosis is difficult and a 'normal' scan should not dissuade from the diagnosis. If findings are present, they typically consist of subtle low density within the anterior and medial parts of the temporal lobed and the island of Reil (insular cortex) 2. If scanned later then the changes may become more obvious and even progress to haemorrhage.
Contrast enhancement is uncommon during the first week of the disease. Thereafter patchy low level enhancement may be seen 5.
MRI
Affected areas however have a similar appearance, in terms of signal characteristics:
-
T1
- may show general oedema in affected region
- if complicated by subacute haemorrhage there may be areas of hyperintense signal
-
T1 C+ (Gd)
- enhancement is usually absent early on
- later enhancement is variable in pattern 5
- gyral enhancement
- leptomeningeal enhancement
- ring enhancement
- diffuse enhancement
-
T2
- hyperintensity of affected white matter and cortex
- more established haemorrhagic components may the hypointense
-
DWI/ADC
- more sensitive than T2 weighted images
- restricted diffusion is common due to cytotoxic oedema
- beware of T2 shine through due to vasogenic odema
-
GE/SWI
-- may demonstrate blooming if haemorrhagic (rare in neonates, common in older patients)
Treatment and prognosis
Mortality ranges dramatically depending on how early treatment is instituted. Even in patients who are young and otherwise well, and only lethargic still have a mortality of 25%. Older patients or those comatose at the time treatment is started invariably have a much poorer outcome 3. Overall mortality is over 70% with only 2.5% of affected patients every fully recovering 5.
Treatment is with intravenous antivirals (e.g. acyclovir).
Differential diagnosis
General imaging diffeential considerations include
- limbic encephalitis
- gliomatosis cerebri
- status epilepticus
- middle cerebral artery (MCA) infarction: typically involves the basal ganglia
- trauma
- viral encephalitides: many can have very similar appearances and are difficult to separate clinically. Diagnosis usually requires PCR. These include 4:
-</ol><p>This article concerns itself with the latter. For a discussion of the former, please refer to the article <a href="/articles/neonatal-herpes-simplex-encephalitis">neonatal herpes simplex encephalitis</a>. </p><h4>Epidemiology</h4><p>Childhood and adult herpes encephalitis is usually due to HSV-1 (90%) with the rest due to HSV-2 <sup>5</sup>. There is no particular age, sex or seasonal predilection. </p><h4>Clinical presentation</h4><p>Presentation is unfortunately relatively non-specific consisting of fever, headaches, focal neurological deficits, seizures, and altered or decreased level of conciousness.</p><p>Diagnosis is established with PCR of CSF, although the combination of clinical scenario, CSF demonstrating pleocytosis and elevated protein, and appropriate imaging is usually highly suggestive and permits commencement of treatment. </p><h4>Pathology</h4><p>HSV is an obligatory intracelluar virus which enters via infecting nasopharyngeal cells into sensory branch of lingual nerve then ascends to trigeminal ganglion and remains latent for lifetime. Reactivasion in case of immunosuppression, trauma, or other stresses can result in fulminant haemorrhagic necrotizing encephalitis. HSV has strong affinity for limbic systems with bilateral but asymmetrical involvement. </p><p>Perivascular cuffs of lymphocytes, large inclusions in neurons and glial cells called "owl's eye", neurophagia, necrosis and haemorrhage are characteristics of HSE.</p><h4>Radiographic features</h4><p>In the adult immunocompetent patient the pattern is quite characteristic and manifests as bilateral asymmetrical involvement of the limbic system, medial temporal lobes, insular cortices and inferolateral frontal lobes. The basal ganglia are typically spared, helping to distinguish it from a <a href="/articles/middle-cerebral-artery-infarction">middle cerebral artery infarct</a>. Extralimbic involvement is more common in children than in adult, seen most commonly in the parietal lobe, with sparing of basal ganglia.Eventually, it results in marked cystic encephalomalacia and volume loss in affected areas.</p><p>In immunocompromised patients, involvement can be more diffuse, and more likely to involve the <a href="/articles/brainstem">brainstem</a> <sup>5</sup>. </p><h5>CT</h5><p>Early diagnosis is difficult and a 'normal' scan should not dissuade from the diagnosis. If findings are present, they typically consist of subtle low density within the anterior and medial parts of the temporal lobed and the <a href="/articles/island-of-reil">island of Reil</a> (insular cortex) <sup>2</sup>. If scanned later then the changes may become more obvious and even progress to haemorrhage. </p><p>Contrast enhancement is uncommon during the first week of the disease. Thereafter patchy low level enhancement may be seen <sup>5</sup>. </p><h5>MRI</h5><p>Affected areas however have a similar appearance, in terms of signal characteristics:</p><ul>- +</ol><p>This article concerns itself with the latter. For a discussion of the former, please refer to the article <a href="/articles/neonatal-herpes-simplex-encephalitis">neonatal herpes simplex encephalitis</a>. </p><h4>Epidemiology</h4><p>Childhood and adult herpes encephalitis is usually due to HSV-1 (90%) with the rest due to HSV-2 <sup>5</sup>. There is no particular age, sex or seasonal predilection. </p><h4>Clinical presentation</h4><p>Presentation is unfortunately relatively non-specific consisting of fever, headaches, focal neurological deficits, seizures, and altered or decreased level of conciousness.</p><p>Diagnosis is established with PCR of CSF, although the combination of clinical scenario, CSF demonstrating pleocytosis and elevated protein, and appropriate imaging is usually highly suggestive and permits commencement of treatment. </p><h4>Pathology</h4><p>HSV is an obligatory intracelluar virus which enters via infecting nasopharyngeal cells into sensory branch of lingual nerve then ascends to trigeminal ganglion and remains latent for lifetime. Reactivation in case of immunosuppression, trauma, or other stresses can result in fulminant haemorrhagic necrotizing encephalitis. HSV has strong affinity for limbic systems with bilateral but asymmetrical involvement. </p><h5>Histology</h5><p>Perivascular cuffs of lymphocytes, large inclusions in neurons and glial cells called "owl's eye", neurophagia, necrosis and haemorrhage are characteristics of HSE.</p><h4>Radiographic features</h4><p>In the adult immunocompetent patient the pattern is quite characteristic and manifests as bilateral asymmetrical involvement of the <a title="Limbic system" href="/articles/limbic-system">limbic system</a>, medial <a title="Temporal lobe" href="/articles/temporal-lobe">temporal lobes</a>, insular cortices and inferolateral frontal lobes. The basal ganglia are typically spared, helping to distinguish it from a <a href="/articles/middle-cerebral-artery-infarction">middle cerebral artery infarct</a>. </p><p>Extralimbic involvement is more common in children than in adult, seen most commonly in the parietal lobe, with sparing of basal ganglia. Eventually, it results in marked cystic <a title="Encephalomalacia" href="/articles/encephalomalacia">encephalomalacia</a> and volume loss in affected areas.</p><p>In immunocompromised patients, involvement can be more diffuse, and more likely to involve the <a href="/articles/brainstem">brainstem</a> <sup>5</sup>. </p><h5>CT</h5><p>Early diagnosis is difficult and a 'normal' scan should not dissuade from the diagnosis. If findings are present, they typically consist of subtle low density within the anterior and medial parts of the temporal lobed and the <a href="/articles/island-of-reil">island of Reil</a> (insular cortex) <sup>2</sup>. If scanned later then the changes may become more obvious and even progress to haemorrhage. </p><p>Contrast enhancement is uncommon during the first week of the disease. Thereafter patchy low level enhancement may be seen <sup>5</sup>. </p><h5>MRI</h5><p>Affected areas however have a similar appearance, in terms of signal characteristics:</p><ul>
-<strong>GE/SWI</strong> - may demonstrate blooming if haemorrhagic (rare in neonates, common in older patients)</li>-</ul><h4>Treatment and prognosis</h4><p>Mortality ranges dramatically depending on how early treatment is instituted. Even in patients who are young and otherwise well, and only lethargic still have a mortality of 25%. Older patients or those comatose at the time treatment is started invariably have a much poorer outcome <sup>3</sup>. Overall mortality is over 70% with only 2.5% of affected patients every fully recovering <sup>5</sup>. </p><p>Treatment is with intravenous antivirals (e.g. acyclovir)</p><h4>Differential diagnosis</h4><p>General imaging diffeential considerations include</p><ul>- +<strong>GE/SWI</strong><ul><li>
- +<strong></strong>may demonstrate blooming if haemorrhagic (rare in neonates, common in older patients)</li></ul>
- +</li>
- +</ul><h4>Treatment and prognosis</h4><p>Mortality ranges dramatically depending on how early treatment is instituted. Even in patients who are young and otherwise well, and only lethargic still have a mortality of 25%. Older patients or those comatose at the time treatment is started invariably have a much poorer outcome <sup>3</sup>. Overall mortality is over 70% with only 2.5% of affected patients every fully recovering <sup>5</sup>. </p><p>Treatment is with intravenous antivirals (e.g. acyclovir).</p><h4>Differential diagnosis</h4><p>General imaging diffeential considerations include</p><ul>
Tags changed:
- infectious disease
Image ( destroy )
Image ( update )
Image ( destroy )
Image 2 MRI (T2) ( update )
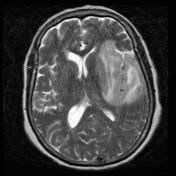
Image 3 MRI (FLAIR) ( update )

Image 4 MRI (FLAIR) ( update )
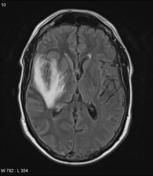
Image 5 MRI (DWI) ( update )

Image 6 MRI (T2) ( update )

Image 7 MRI (FLAIR) ( update )

Image 8 MRI (T2) ( update )

Image 10 MRI (FLAIR) ( update )

Image 11 MRI (T1) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.