Intracranial lipomas are not tumors as such, but rather a result of abnormal differentiation of embryologic meninx primitiva. They are frequently associated with abnormal development of adjacent structures.
On this page:
Terminology
The term intracranial lipoma is used somewhat loosely. The broadest usage would include all causes of focal adipose tissue within the intracranial cavity (e.g. fatty falx cerebri). A narrower, and probably more useful, definition is to limit the use of the term to adipose tissue within the intradural space, specifically those located within the CSF-containing spaces (subarachnoid space and around the ventricles). The remainder of this article restricts itself to this narrower definition.
Epidemiology
Intracranial lipomas are congenital lesions and as such are found at any age when the brain is imaged for other reasons.
Clinical presentation
They are usually asymptomatic, and either found incidentally or as a result of investigation of related malformations and their presentation (e.g. epilepsy, hydrocephalus) 5,6. If symptomatic, patients may present with a range of potential symptoms, including headaches, epilepsy, intellectual disability, and cranial nerve deficits 6.
Pathology
A number of theories have been put forward to explain the development of intracranial lipomas. The favored theory is persistence and maldifferentiation of the meninx primitiva (subarachnoid space precursor), which accounts for the subarachnoid location, associated parenchymal anomalies, and traversing structures of intracranial lipomas 7,8.
Location
Intracranial lipomas are widely distributed in the intracranial compartment. Although they can be found essentially anywhere, certain regions are characteristic:
-
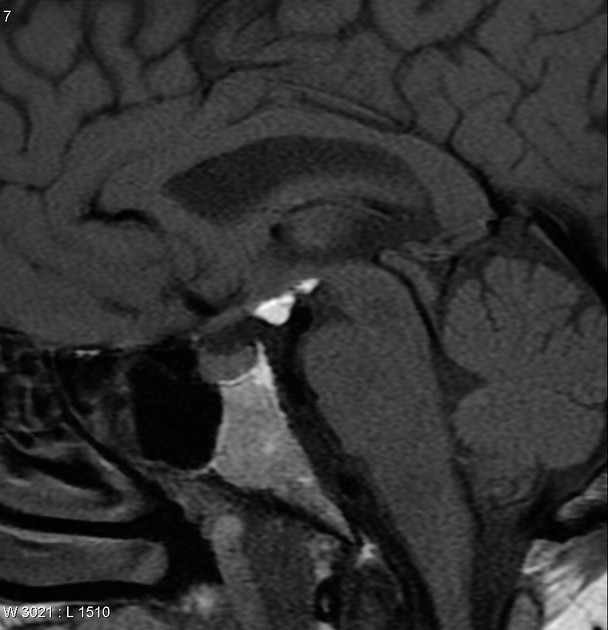
pericallosal lipoma (50%)
associated with agenesis of the corpus callosum in ~50% of cases
divided morphologically into tubonodular and curvilinear types
-
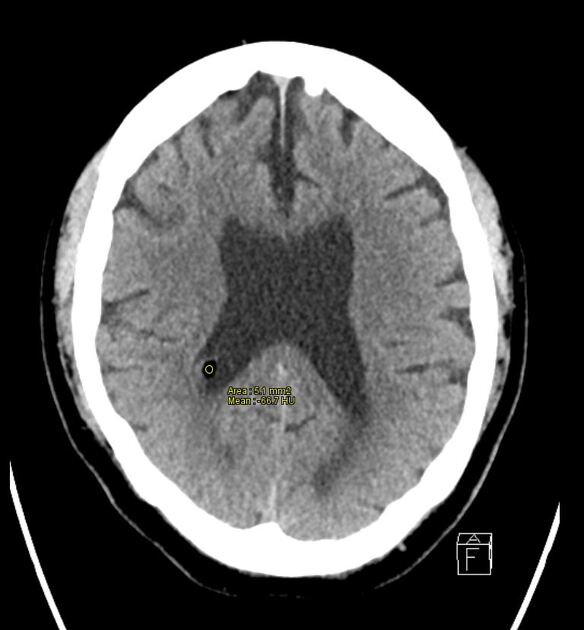
quadrigeminal cistern lipoma (25%)
associated with underdevelopment of the inferior colliculus
-
cerebellopontine angle lipoma (10%)
the facial nerve and vestibulocochlear nerve often courses through the lipoma
Sylvian fissure (5%)
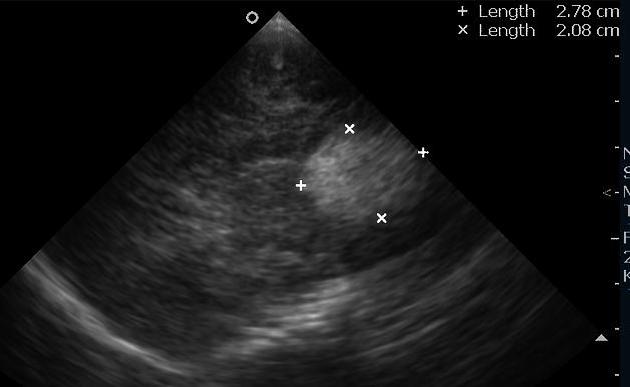
choroid plexus lipoma (rare) 9
Radiographic features
The characteristic finding on both CT and MRI is a mass which has appearances consistent with fat.
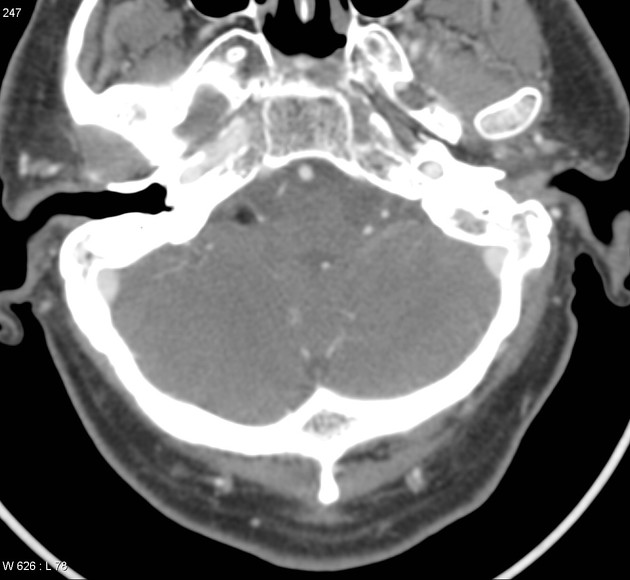
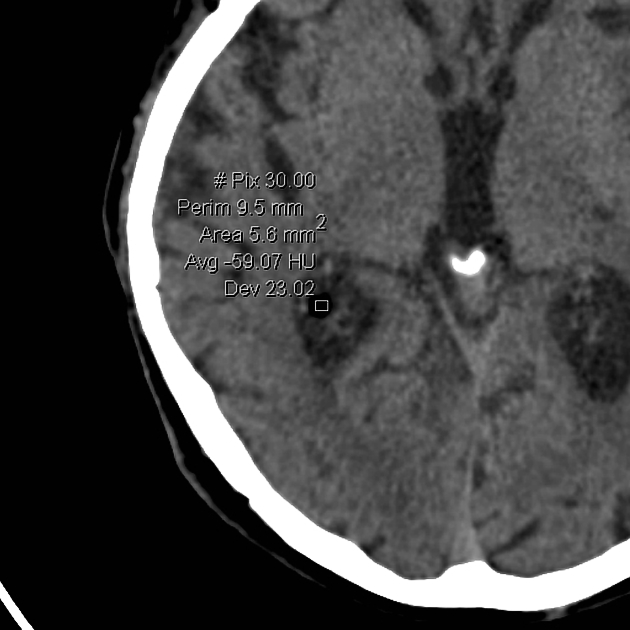
CT
On CT, they typically appear as a non-enhancing mass with uniform fat density (CT attenuation values of ~-100). It has a lobulated 'soft' appearance, conforming to adjacent anatomy. Some peripheral calcification may be present.
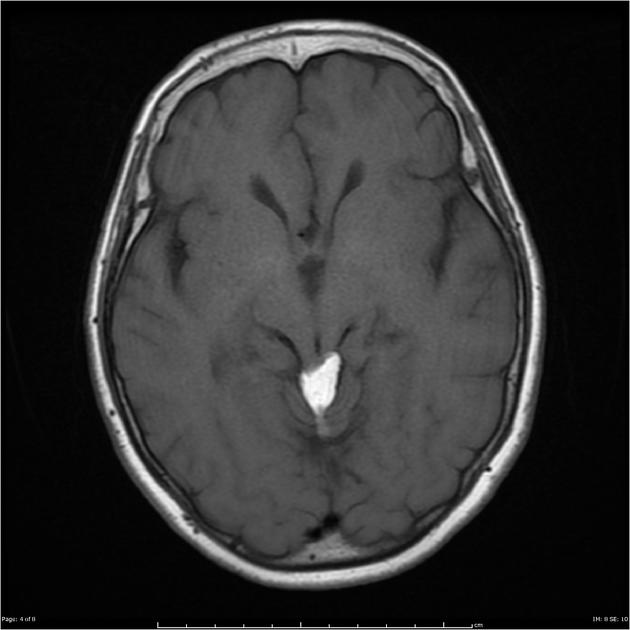
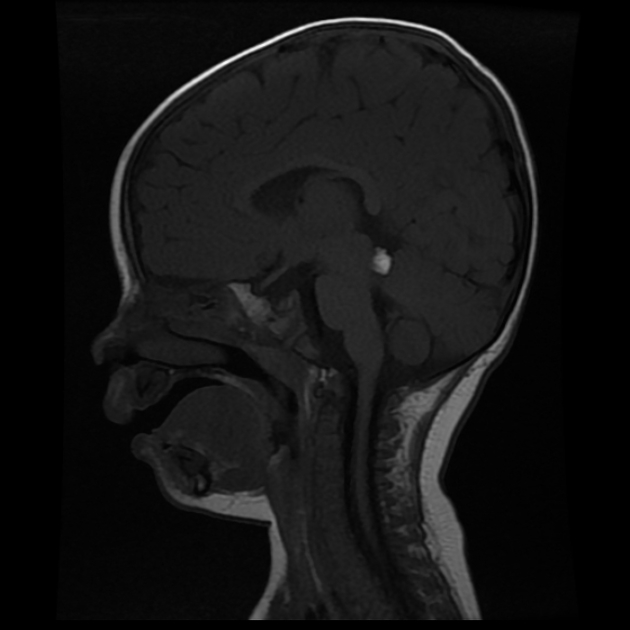
MRI
MRI with and without fat saturation are able to make the diagnosis easily. In the absence of fat-saturated images, then chemical shift artifact may be useful. Signal characteristics are, not surprisingly, that of fat:
T1: high signal intensity
T2: high signal intensity
T1 C+ (Gd): no enhancement
fat saturated sequences: low signal
SWI: can produce blooming due to susceptibility artifact 10
Often the lipomas are traversed by cranial nerves and adjacent vessels, best seen on high-resolution sequences.
Treatment and prognosis
Intracranial lipomas are in most cases asymptomatic, and even when associated with symptomatic malformations (e.g. callosal dysgenesis) they usually require no treatment per se. In fact, attempts at resection have had relatively high morbidity with little benefit due to their vascular characteristics and adhesion to surrounding neural tissue 5,6,11. Treatment of seizures or hydrocephalus is clinically indicated if these are present 5,6.
Differential diagnosis
The differential is essentially that of masses which contain fat, and therefore includes:
intracranial dermoid: if ruptured will often have multiple droplets scattered through the subarachnoid space; usually midline
lipomatous transformation of neoplasm: PNET, ependymoma, glioma
On MRI, if no fat saturated sequences are available then a number of other possibilities should be entertained, which also have high T1 signal.
thrombosed berry aneurysm: often will have a calcified rim and hemosiderin staining on gradient echo or SWI sequences
white epidermoid: rare, and will restrict on DWI







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.