Kawasaki disease is a small to medium vessel vasculitis predominantly affecting young children. It can affect any organ but there is a predilection for the coronary vessels.
On this page:
Epidemiology
Japan has the highest incidence in the world, with an annual incidence of 3 per 1000 children under the age of four years 10. Worldwide, it is the most common vasculitis in children 9. It is slightly more common in males with a M:F ratio of 1.4:1 10.
It is more common in siblings; ~3% of siblings will be diagnosed with Kawasaki. This equates to a ten-fold increased risk in a sibling. It is also more likely in children of affected parents, although no genetic link has been identified 10.
In the United States, it is most commonly seen in children of Asian ethnicity, in particular, Japanese, but less commonly in the Black population and least commonly in the White population.
Since April 2020, rare cases of a Kawasaki-like disorder have been reported in critically-ill children who are COVID-19 positive. A true causative association between SARS-CoV-2, the cause of COVID-19, and Kawasaki disease has not been established as yet 14,15.
Diagnosis
Diagnostic criteria
Classic Kawasaki disease is diagnosed in the presence of fever for at least 5 days and at least 4 of the following:
erythema and cracking of lips, strawberry tongue, or erythema of oral and pharyngeal mucosa
bilateral bulbar conjunctival injection without exudate
rash: maculopapular, diffuse erythroderma, or erythema multiforme–like
erythema and edema of the hands and feet in the acute phase
cervical lymphadenopathy (≥1.5 cm in diameter), usually unilateral
Clinical presentation
Persistent fever is the commonest way with which most children present. The specific signs and symptoms vary with the stage of the disease:
Acute stage
fever that is refractory to antibiotics
general malaise and irritability
anterior uveitis (70%)
perianal erythema (70%)
lymphadenitis (75%)
strawberry tongue
Subacute stage
desquamation of the digits
highest risk of death
Convalescent stage
clinical symptoms and signs recede
Chronic stage
persistence of any cardiac complications into adulthood
Pathology
An autoimmune etiology has been postulated. It is generally self-limiting but acute fatalities are thought to occur in ~1% of cases. The most concerning morbidity is due to coronary involvement where it can manifest as myocarditis with coronary arterial aneurysm formation 1,2,4.
Radiographic features
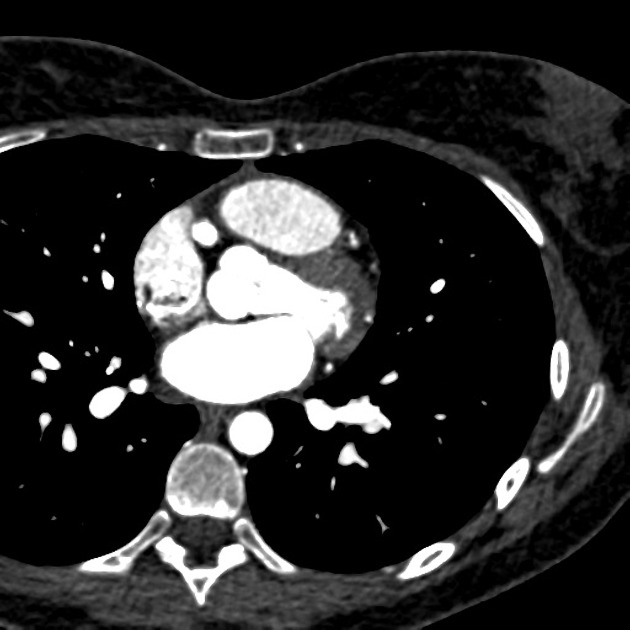
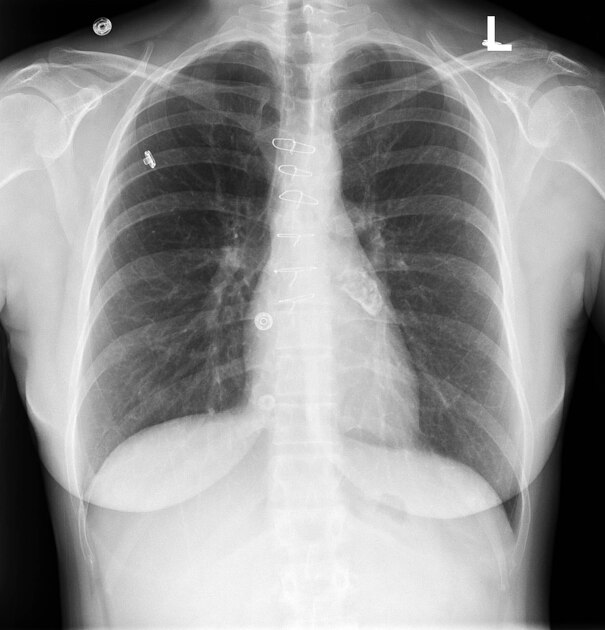
Plain radiograph
Chest radiographs can be normal. Abnormal findings are non-specific and include a reticulogranular pattern, peribronchial cuffing, pleural effusion, atelectasis and/or air trapping 1.
Rarely, a few years after resolution of the initial episode, the patient may present with calcified coronary artery aneurysms visible on the chest x-ray 8. Although rare, this is an Aunt Minnie presentation of Kawasaki disease sequelae in older patients.
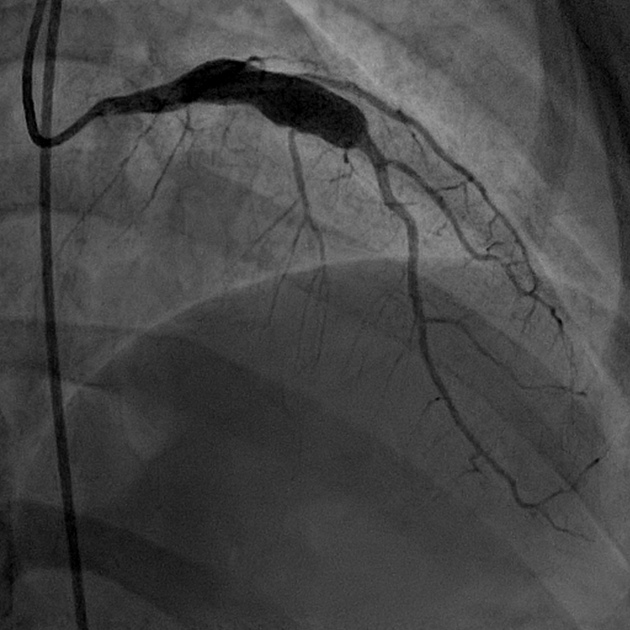
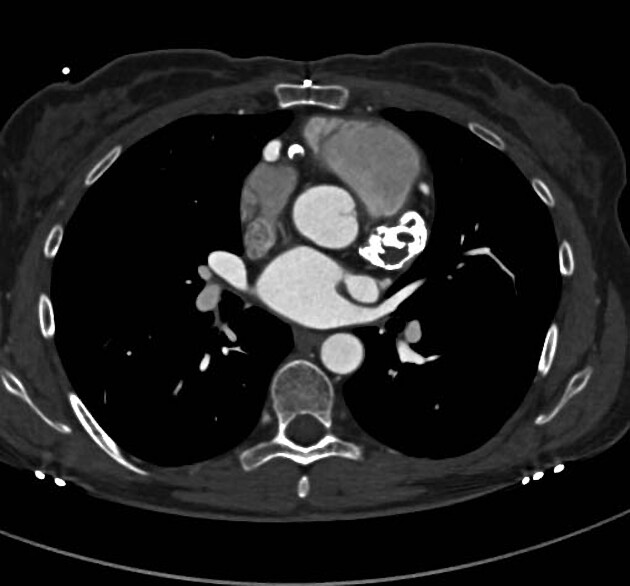
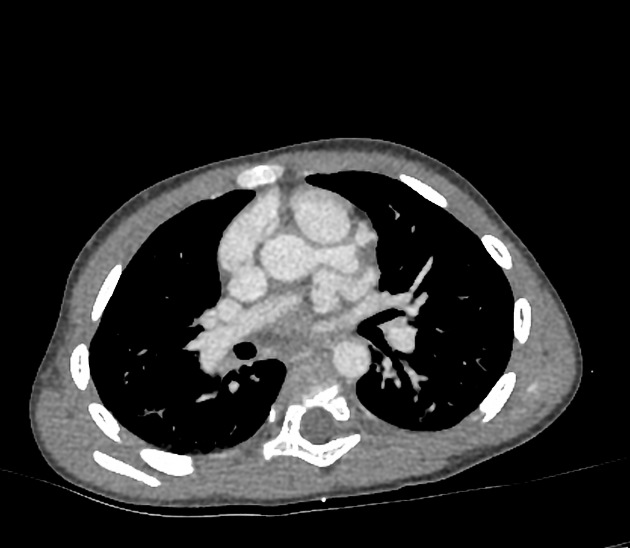
Angiography (coronary/CT/MRI)
May show small coronary arterial ectasias, aneurysms or stenoses. Angiography is the most sensitive and specific for vascular assessment 4.
Coronary artery aneurysms can be classified as 11:
small: <5 mm
medium: 5-8 mm
large: >8 mm
Coronary stenosis is more common in the left coronary artery while intracoronary thrombus is more frequently observed in the right coronary artery 11.
MRI is also useful in assessing myocardial perfusion, wall thinning, and aneurysms.
Ultrasound
Echocardiography
Transthoracic echocardiography is especially useful in the approach to patients who fall short of full clinical criteria (incomplete Kawasaki disease), as the presence of the following is diagnostic 12:
-
dilation which exceeds the mean coronary artery diameters by 2.5 standard deviations is classified as aneurysmal
-
manifestation of endocardial inflammation
Treatment and prognosis
Initial treatment consists of intravenous immunoglobulin and aspirin 17. In refractory cases, corticosteroids, infliximab, and other immunosuppression may be employed 17.
History and etymology
It is named after the Japanese pediatrician Tomisaku Kawasaki (1925-2020) 9,16 who saw his first case in 1961 and initially described it in a case series of 50 children in 1967 7,9.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.