CNS infection with Listeria monocytogenes, classically presenting as listeria rhombencephalitis, results from infection with Listeria monocytogenes, a motile facultative anaerobic bacterium. It is cited as the most common etiology for rhombencephalitis, typically seen in the elderly, and resulting in significant morbidity and mortality but the involvement of the rest of the central nervous system, particularly in immunocompromised individuals.
On this page:
Epidemiology
The majority of listerial rhombencephalitis cases occur in previously healthy adults who develop infection with Listeria monocytogenes 2,3. Rhomboencaphalitis develops in approximately 17% of patients with listeriosis 7.
In contrast, listerial cerebritis or meningoencephalitis is rare and encountered mostly in the setting of immune compromise (organ transplant, malignancy, HIV/AIDS, etc..) 4,5,8.
Pregnancy also increases susceptibility to infection, which may, despite being subclinical in the mother, nonetheless result in chorioamnionitis and subsequent stillbirth or early-onset neonatal listeriosis 8.
Neonatal listeriosis also occurs and can be "early-onset" (transplacental infection resulting in premature delivery of a septic neonate) or "late-onset" (infection occurs at the time of delivery from a colonized birth canal and presents one to two weeks later) 8.
Clinical presentation
Affected patients tend to have two phases that reflect the pathogenesis of the disease (see below).
prodrome
neurological signs and symptoms
The prodrome lasts one to two weeks and results from systemic listeria infection. Patients experience fatigue, fevers, nausea and vomiting 7. Due to the non-specific nature of these symptoms, patients are often misdiagnosed 1-3.
Patients with rhombencephalitis later develop a spectrum of symptoms due to brainstem involvement, such as multiple cranial nerve palsies (occur in ~75% of all cases) or cerebellar deficits, long-tract motor and/or sensory deficits, ataxia, nystagmus, vertigo, facial numbness, dysphagia, persistent hiccuping, and respiratory failure (~41%) 3.
CSF
increased leukocyte count (usually due polymorphonuclear cells) 1
increased protein 1
normal glucose levels 1
It is difficult to isolate the agent: the bacillus can be cultured from blood in 61% and from CSF in 33-41% 3,7.
Pathology
Listeria monocytogenes is an anaerobic and gram-positive bacillus found commonly in animal and human feces and in the soil and thus also in food and water 5.
In most cases, the bacteria is injested orally and reaches the enteric nerves through a breach in the mucosa or via dental disease and becomes an intracellular pathogen 5,6. From there, the bacteria can migrate along the nerves via axonal migration back towards the brainstem nuclei 5-7. This can occur via innervation of the oral cavity (trigeminal nerve, facial nerve, glossopharyngeal nerve and vagus nerve) or bowel (vagus nerve). This axonal migration takes time and may account for the lengthy delay between exposure and manifestation of brainstem symptoms 5,7.
Radiographic features
Beam-hardening artifacts limit the visualization of the brainstem on CT images (initial CT of the brain often gives normal results) and MRI is the imaging modality of choice for the assessment of patients with suspected pathology in that anatomic location. The protocol should include contrast.
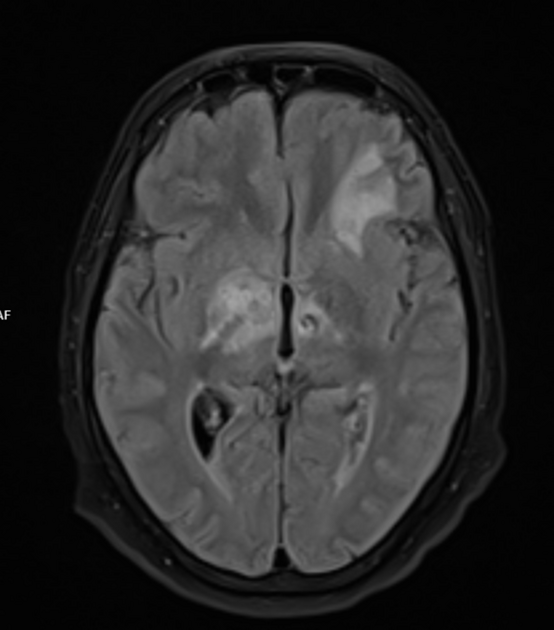
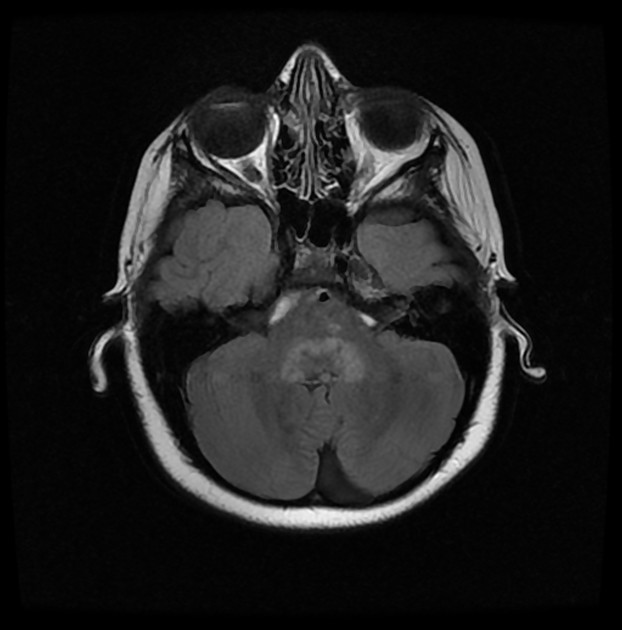
Subcortical abscesses in the thalamus, pons and medulla are common in rhombencephalitis caused by this bacteria, due to the aforementioned retrograde infection along cranial nerves 2,3,5,6.
MRI
T1: hypo- to isointense lesion
T2/FLAIR: hyperintense
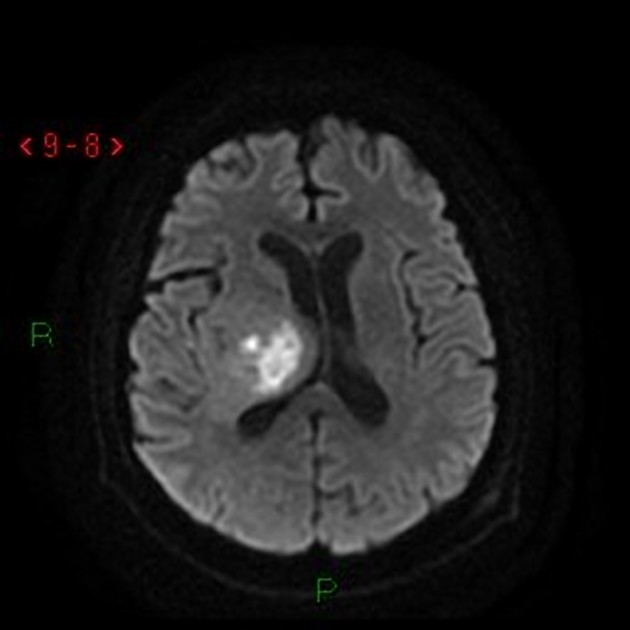
DWI: hyperintense/hypointense on ADC map
-
T1 C+:
linear cranial nerve enhancement, both the cisternal segment and the course through the brainstem to the nucleus 7
ring enhancement (abscess)
heterogeneous if extensive inflammation
Treatment and prognosis
Listeria rhombencephalitis is reported to have a high mortality (30-50%) and frequent serious sequelae for survivors (~60%) 3,7.
Survival is strongly related to the timely use of appropriate antibiotics: usually ampicillin or penicillin combined with gentamicin for a period of at least six weeks 2.
Pregnancy-associated listeriosis, particularly early-onset listeriosis, has a poor prognosis 8.
Differential diagnosis
-
other causes of infective rhomboencephalitis/encephalitis
bacterial, fungal, mycobacterial, parasitic, viral
-
demyelination
tumors
Behçet disease




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.