Splenic trauma can occur after blunt or penetrating trauma or secondary to medical intervention (i.e. iatrogenic). The spleen is the most frequently injured internal organ after blunt trauma.
On this page:
Epidemiology
In blunt trauma, the spleen can account for up to 49% of abdominal organ injuries 2.
Clinical presentation
Patients may present with left upper quadrant, left chest pain, left shoulder tip pain (referred from diaphragmatic irritation), and signs of hypotension or shock.
Pathology
The spleen may be injured after blunt or penetrating trauma or may be iatrogenic (e.g. colonoscopy).
Types
laceration
-
hematoma: subcapsular (more common) or intraparenchymal
active hemorrhage
pseudoaneurysm or AV fistulas (in ~15% of splenic trauma 4)
splenic infarct (rare) 7
Grading
Associations
Splenic trauma is associated with injuries to other intra-abdominal organs 1:
left hemidiaphragm
left lobe of the liver
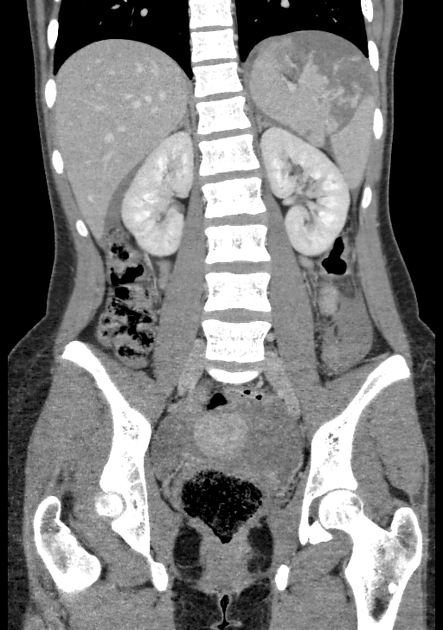
left kidney
left adrenal gland
In penetrating trauma, the spleen is more likely to be injured than bowel 6.
Radiographic features
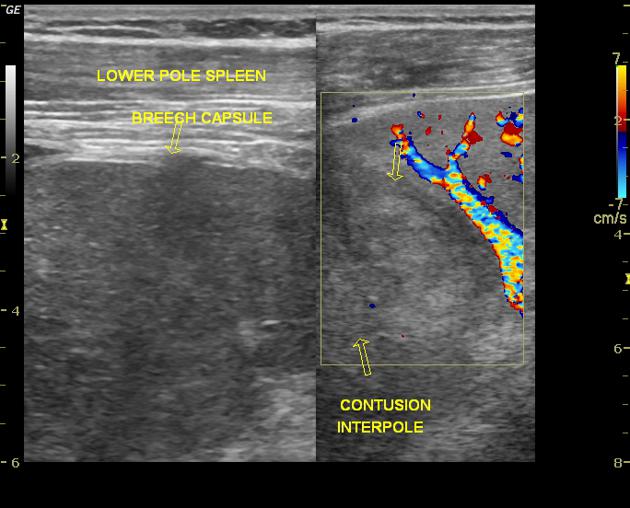
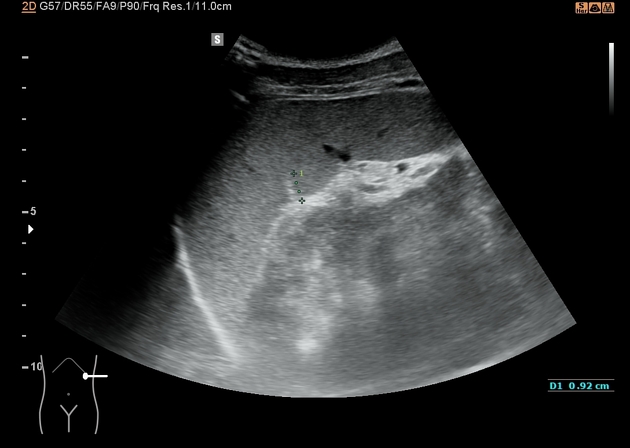
Ultrasound
-
FAST scanning may be performed to determine the presence of free fluid
particularly in the upper abdomen
fresh blood is usually characterized as echoes free
absence of free fluid does not rule out splenic injury 1
disruption to the splenic echotexture indicating laceration or hypoechoic regions representing hematoma may be present 1
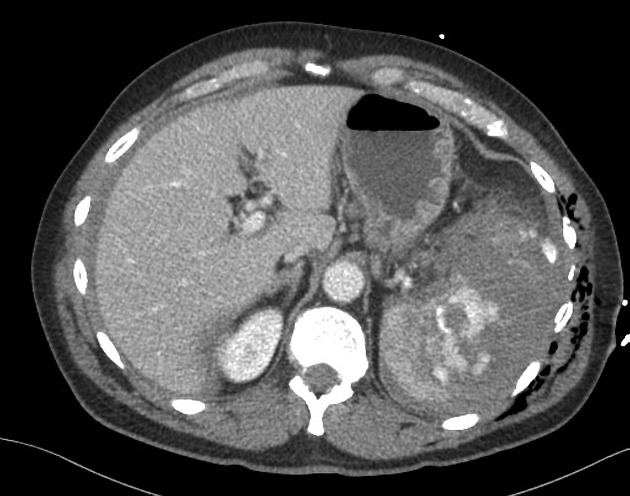
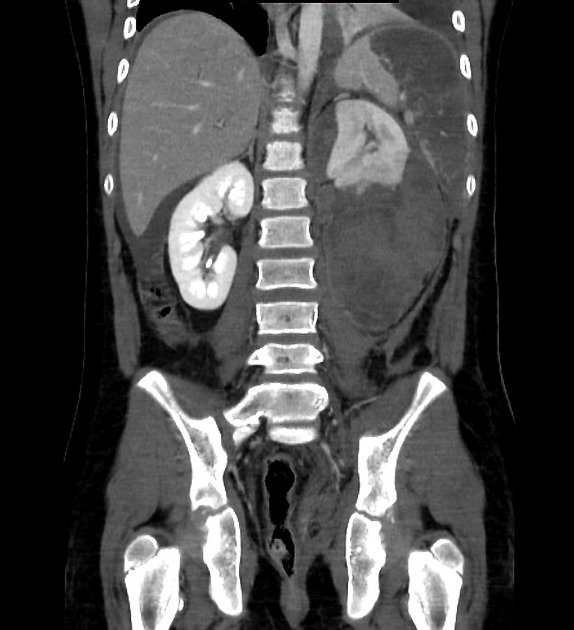
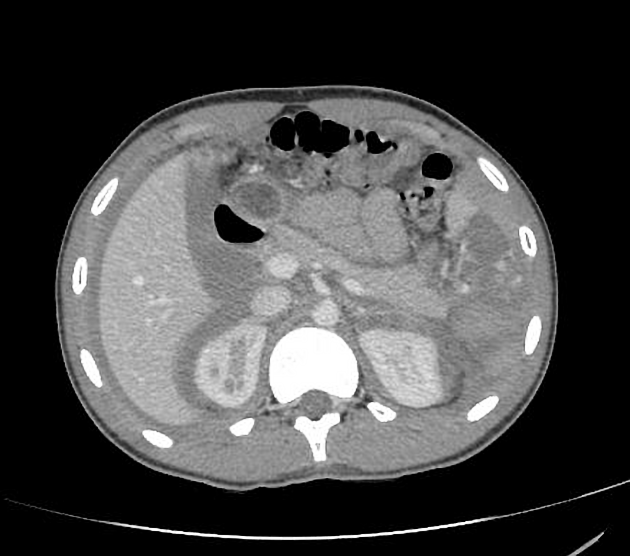
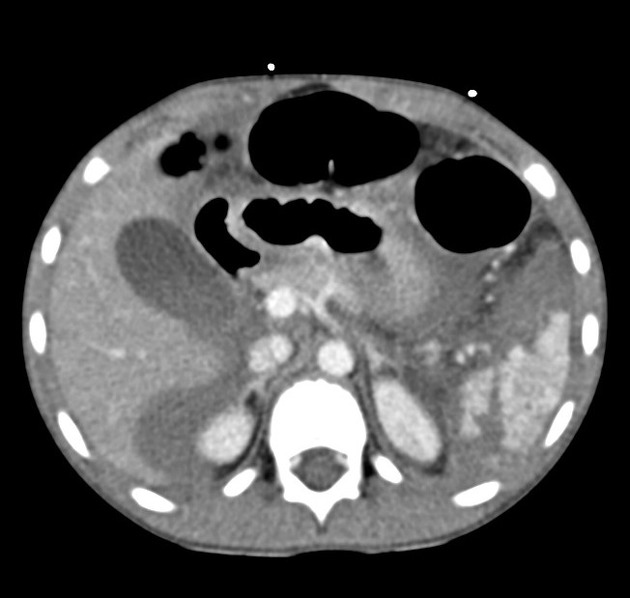
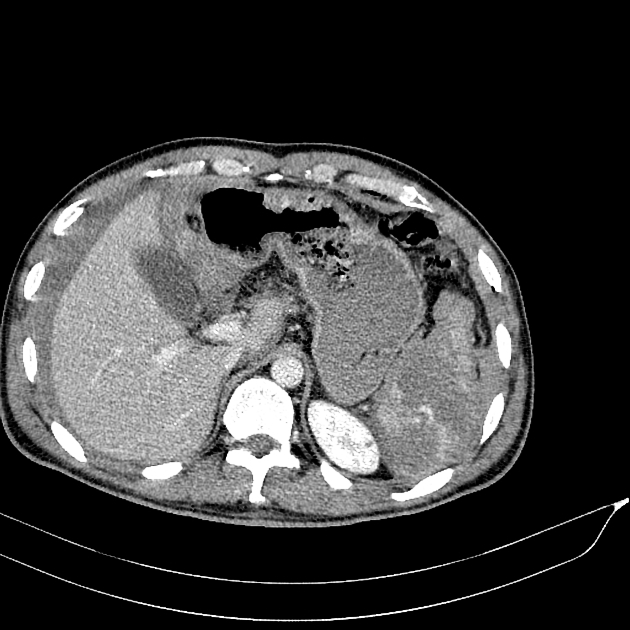
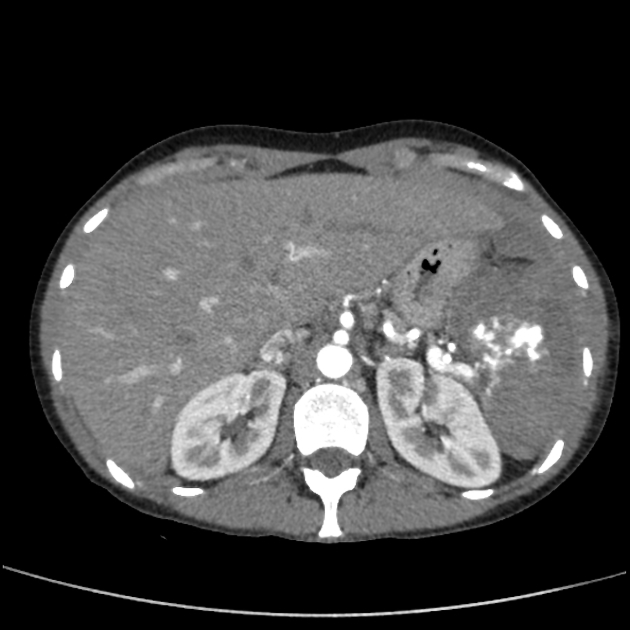
CT
CT is the modality of choice for assessing splenic trauma:
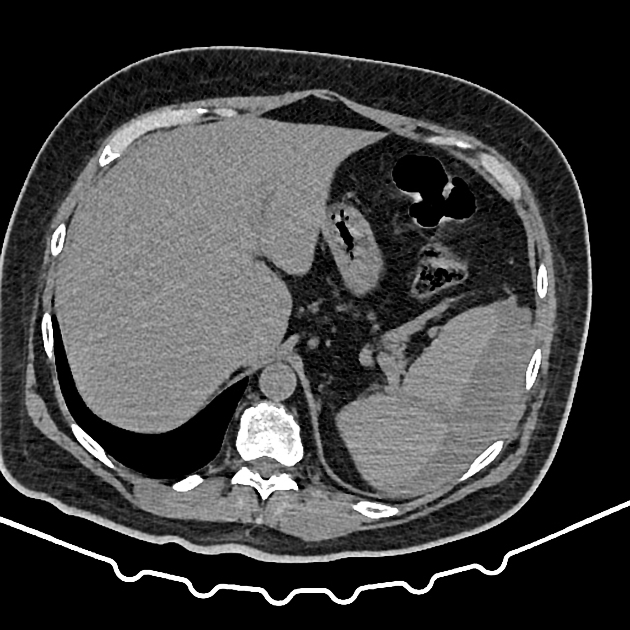
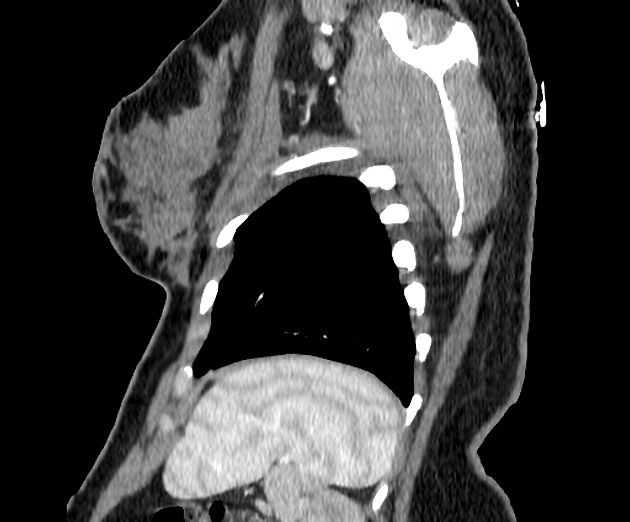
splenic parenchyma should be assessed in portal venous phase as the inhomogeneous splenic enhancement (zebra or psychedelic spleen) seen on the arterial phase can mimic splenic laceration/contusion; arterial phase scanning can be useful in detecting vascular injuries such as pseudoaneurysm and AV fistula 3-5
lacerations appear as linear or branching hypodensities (geographic pattern) 3
subcapsular hematomas can be seen as low-density fluid adjacent to the spleen that distorts the splenic architecture 2
active hemorrhage appears as a high-density (80-95 HU) material due to the extravasation of contrast media that increases in size on delayed imaging 2,3
pseudoaneurysms and AV fistulas have a similar appearance to active hemorrhage on initial scanning but do not increase in size on delayed phases 3 and follow the blood pool
-
splenic clefts may be mistaken for a laceration 9
these are due to persistent lobulation of the spleen after development
in contrast to a laceration, a cleft is usually smooth with a rounded edge and is not associated with an adjacent subcapsular hematoma or perisplenic fluid
some larger clefts may contain fat
DSA
active contrast extravasation contained in the splenic parenchyma
active contrast extravasation entering the peritoneal cavity
focal regions of non enhancement
pseudoaneurysm
arteriovenous fistula
multiple small punctate regions of intraparenchymal contrast extravasation (Seurat spleen)
Treatment and prognosis
Most splenic injuries in haemodynamically-stable patients are treated non-surgically. Splenic artery embolization plays a major role in treating high-grade splenic injuries (both in haemodynamically-stable and -unstable patients; practice varies from institution-to-institution).
Splenectomy is considered by the surgical team if there is major active bleeding seen on CT.
Complications
Complications of splenic trauma include 2:
delayed splenic rupture (~5% in non-surgically treated patients)
splenic pseudocyst (<1%)
splenic abscess formation
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.