Supratentorial ependymomas are an uncommon type of ependymoma, found within the cerebral hemispheres, either remote to or abutting the ventricles.
They have distinct molecular features compared to both posterior fossa ependymomas and spinal ependymomas.
On this page:
Epidemiology
Overall, supratentorial ependymomas affect primarily children and adolescents, but also adults to a lesser degree 10.
The epidemiology varies according to molecular subtype 7,9,10:
-
supratentorial ependymoma, ZFTA fusion-positive
the majority of supratentorial ependymomas, especially in children
M:F = 2:1
age: older children
-
supratentorial ependymoma, YAP1 fusion-positive
uncommon (<10% of all supratentorial ependymomas)
M:F = 1:3
age: <3 years of age
Clinical presentation
Supratentorial ependymomas usually present with headaches, seizures and focal neurological deficits compared to their infratentorial counterparts that mainly present with features of raised intracranial pressure.
Pathology
Although histologically similar, supratentorial ependymomas have a distinct molecular profile to the more common posterior fossa ependymomas. In the 5th edition (2021) of the WHO classification of CNS tumors, supratentorial ependymomas are divided into 9,10:
supratentorial ependymoma, ZFTA (RELA) fusion-positive
supratentorial ependymoma, YAP1-MAMLD1 fusion
In the minority of cases when these two common molecular alterations are absent (17-30%), or testing is inconclusive or unavailable, then the term supratentorial ependymoma NEC or NOS should be used respectively 10.
Radiographic features
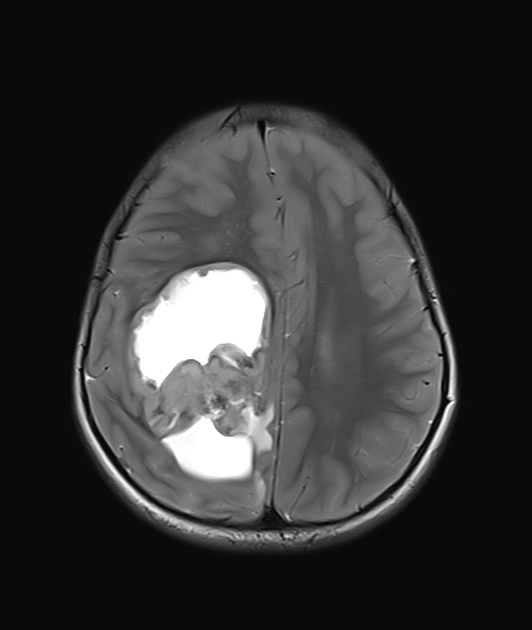
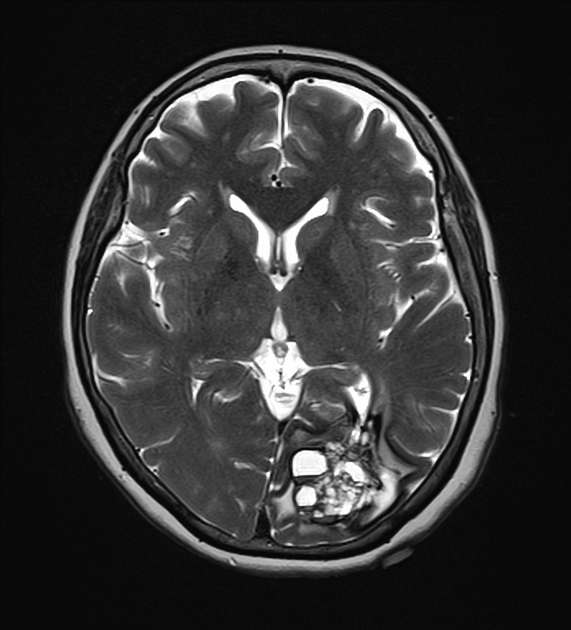
Radiologically these tumors have few characteristic features, appearing as heterogeneous parenchymal masses with calcification, cystic components, solid enhancing components and surrounding edema.
Although they can be located anywhere in the hemispheres, they seem to have a predilection for the frontal and parietal lobes 10.
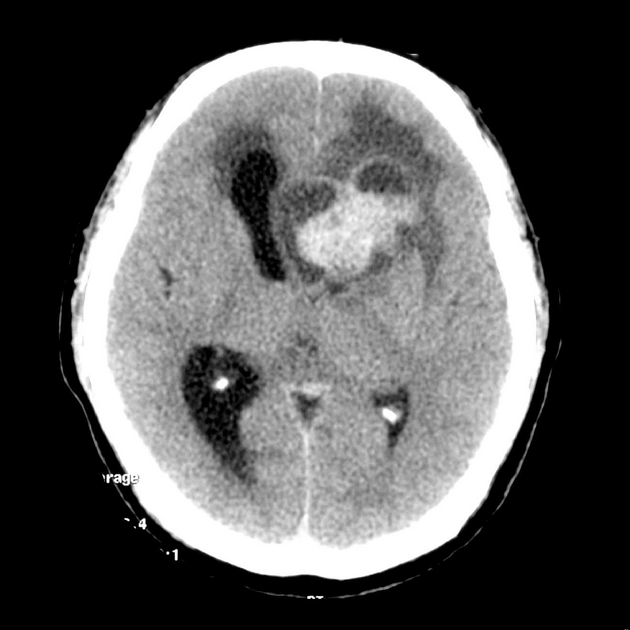
CT
coarse calcification is common (50%)
cystic areas (50%)
solid component iso to slightly hyperdense
heterogeneous enhancement
a small proportion can have hemorrhage
non-contrast CT appearances of an intraparenchymal ependymoma is said to resemble a periwinkle flower, thus periwinkle sign 8.
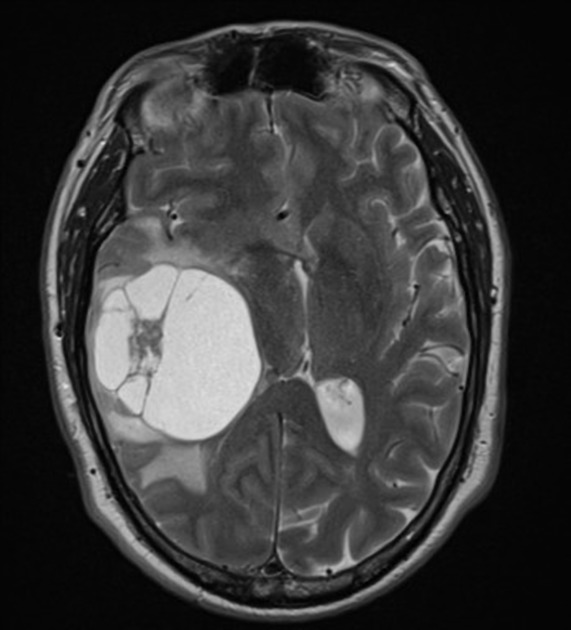
MRI
-
T1
solid portions of ependymoma typically are isointense to hypointense relative to white matter 7
-
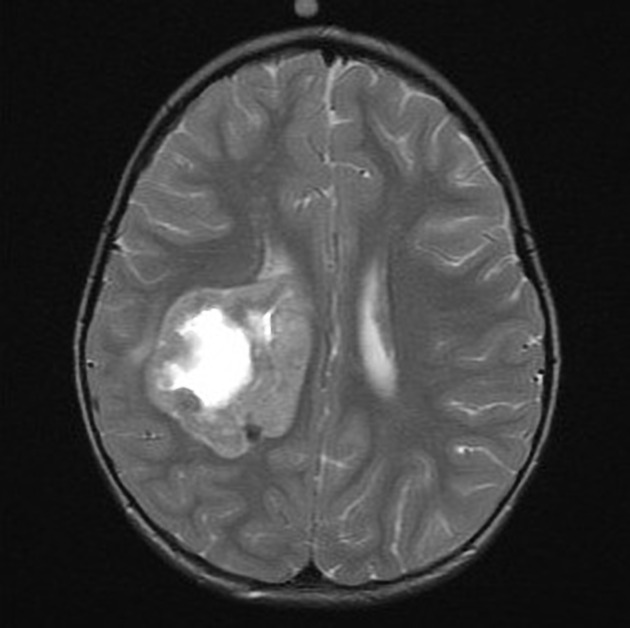
T2
hyperintense to white matter
more reliable in differentiating tumor margins than non-contrast T1-weighted images (but less reliable than contrast-enhanced T1)
-
T2* (e.g. SWI)
foci of blooming from hemorrhage or calcification
-
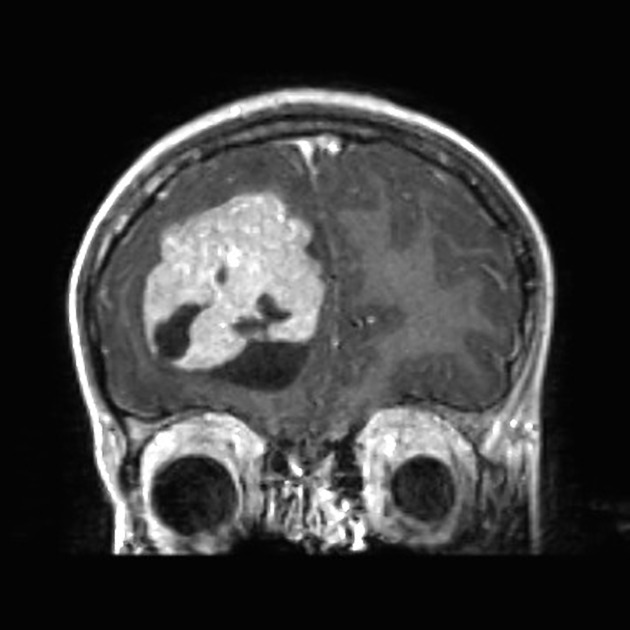
T1 C+ (Gd)
enhancement present but heterogeneous
enhancement with gadolinium is useful in differentiating tumors from adjacent vasogenic edema and normal brain parenchyma
-
DWI/ADC
restricted diffusion may be seen in solid components especially in grade 3 tumors
diffusion should be interpreted with caution in masses with significant hemorrhage or calcification
Mnemonic
The imaging findings can be remembered by the “1234 rule”:
1: a single large tumor common in the first decade
2P: Perilesional edema and Periwinkle sign
3L: Large Lobulated Lobar mass
4C: Central Chunky Calcification and large peripheral Cyst
Treatment and prognosis
Treatment is primarily with maximal (hopefully complete) surgical resection 10. Recurrence is common and CSF spread is encountered fairly frequently, especially in grade 3 tumors 10.
Supratentorial ependymomas generally have a somewhat poorer prognosis than their more common posterior fossa counterparts 10. This is especially the case in children 7.
ZFTA fusion-positive tumors have a poor prognosis, whereas YAP1 fusion-positive tumors appear to have a substantially better prognosis, despite their often large size at diagnosis 10.
Differential diagnosis
Imaging differential considerations depend on whether the tumor is within the parenchyma (usually the case) or less commonly within the ventricle.
For parenchymal tumors consider:
When the mass appears to be intraventricular, consider:





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.