Ultrasound assessment of carotid arterial atherosclerotic disease has become the first choice for carotid artery stenosis screening, permitting the evaluation of both the macroscopic appearance of plaques and flow characteristics in the carotid artery.
This article focuses on internal carotid artery (ICA) stenosis, reporting both criteria: the one published by the Society of Radiologists in Ultrasound 2 and the Sonographic NASCET Index 1.
Please refer to the article on extracranial carotid artery stenosis for a general discussion involving carotid stenosis and other image modalities engaged in it.
Society of Radiologists in Ultrasound (SRU) consensus
This consensus developed recommendations for the diagnosis and stratification of ICA stenosis 2.
[PSV = peak systolic velocity; EDV = end-diastolic velocity; ICA = internal carotid artery; CCA = common carotid artery]
-
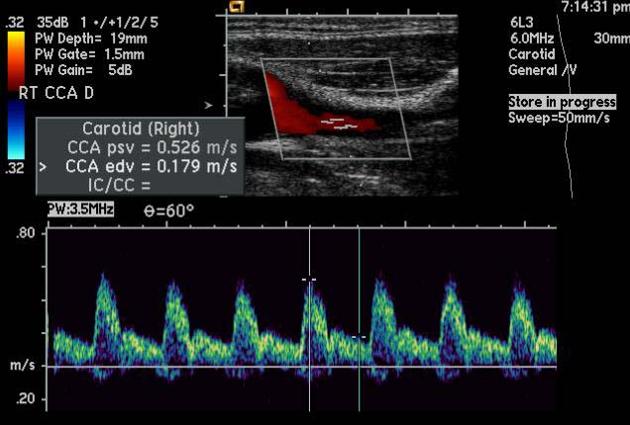
normal
ICA PSV is <125 cm/sec and no plaque or intimal thickening is visible sonographically
additional criteria include ICA/CCA PSV ratio <2.0 and ICA EDV <40 cm/sec
-
<50% ICA stenosis
ICA PSV is <125 cm/sec and plaque or intimal thickening is visible sonographically
additional criteria include ICA/CCA PSV ratio <2.0 and ICA EDV <40 cm/sec
-
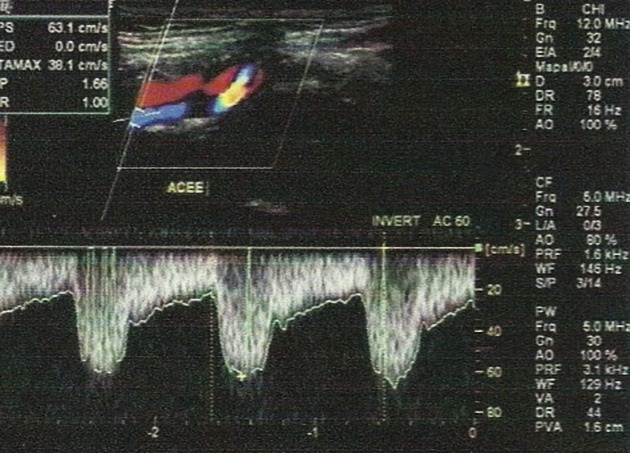
50-69% ICA stenosis
ICA PSV is 125-230 cm/sec and plaque is visible sonographically
additional criteria include an ICA/CCA PSV ratio of 2.0-4.0 and an ICA EDV of 40-100 cm/sec
-
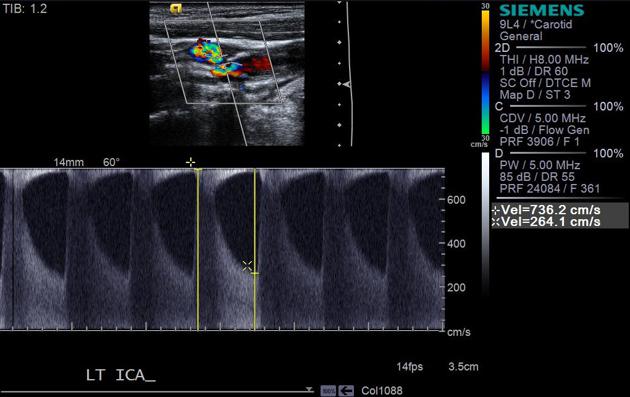
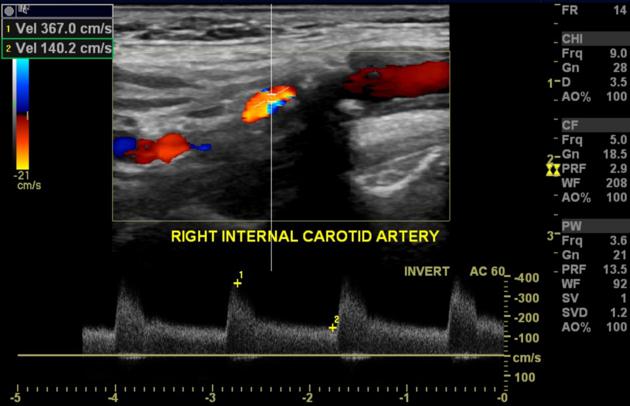
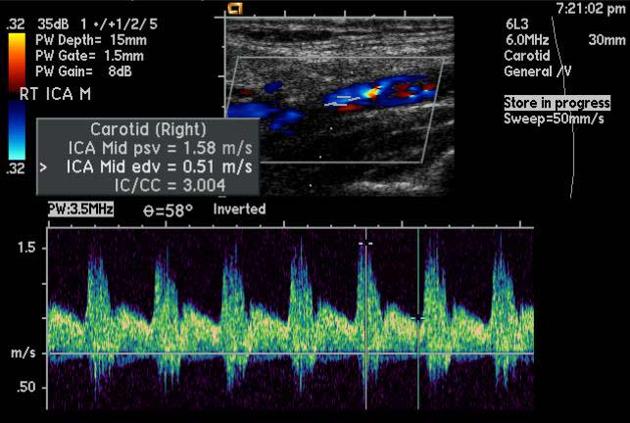
≥70% ICA stenosis but less than near occlusion
ICA PSV is >230 cm/sec and visible plaque and luminal narrowing are seen at grey-scale and color Doppler ultrasound (the higher the Doppler parameters lie above the threshold of 230 cm/sec, the greater the likelihood of severe disease)
additional criteria include ICA/CCA PSV ratio >4 and ICA EDV >100 cm/sec
-
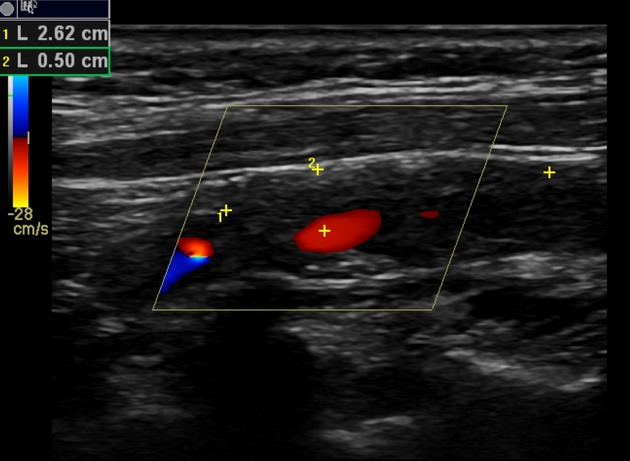
near occlusion of the ICA
variable velocity parameters which may be high, low, or undetectable
diagnosis is established primarily by demonstrating a markedly narrowed lumen with "trickle flow," on color or power Doppler ultrasound
-
total occlusion of the ICA:
no detectable luminal patency with grey-scale ultrasound and no detectable flow with color, spectral, or power Doppler ultrasound
there may be compensatory increased velocity in the contralateral carotid
Sonographic NASCET Index
This study proposed incorporating distal ICA flow velocity information on the conventional carotid Doppler study improving the diagnostic accuracy of PSV 1.
-
<15% stenosis
deceleration spectral broadening with a peak systolic velocity (PSV) <125 cm/s
-
16-49% stenosis
pansystolic spectral broadening with a PSV <125 cm/s
-
50-69% stenosis
pansystolic spectral broadening with a PSV of >125 cm/s
andend-diastolic velocity (EDV) <110 cm/s or ICA/CCA PSV ratio >2 but <4
-
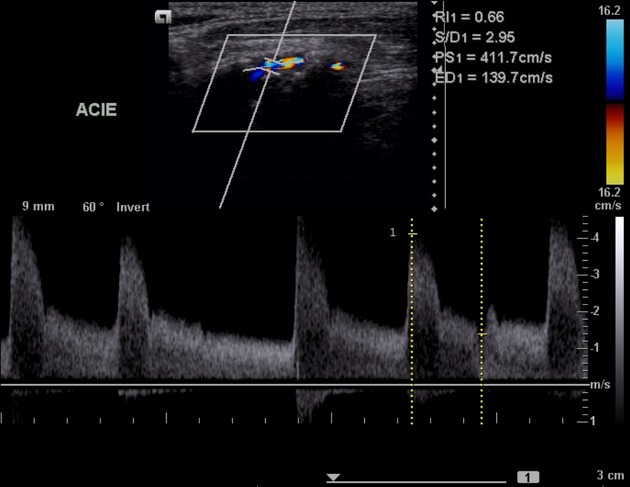
70-79% stenosis
-
pansystolic spectral broadening with PSV >270 cm/s
or
EDV >110 cm/s
orICA/CCA PSV ratio >4
-
80-99% stenosis: EDV >140 cm/s
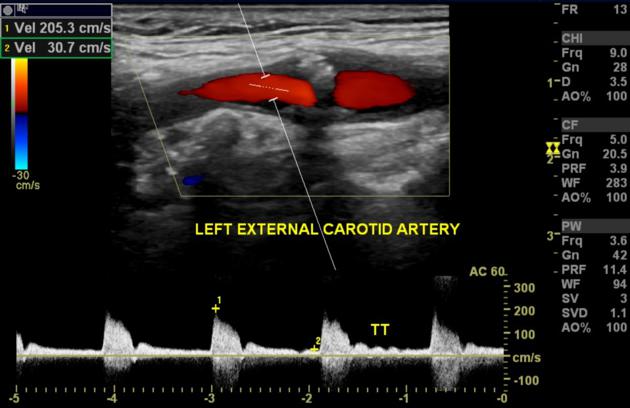
complete occlusion: no flow; terminal thump
Other criteria
Australasian Society for Ultrasound in Medicine
The following criteria were approved in 2021 7.
-
0
normal waveform and image
-
<50% diameter reduction: PSV and ICA/CCA
peak systolic velocity (PSV) <125 cm/s
ICA/CCA PSV ratio <2
-
50-69% diameter reduction: ICA/CCA with or without PSV
peak systolic velocity (PSV) >125 cm/s
ICA/CCA PSV ratio >2
-
70-79% diameter reduction: PSV or EDV or ICA/CCA
peak systolic velocity (PSV) >270 cm/s
end-diastolic velocity (EDV) >110 cm/s
ICA/CCA PSV ratio >4
-
>80% diameter reduction: PSV and EDV and ICA/CCA
peak systolic velocity (PSV) >270 cm/s
end-diastolic velocity (EDV) >140 cm/s
ICA/CCA PSV ratio >4
-
95-99% near occlusion
velocities can be high or low but criteria for >80% reduction may apply
correlate with B-mode and color Doppler appearances, including string sign
-
occluded
no flow; terminal thump





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.