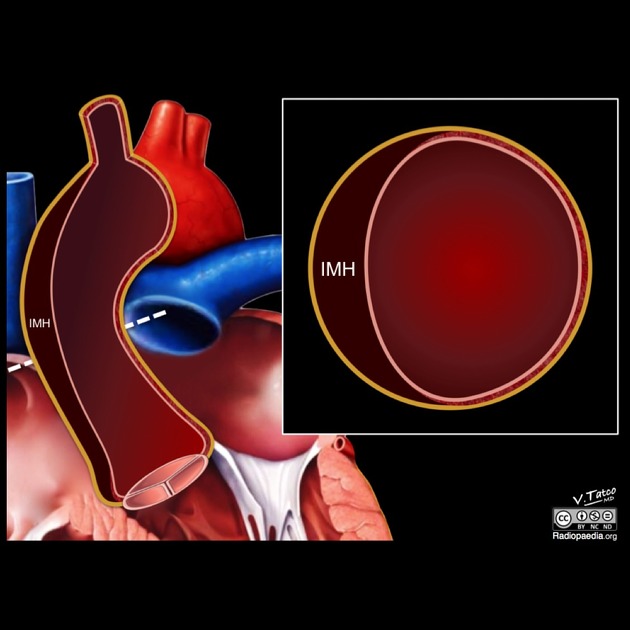
Aortic intramural hematoma (IMH) is an atypical form of aortic dissection due to a contained hemorrhage into the aortic wall usually from the vasa vasorum without an intimal tear. It forms part of the acute aortic syndrome spectrum along with penetrating atherosclerotic ulcer and classical aortic dissection.
On this page:
Epidemiology
Typically, aortic intramural hematomas are seen in elderly hypertensive patients. The same condition may also develop as a result of blunt chest trauma with aortic wall injury or a penetrating atherosclerotic ulcer 1,2.
Associations
Acute intramural hematoma may coexist with other forms of acute aortic syndrome (e.g. aortic dissection) and/or hemopericardium 14.
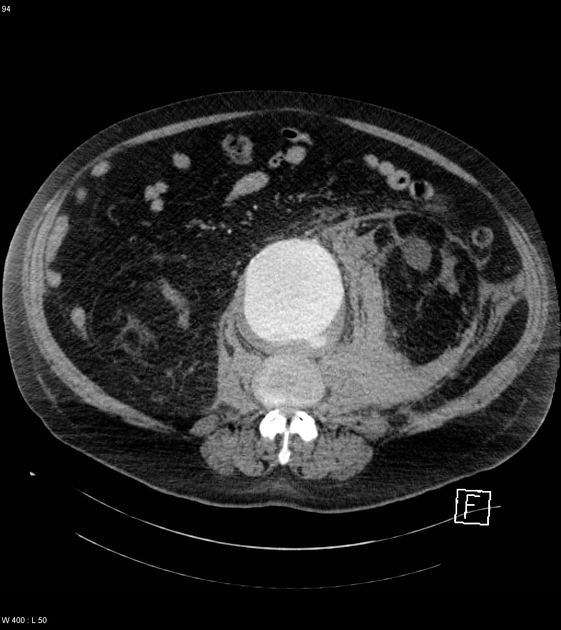
Patients with aortic intramural hematoma and penetrating atherosclerotic ulcers have an increased risk of concomitant abdominal aortic aneurysm 13.
Clinical presentation
The clinical features of intramural hematoma are those of the acute aortic syndromes, namely chest pain radiating to the back and hypertension 14.
Pathology
This condition is thought to begin with spontaneous rupture of the vasa vasorum, the blood vessels that penetrate the outer half of the aortic media from the adventitia and arborize within the media to supply the aortic wall 2. Other theories describing the pathogenesis include thrombosis of a dissection lumen, microscopic intimal tears, progression from a penetrating atherosclerotic ulcer and traumatic medial injury 13.
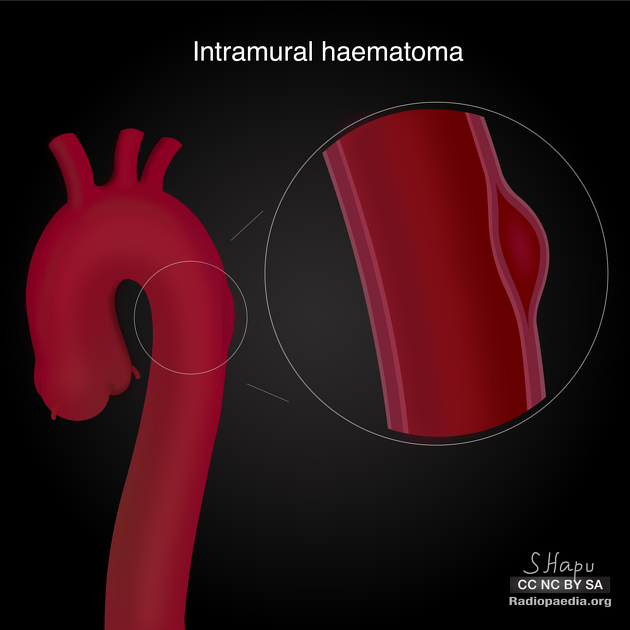
The hematoma propagates along the medial layer of the aorta. Consequently, intramural hematoma weakens the aorta and may progress either to outward rupture of the aortic wall or to inward disruption of the intima, the latter leading to a communicating aortic dissection 2.
Location
Aortic intramural hematoma has a greater predilection to involve the descending aorta 13.
Classification
Similar to aortic dissections, aortic intramural hematomas are classified according to the Stanford classification 4:
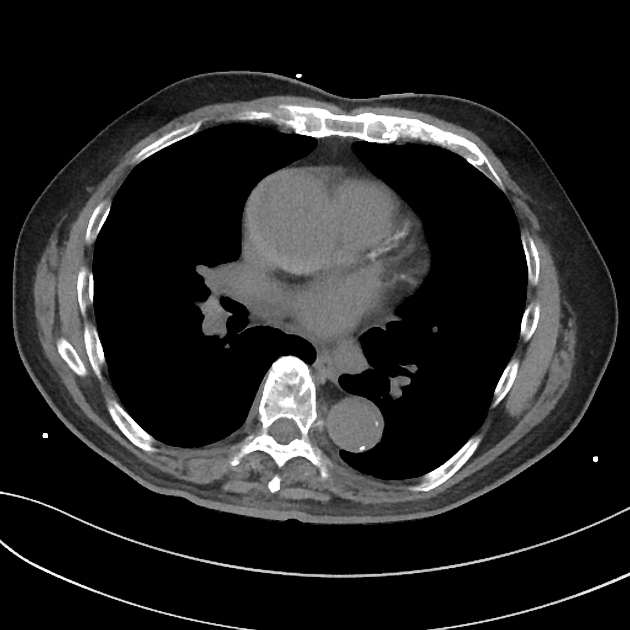
type A: involves the ascending aorta, with or without descending aortic involvement
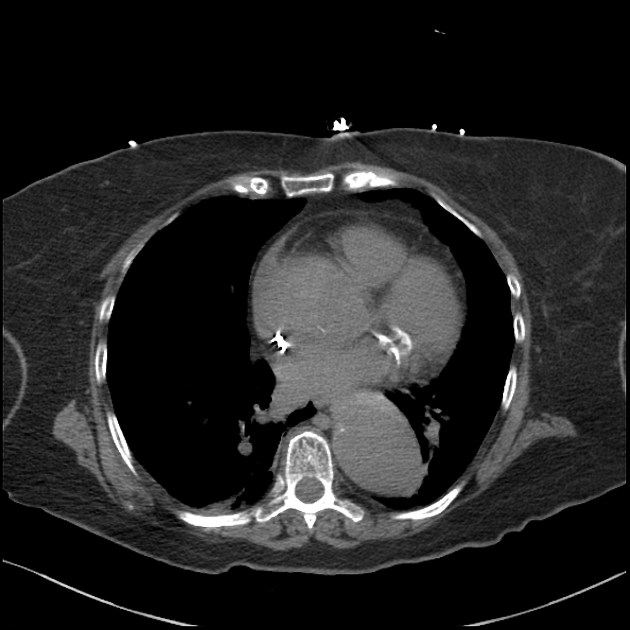
type B: confined to the descending aorta, distal to the origin of the left subclavian artery
The DeBakey classification can also be used 5.
Radiographic features
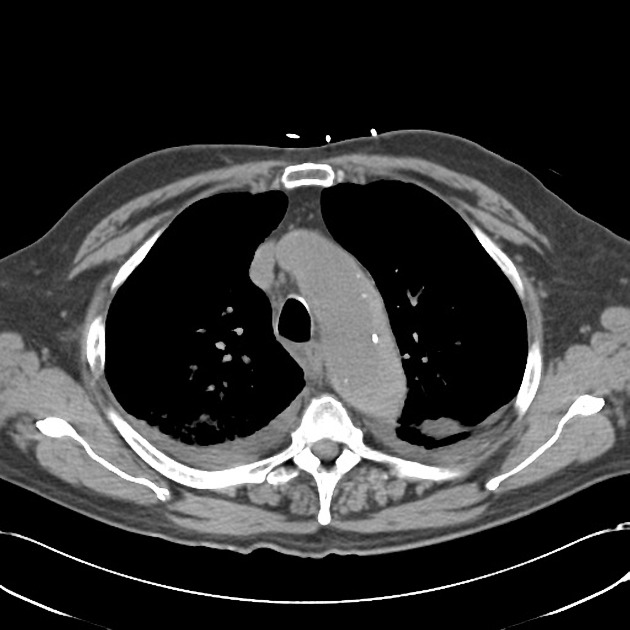
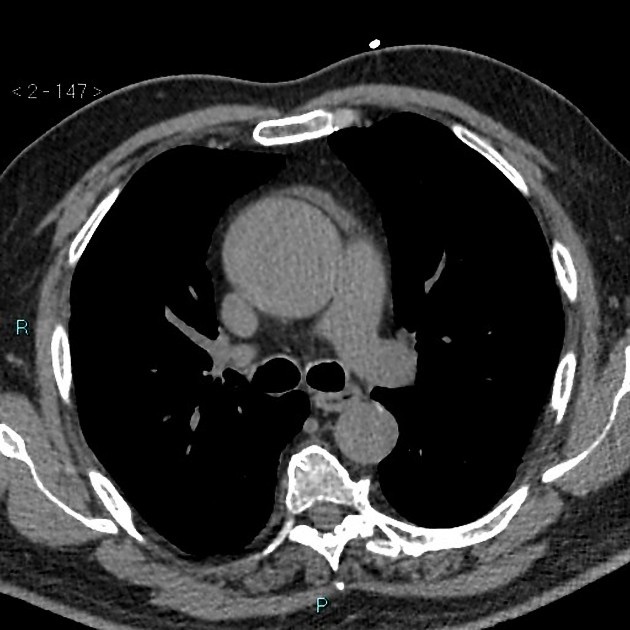
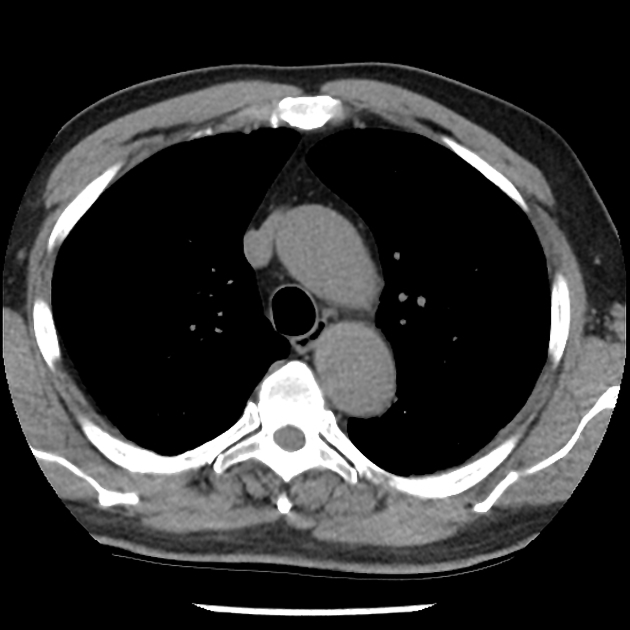
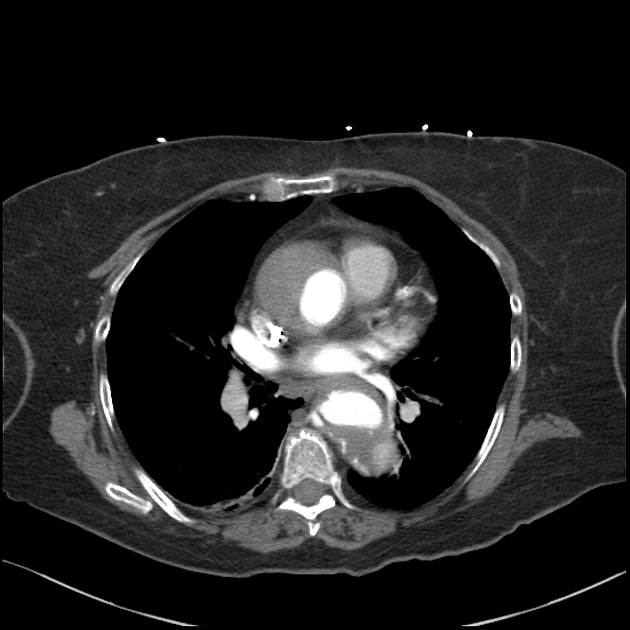
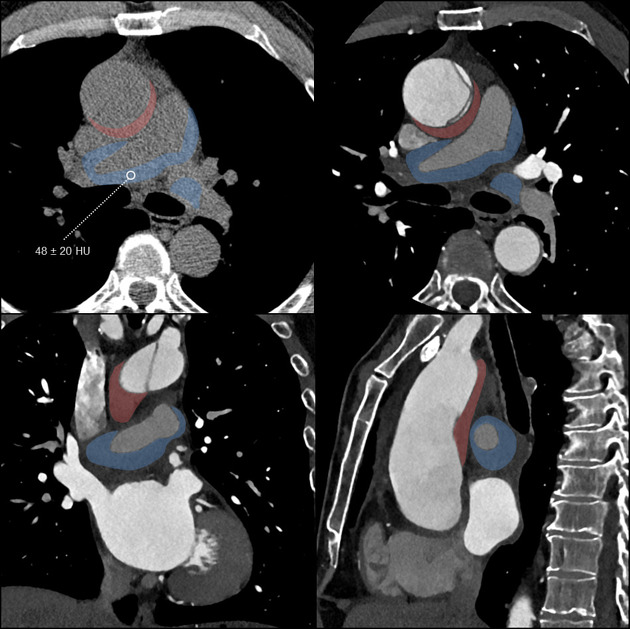
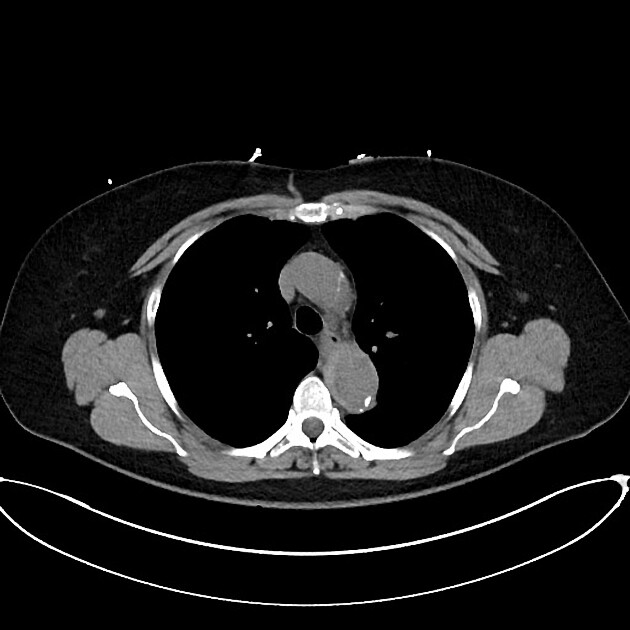
CT
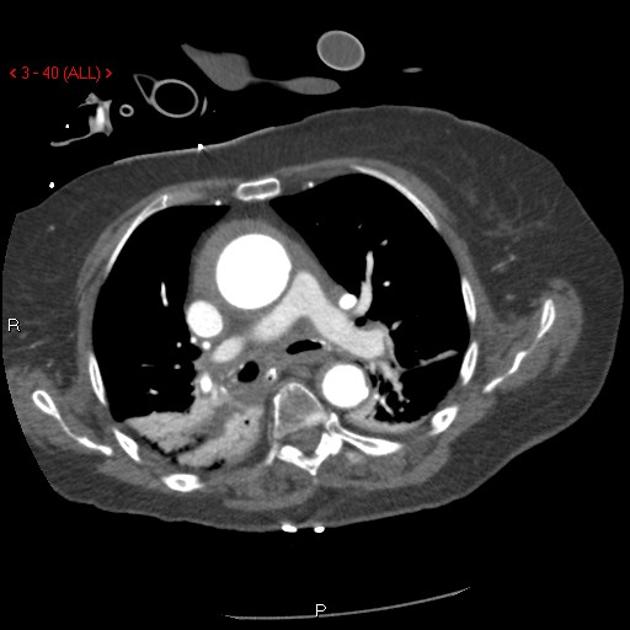
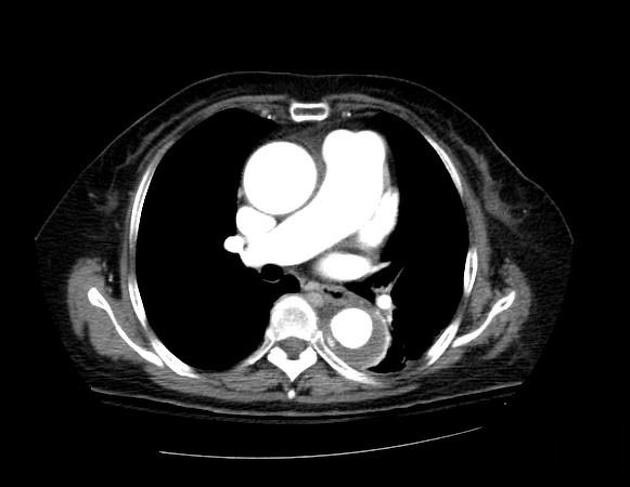
Acute intramural hematomas appear as focal, crescentic, high-attenuating (60-70 HU) regions of eccentrically thickened aortic wall on non-contrast CT (high-attenuation crescent sign). A narrow window width is essential for identifying subtle lesions 6. Intimal calcification may be displaced inwards, best appreciated in the non-contrast phase. Thickening is greater than the normal aortic wall thickness.
The lesions exhibit low attenuation in relation to the aortic lumen on post-contrast CT and can be far more subtle, hence a non-contrast phase before CTA is often the first series performed in an acute aortic syndrome protocol. Unlike aortic dissection, no intimal flap is present on the CTA. On follow-up imaging, contrast can occasionally be seen within the intramural hematoma. It is important to distinguish between aortic dissection and acute intramural hematoma as they have different prognostic significance 11.
-
small region of contrast accumulation within the hematoma with invisible or small (<2 mm) communication with the true lumen, often with a peripheral connection with an intercostal or lumbar artery 11
often regress with no adverse prognostic implications 11
ulcer-like projection: new intimal disruption (not present in the original study) with a wide neck - these usually progressively enlarge and herald a poor prognosis 11
The direction of atheromatous calcification displacement can help differentiate intramural hematoma from mural thrombus:
calcification displaced towards the aortic lumen in intramural hematomas
calcification displaced away from the aortic lumen in mural thrombus
A CTA radiology report of an intramural hematoma should include 13:
proximal and distal extent of the hematoma
the thickness of the hematoma
maximal diameter of the affected aortic lumen
presence and thickness of associated penetrating atherosclerotic ulcer
Echocardiography
An intramural hematoma may be readily visualized with transesophageal echocardiography, which offers superior visualization of the aorta than is usually available via transthoracic examinations. Defining features include 10:
-
crescentic thickening of the aortic wall
normal aortic wall thickness <3 mm
wall thickness must exceed 7 mm to diagnose intramural hematoma
-
wall demonstrates mixed echogenicity
predominantly echodense with scattered internal echolucencies
-
no internal flow detectable
-
color flow Doppler interrogation is important to differentiate from aortic dissection
the true lumen of dissection will demonstrate systolic flow
variable flow patterns may be present in a false lumen, which tends to expand in size during diastole
-
-
lack of an intimal (dissection) flap
the luminal surface in intramural hematoma tends to be smooth and continuous
Other modalities
MRI may also detect the abnormality but conventional angiography will not.
Treatment and prognosis
If an intramural hematoma involves the ascending aorta (Stanford A), surgical treatment is offered to prevent rupture and progression to classic aortic dissection, which occurs in ~30% (range 20-45%) of patients 14. Medical management of type A intramural hematoma leads to mortality of 40% 13.
Conservative management is indicated for an intramural hematoma of the descending aorta (Stanford B).
77% of intramural hematomas regress at 3 years
survival of >90% at 5 years 7
Risk factors for progression of intramural hematoma and worse prognosis include 13:
presence of ulcer-like projections (ULPs) 15
IMH thickness greater than 10 mm
associated aortic aneurysm
increase in the thickness of the intramural hematoma at follow-up CTA
Untreated, an intramural hematoma can be life-threatening as it can lead to:
Differential diagnosis
The main differential diagnoses are:
thrombosed false lumen in classic aortic dissection: typically spirals longitudinally around the aorta whereas an intramural hematoma usually maintains a constant circumferential relationship with the aortic wall
aortitis: typically shows concentric uniform thickening of the aortic wall with or without peri-aortic inflammatory stranding, whereas an intramural hematoma is often eccentric in configuration








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.