Cirrhosis (plural: cirrhoses) is the common endpoint of a wide variety of chronic liver disease processes which cause hepatocellular necrosis. Cirrhosis can be diagnosed with ultrasound, CT, and MRI, and these imaging modalities can also be used to evaluate for possible complications of cirrhosis, such as portal hypertension or hepatocellular carcinoma.
On this page:
Epidemiology
The demographics of cirrhosis reflect the underlying causes. Alcohol use and viral hepatitis from intravenous drug use or in an endemic region are the common causes.
The distribution of underlying etiology will vary regionally, with viral hepatitis being much higher in the developing world, especially in Asia. A typical distribution of causality in Western nations is as follows 4:
alcohol: 60-70%
-
viral hepatitis: 10%
hepatitis B virus most common in sub-Saharan Africa and Asia 14
hepatitis C virus is most common in Western countries and Japan 14
cryptogenic/metabolic dysfunction–associated steatohepatitis (MASH): 10-15%
biliary disease: e.g. primary sclerosing cholangitis (PSC), primary biliary cholangitis (PBC): 5-10%
metabolic disease: e.g. hereditary hemochromatosis, Wilson disease, alpha-1-antitrypsin deficiency: 5%
vascular disease: e.g. congestive hepatopathy (right heart failure), Budd-Chiari syndrome, hepatic veno-occlusive disease (rare)
cystic fibrosis: uncommon but increasing with increased survival
medications: e.g. methotrexate
Clinical presentation
The diagnosis is made either at screening for cirrhosis due to known risk factors, elevated liver enzymes, or discovered incidentally in an examination for non-specific symptoms (e.g. right upper quadrant pain). It may also present due to one of its complications:
Pathology
Focal hepatocellular necrosis caused by a variety of insults (see above) is accompanied by the three characteristics of cirrhosis 3:
fibrosis
nodular regeneration
distortion of hepatic architecture
Although traditionally cirrhosis has been divided into micro-and macronodular cirrhosis, many entities begin as micronodular (<3 mm) 9 and progress to macronodular (e.g. alcoholic cirrhosis), and thus it is of limited utility as a classification scheme 4.
Severity scoring
clinical scoring: Child-Pugh scoring system
liver biopsy histology: METAVIR score
Radiographic features
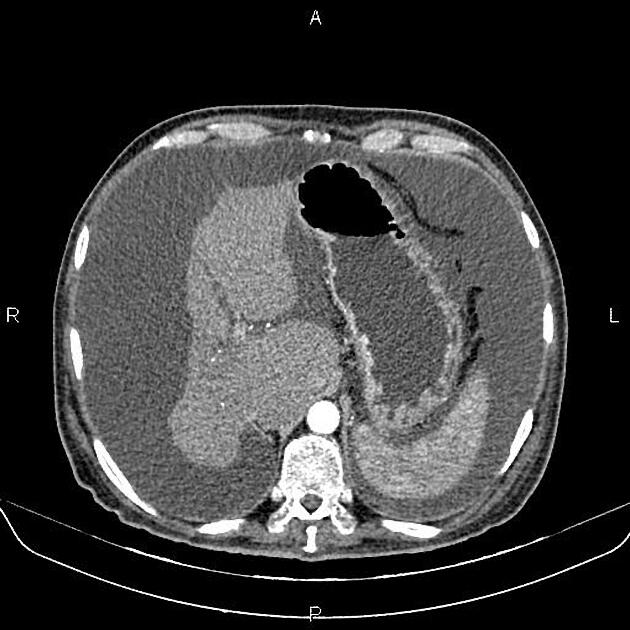
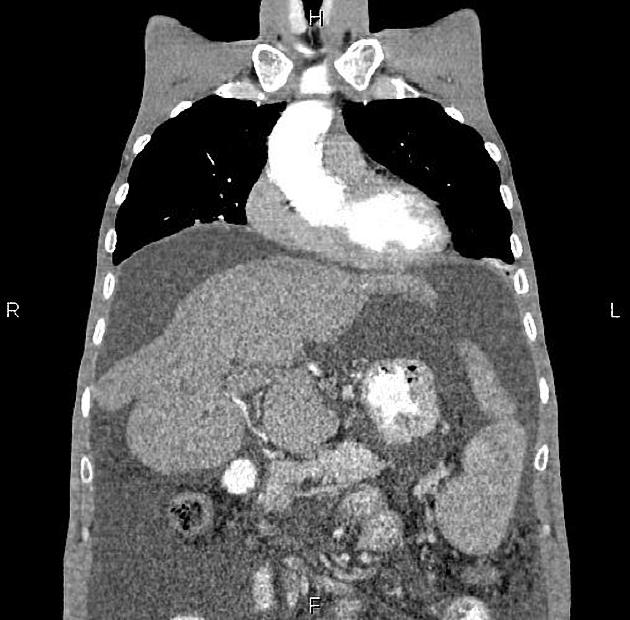
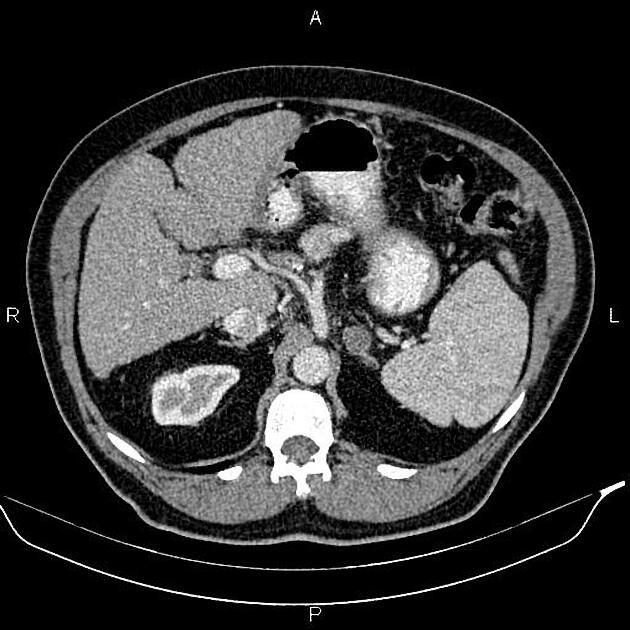
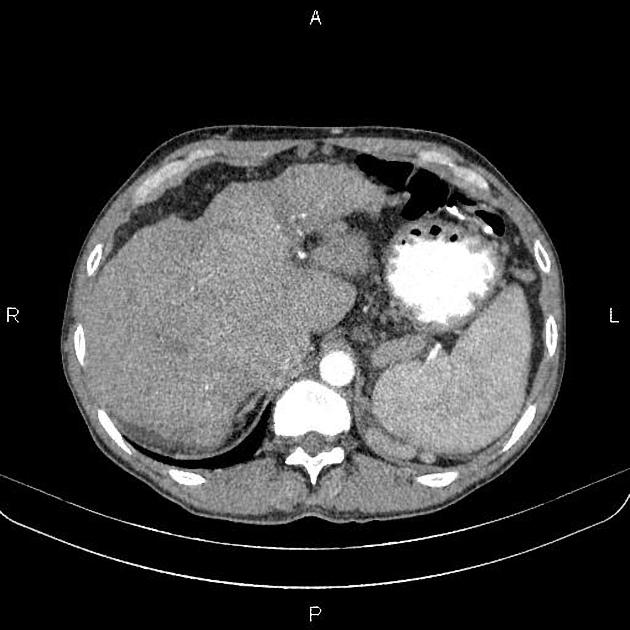
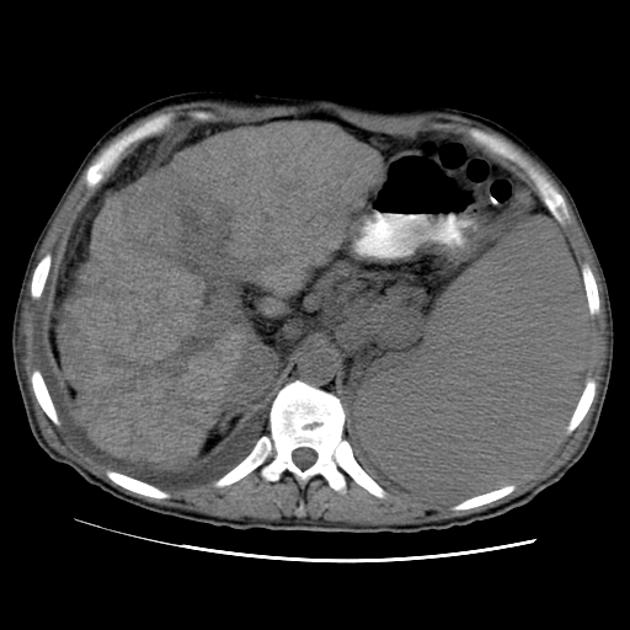
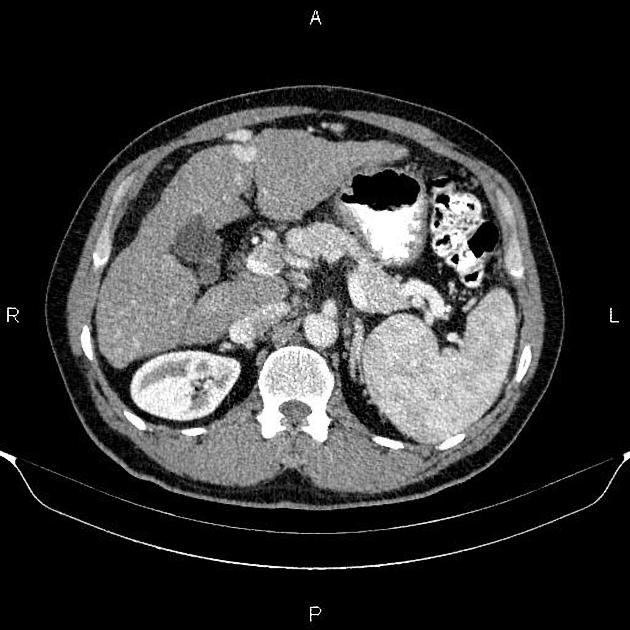
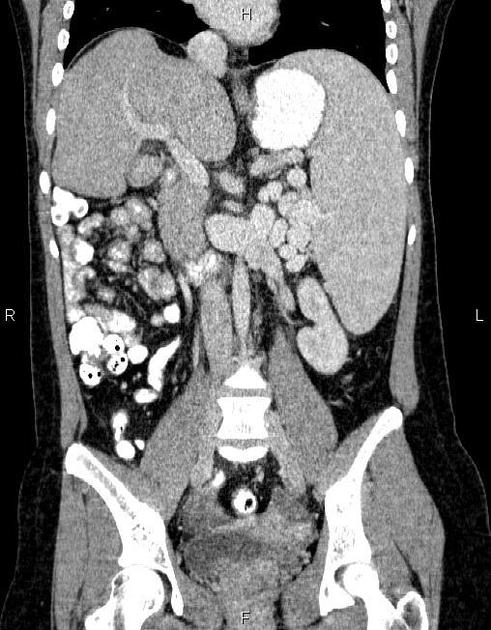
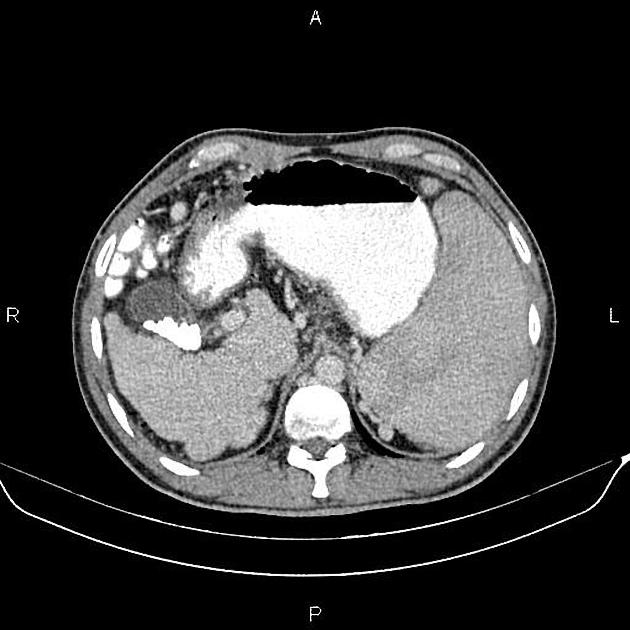
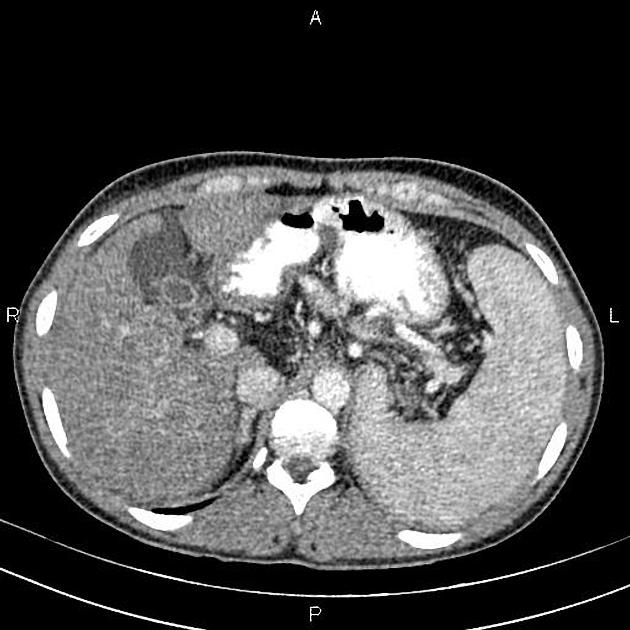
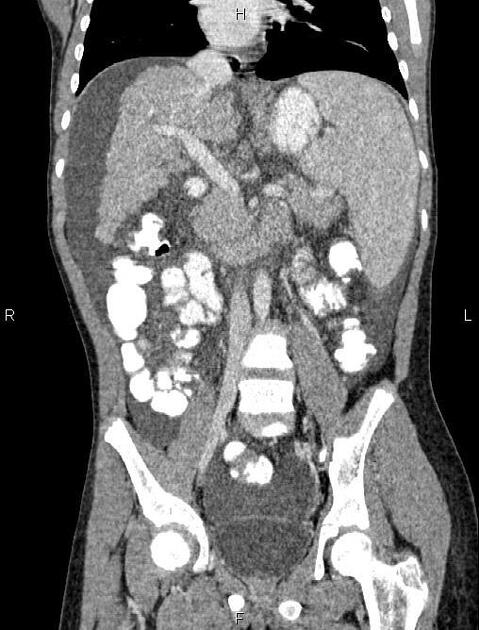
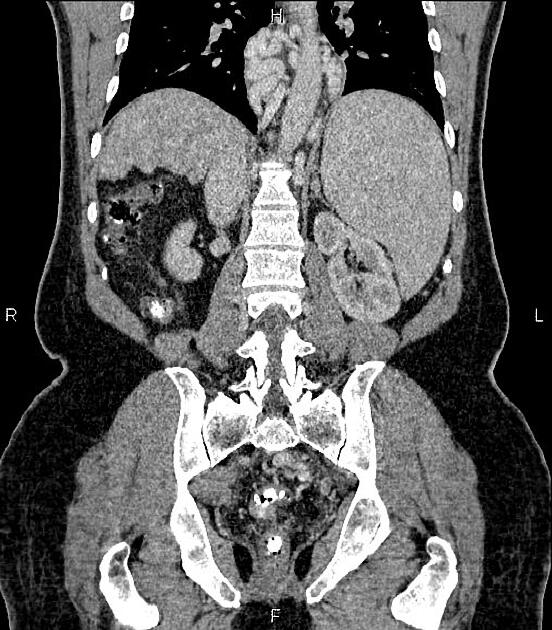
Frequent findings in advanced cirrhosis include hypertrophy of the caudate lobe and lateral segments of the left lobe (segments 2 and 3) with concomitant atrophy of the posterior segments (6 and 7) of the right lobe. These changes are likely related to changes in blood flow between the segments. See article: caudate-right lobe ratio (C/RL).
Imaging is not reliable enough to differentiate between various underlying etiologies.
The main imaging challenge is distinguishing regenerative nodules, siderotic nodules and dysplastic nodules from:
small hepatocellular carcinoma: early arterial enhancement with washout
hepatic metastases: typically high T2
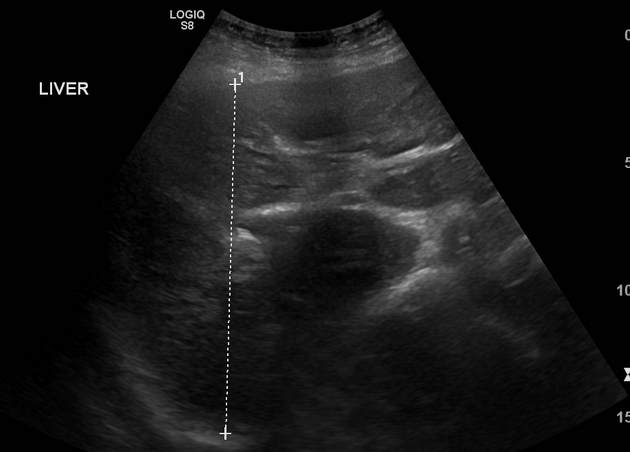
Ultrasound
Ultrasound is a major screening tool for cirrhosis and its complications. It is also useful to aid for biopsy. Appearances include:
surface nodularity: 88% sensitive, 82-95% specific 5
overall coarse and heterogeneous echotexture
-
segmental hypertrophy/atrophy (see above)
caudate width: right lobe width >0.65 (43-84% sensitive, 100% specific 5)
reduction of the transverse diameter (<30 mm) of the medial segment of the left lobe (segment 4) 11
-
signs of portal hypertension
-
Doppler flow changes
-
portal venous system
enlarged portal vein: >13 mm (42% sensitive, 95-100% specific 6)
slow portal venous flow <15 cm/sec
reversal or to-and-fro portal venous flow
-
enlarged superior mesenteric vein and splenic vein: >10 mm
NB: this should be measured during deep inspiration as size can vary
loss of respiratory variation in superior mesenteric vein and splenic vein spectral Doppler waveforms
enlarged paraumbilical vein with hepatofugal flow 17
-
hepatic veins
portalisation of hepatic vein waveform
-
hepatic arteries
"corkscrew" appearance
increased velocity (compensating for decreased portal vein flow)
-
fatty change (variable)
-
Sonoelastography may also be useful to assess the amount of liver fibrosis 12. Suggested values for diagnosis are:
>7 kPa: advanced fibrosis
12.5-15 kPa: cirrhosis
Contrast-enhanced ultrasound may have a role in the diagnosis of cirrhosis, as diminished mean hepatic venous transit time is similar to that of perfusion CT 13.
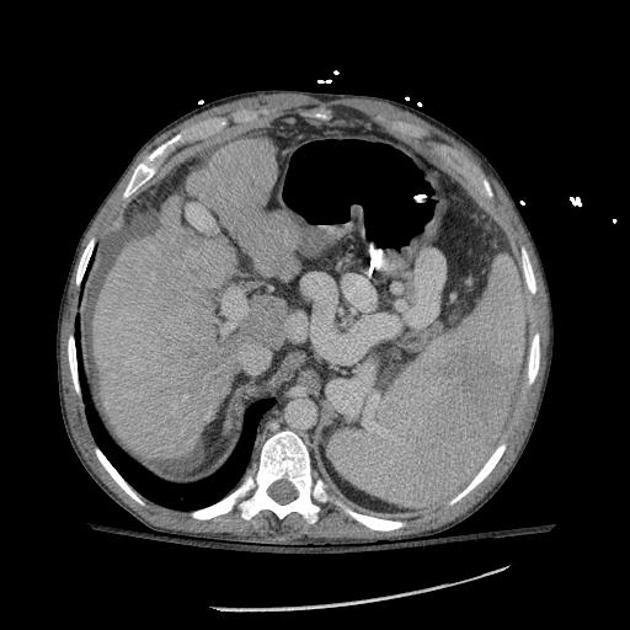
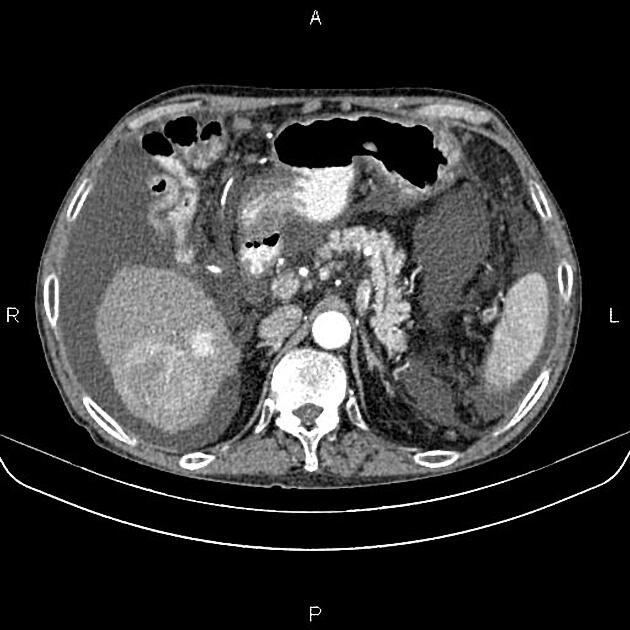
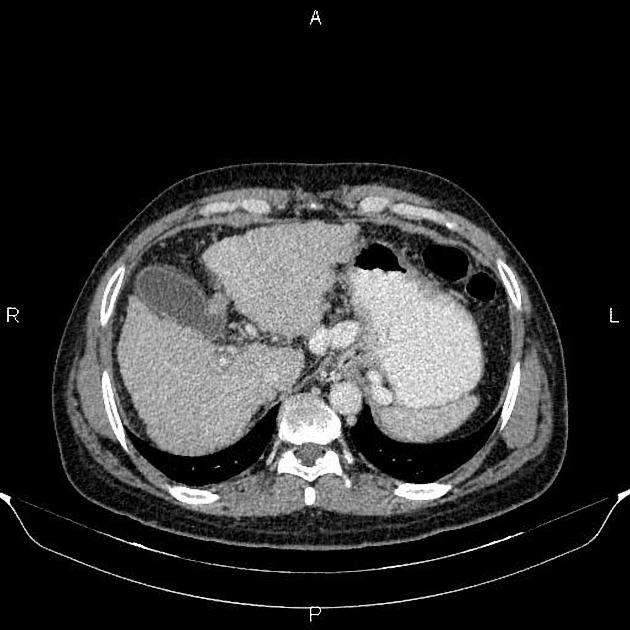
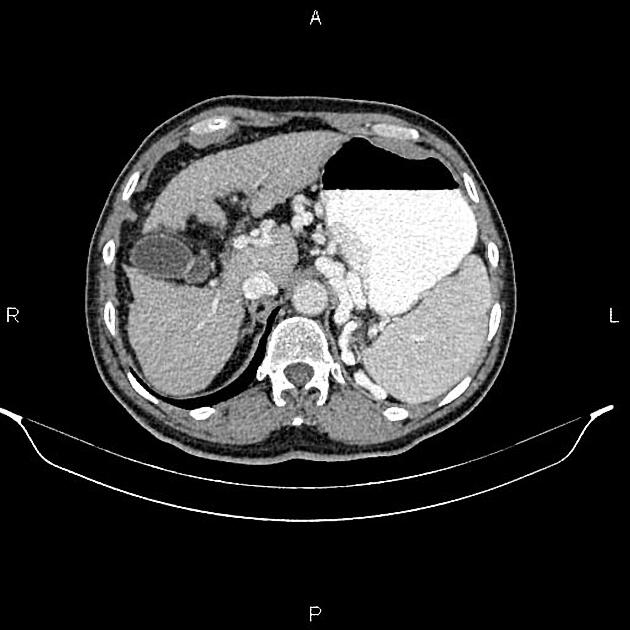
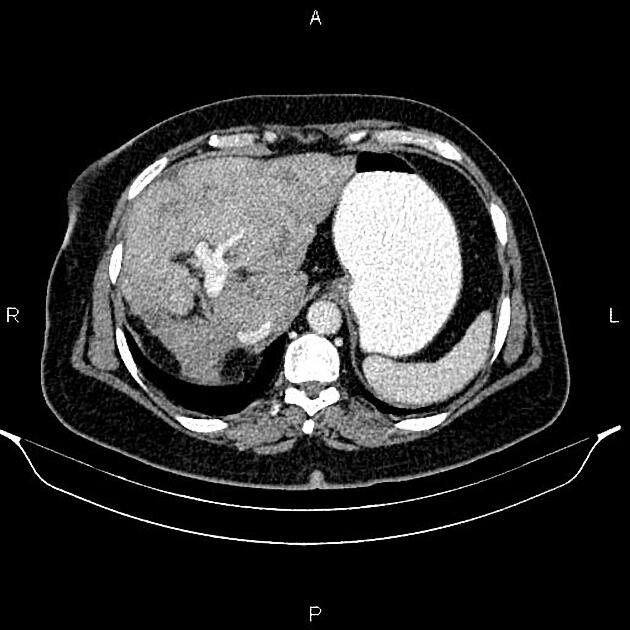
CT
CT is insensitive in early cirrhosis. More established findings include:
-
surface and parenchymal nodularity
regenerative nodules (majority): isodense/hyperdense to the rest of liver
siderotic nodules (minority): hyperdense due to accumulation of iron 6
fatty change (variable)
parenchymal heterogeneity both on the pre and post intravenous contrast scans
predominantly portal venous supply to dysplastic nodules
in advanced cirrhosis, nodular margin and lobar hypertrophy/atrophy may be demonstrated (see above)
-
signs of portal hypertension
portal vein enlargement
portal venous thrombosis +/- cavernous transformation
splenomegaly
enlarged superior mesenteric vein and splenic vein
enlarged paraumbilical vein
portosystemic collaterals
upper abdominal lymphadenopathy in end-stage disease 16
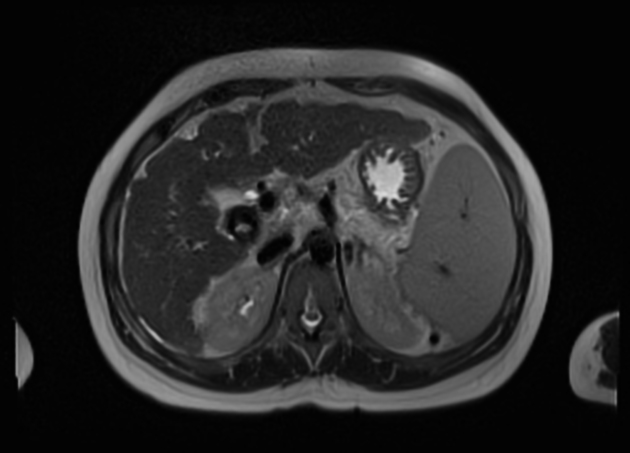
MRI
MRI is also insensitive in early cirrhosis but has a significant role in screening cirrhotic livers for small hepatocellular carcinomas (see LI-RADS). MRI findings include:
morphologic changes (same as on CT and ultrasound)
-
regenerative nodules (or cirrhotic nodules)
-
T1
variable, usually isointense
occasionally mildly hyperintense
no early enhancement and washout as most supply is from the portal vein 7,9
-
T2
usually isointense 9
hypointense if siderotic
-
-
maybe of low or high grade, and thus have a variable appearance
low-grade nodules will resemble regenerative nodules
high-grade nodules will resemble hepatocellular carcinomas 9
-
small hepatocellular carcinoma (HCC)
-
T1 C+ (Gd)
arterial phase enhancement and washout 7
late enhancing capsule
growth in the interval between studies
T2: typically mildly or moderately hyperintense
-
MR angiography or a balanced steady-state free precession sequence may also be used to assess portal vein patency and portosystemic collaterals.
Treatment and prognosis
Treatment depends on the underlying etiology and presence of complications. One of the key roles of diagnostic radiology is the detection of hepatocellular carcinoma (six-monthly ultrasound should be done for surveillance as per 2018 AASLD (American Association for the Study of Liver Diseases) guidelines in cirrhotic patients to screen for hepatocellular carcinoma development) 15. Interventional radiology can be very helpful for the treatment of portal hypertension and its complications (e.g. TIPS, ascites drainage), as well as chemoembolisation or radiofrequency ablation of hepatocellular carcinoma.
Complications
History and etymology
The word cirrhosis derives from the Ancient Greek word "κιρρόειν", meaning "to turn reddish-yellow" or "tawny". The French physician René Laennec (1781-1826) was first to use the term to describe the macroscopic appearance of fibrotic changes in a liver with alcoholic cirrhosis.
Differential diagnosis
Several conditions can potentially mimic cirrhosis on imaging 10:
widespread (miliary type) liver metastases
Budd-Chiari syndrome (particularly chronic)
chronic portal vein thrombosis
nodular regenerative hyperplasia of the liver
Practical points
hepatopulmonary syndrome and hepatorenal syndrome may develop in cirrhosis











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.