Idiopathic orbital inflammation, also known as orbital pseudotumor, or idiopathic orbital inflammatory syndrome and non-specific orbital inflammation, is an idiopathic inflammatory condition that most commonly involves the extraocular muscles. Less commonly there is inflammatory change involving the uvea, sclera, lacrimal gland, and retrobulbar soft tissue.
The exact etiology is not known but an association with many inflammatory/autoimmune diseases is reported.
On this page:
Terminology
Many terms are used interchangeably in the literature to refer to idiopathic orbital inflammation including orbital pseudotumor, non-specific orbital inflammation and orbital inflammatory syndrome.
Epidemiology
Associations
The condition has been associated with other inflammatory and autoimmune conditions:
IgG4-related disease, now recognized as a separate entity: IgG4-related orbital disease
Clinical presentation
Patients typically present with rapid-onset, usually unilateral, painful proptosis and diplopia. In a minority of cases (8-20%) bilateral involvement may occur either simultaneously or metachronously 8-10. Idiopathic orbital inflammation is a diagnosis of exclusion; atypical presentation, poor response to treatment with corticosteroid and recurrence should prompt biopsy to exclude other diseases.
Pathology
Histologically acute lesions demonstrate lymphocytes (which can be mistaken for orbital lymphoma), plasma cells, and giant cell infiltration.
Classification
Division into a number of subgroups according to location has been proposed:
lacrimal pseudotumor (dacryoadenitis)
anterior pseudotumor: in the immediate retrobulbar fat
posterior pseudotumor: in the fat at the orbital apex; distinguished from Tolosa-Hunt syndrome in that the cavernous sinus is spared
myositic pseudotumor (myositis): predominantly involves the extraocular muscles and therefore mimic thyroid-associated orbitopathy (TAO) but unlike TAO it also involves the tendons
optic perineuritis: involvement of the optic nerve sheath
diffuse pseudotumor: affecting multiple compartments
Radiographic features
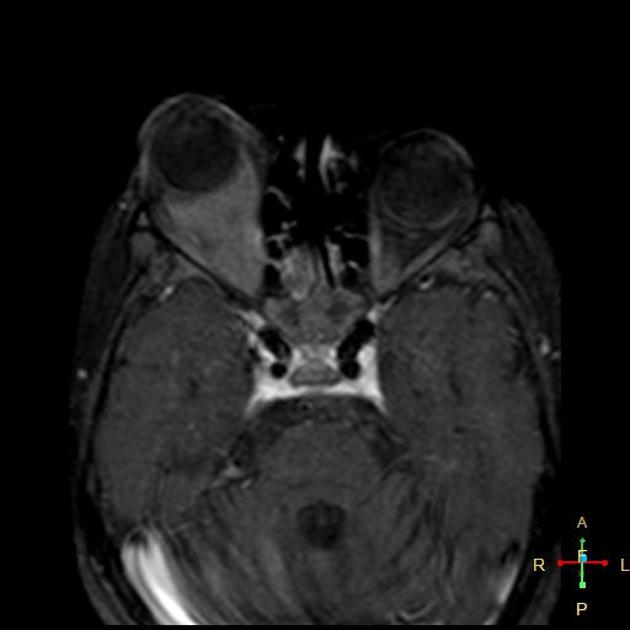
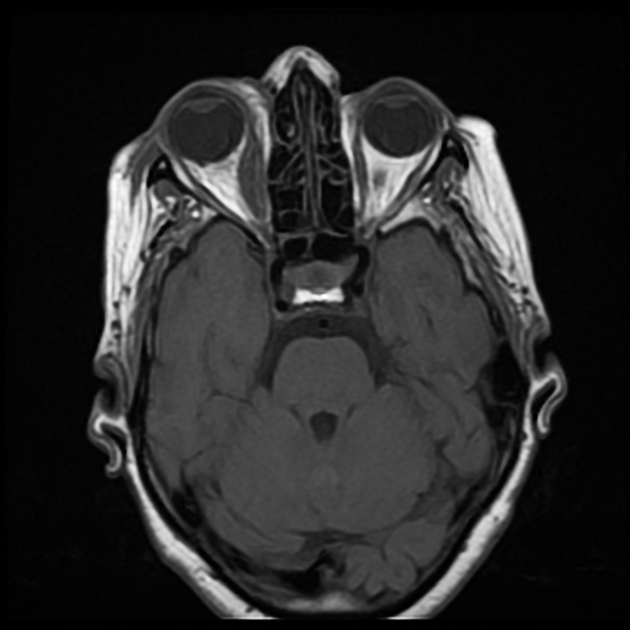
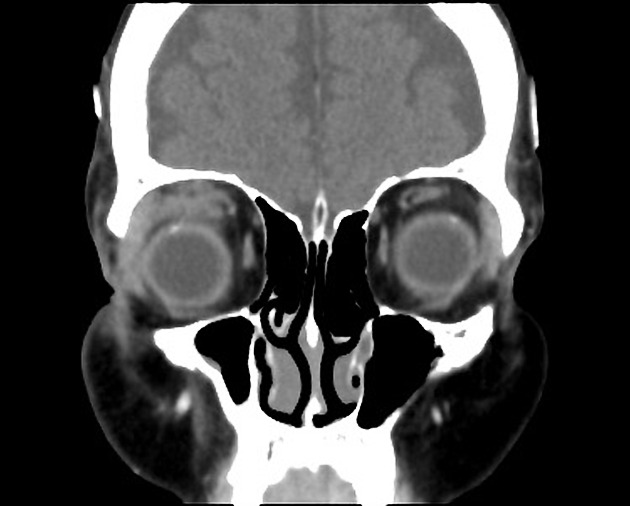
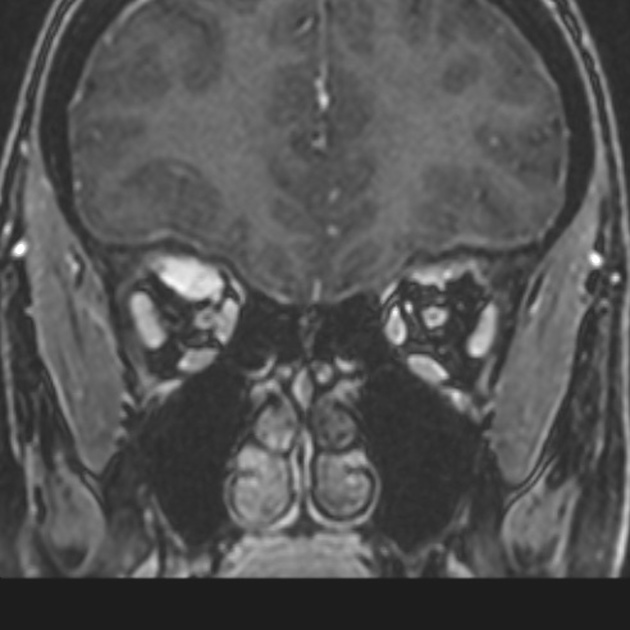
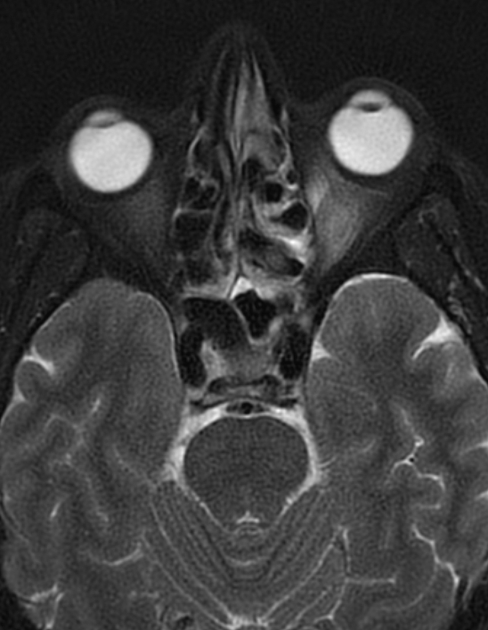
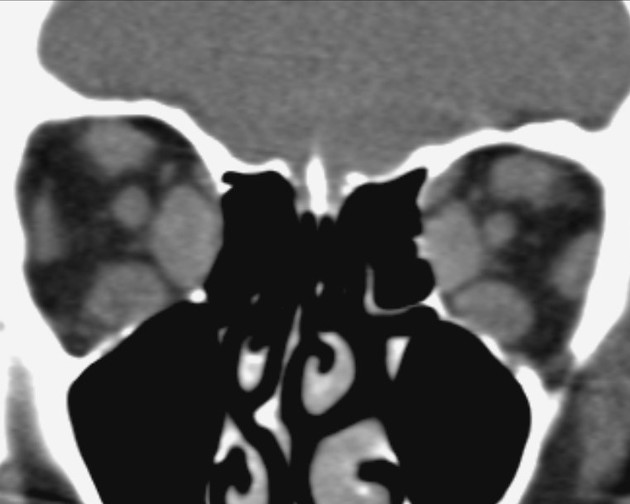
Imaging demonstrates enlargement of the muscle belly of one (or more) extraocular muscles typically with the involvement of tendinous insertions. Involvement of the tendinous insertion distinguishes the idiopathic orbital inflammation from thyroid-associated orbitopathy in which the insertion point is spared. However, sparing of the anterior tendon does not exclude the diagnosis of idiopathic orbital myositis 7.
Additional inflammation can be seen in surrounding tissues, including the orbital fat, lacrimal gland, and optic nerve sheath 9.
It can appear as an infiltrative mass and extends outside of the orbit via superior or inferior orbital fissures. Extension into the cavernous sinus, meninges, and dura can occur. It is most commonly unilateral but can be bilateral (either at the same time or sequentially) in 8-20% of cases 8-10.
MRI
Reported signal characteristics include:
T1: affected region typically isointense (to extraocular muscles) 1 but can also be hypointense 1-3
T2: affected region typically hypointense due to fibrosis and with more progression of fibrosis it becomes more hypointense, but the signal can also be iso- to hyperintense to extra-ocular muscles 2
T1 C+ (Gd): moderate to a marked diffuse enhancement
Treatment and prognosis
Most cases resolve rapidly with treatment (usually corticosteroids suffice) although in a subset with more chronic progression chemotherapy and radiotherapy may be required. A degree of residual fibrosis can be demonstrated, especially in the more refractory cases.
History and etymology
The disease was first described by Birch-Hirschfeld et al. in 1905 6. They also introduced the term orbital pseudotumor afterward in 1930 7.
Differential diagnosis
One of the main differential diagnoses of idiopathic orbital inflammation is orbital lymphoma. There is considerable overlap between these entities both clinically and radiologically. However, orbital lymphoma usually presents as a progressive orbitopathy rather than acutely, is more often bilateral, shows lower values on ADC, and does not respond to corticosteroid.
Other imaging differential considerations include:
orbital cellulitis: usually associated with a subperiosteal abscess from adjacent sinusitis or with a previous history of trauma/dental procedure
thyroid-associated orbitopathy (TAO): spares the tendinous insertions and not usually painful
Tolosa-Hunt syndrome: related condition with the involvement of the cranial nerves in the cavernous sinus and resulting ophthalmoplegia
granulomatosis with polyangiitis: bilateral involvement of the paranasal sinuses and orbits associated with osseous destruction














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.