Methanol poisoning is a cause of an acute toxic leukoencephalopathy that also has eventual chronic sequelae.
On this page:
Epidemiology
Methanol is found in a variety of consumer products including perfumes, model aircraft and car fuels, windshield washing solutions, carburator cleaners, solid cooking fuels, gas line antifreeze and photocopying fluid 5.
Contamination of unregulated ethanol containing beverages has resulted in numerous epidemics of toxicity worldwide 6. Ingestion is the most common route of exposure although rare cases of significant absorption and toxicity have resulted from inhalation as well as dermal exposure 1,2,7.
Clinical presentation
Methanol poisoning classically presents with mild central nervous system depression followed by visual dysfunction and gastrointestinal symptoms 4. A period of clinical latency often precedes the visual abnormalities 4 which ranges from less than an hour to three days.
Perturbations in vision, known as methanol-induced optic neuropathy, are bilateral and painless, with symptoms ranging from subjective blurring to complete, often persistent, blindness 5,9. Permanent neurologic sequelae may include a syndrome resembling Parkinson disease with bradykinesia, tremors, dementia and rigidity 8.
Severely poisoned patients develop an anion gap metabolic acidosis 4. Other features of severe toxicity may include shock, coma, seizures, rhabdomyolysis with myoglobinuric acute renal failure, and pancreatitis 4.
Pathology
Methanol (CH3OH) is a clear, colourless liquid which is biotransformed in-vivo to formaldehyde and formic acid; the latter metabolite is primarily responsible for the associated metabolic acidosis as well as the neurologic and ophthalmologic toxicity 4.
After absorption and distribution, methanol undergoes rapid, sequential oxidation by the hepatic enzymes alcohol and aldehyde dehydrogenase yielding formic acid which is inefficiently metabolized and thus accumulates. The formation of this organic acid is thought to be primarily responsible for the ensuing metabolic acidosis, which may be exacerbated by a concomitant elevation in lactate due to mitochondrial injury.
Formic acid binds a heme moiety in the the terminal complex of the mitochondrial electron transport chain (cytochrome oxidase) resulting in an inhibition of oxidative metabolism, ATP depletion, and cell death 4,5. The retina, optic nerve, and putamina are particularly vulnerable likely by virtue of their relative metabolic requirements and develop cytotoxic edema.
Radiographic features
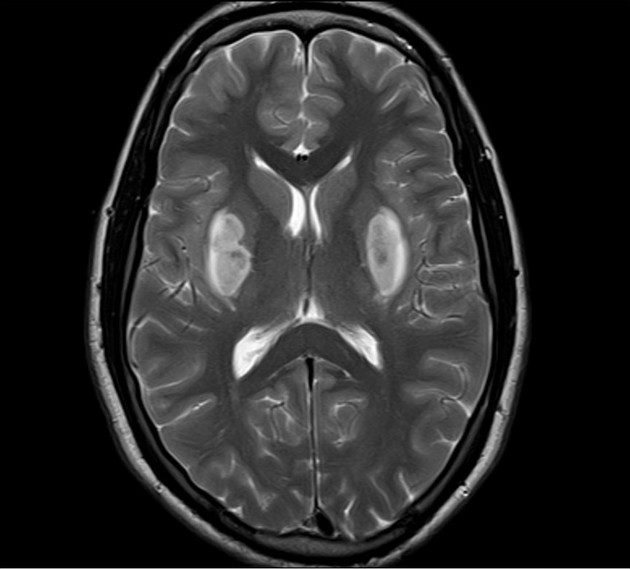
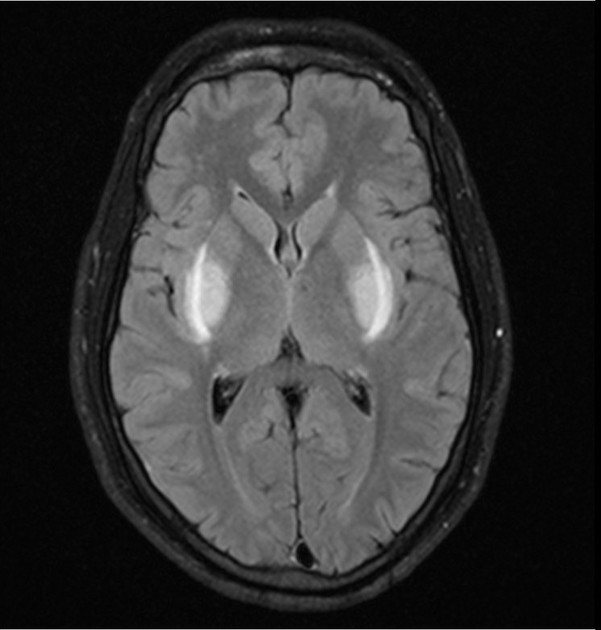
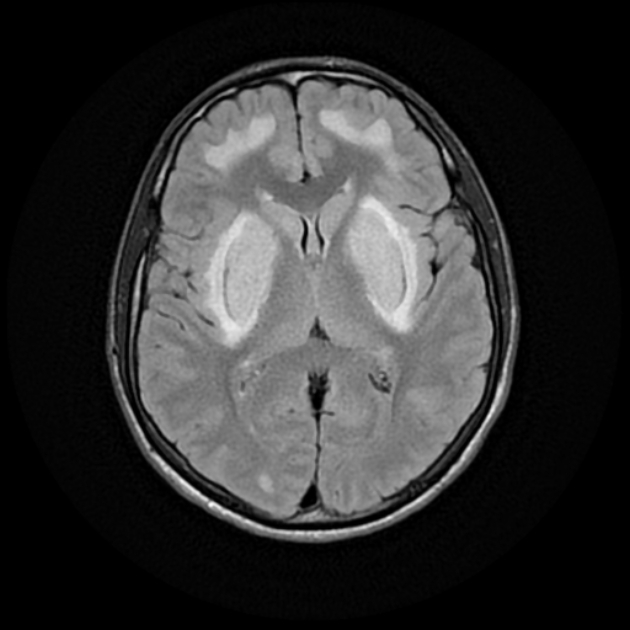
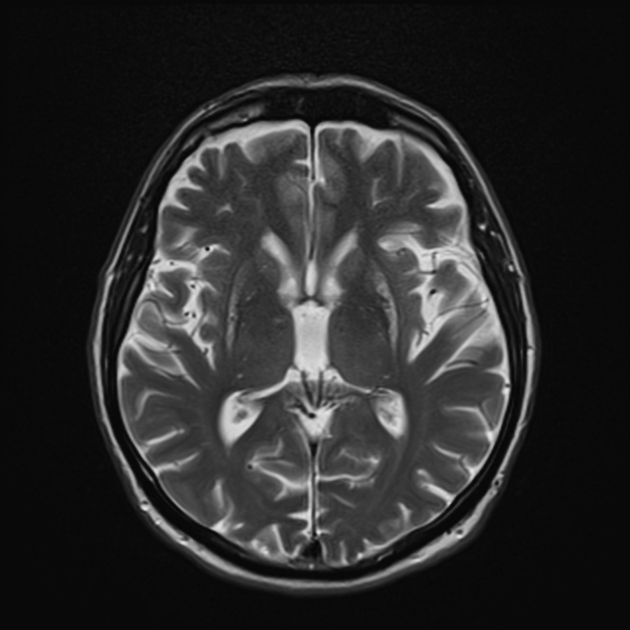
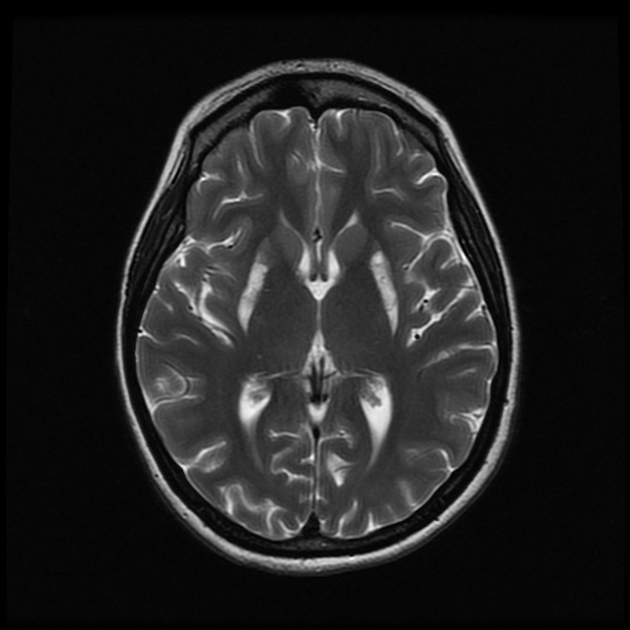
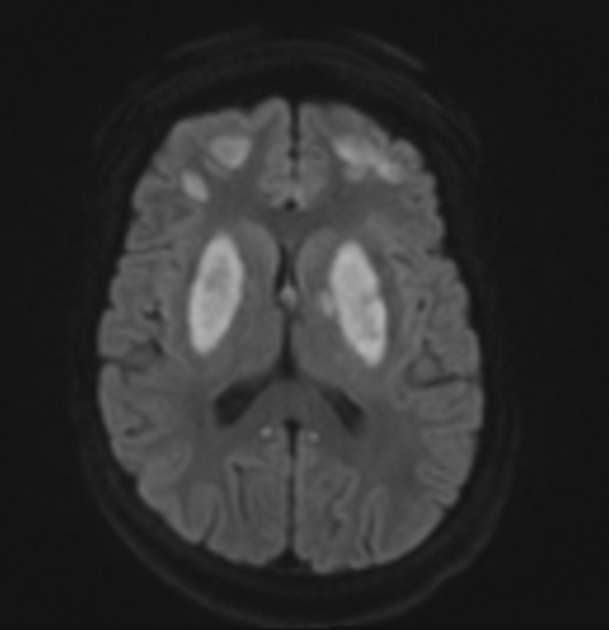
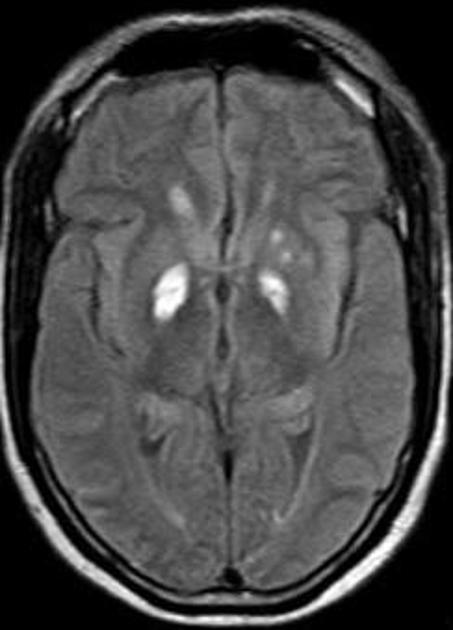
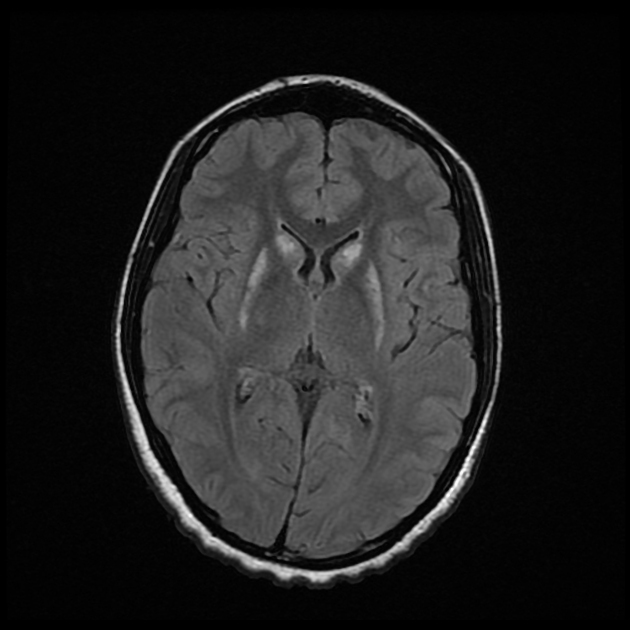
Methanol poisoning characteristically produces a pattern of symmetric, bilateral necrosis of the basal ganglia with a predilection to involve the putamina with minimal involvement of the globi pallidi 7. Other affected structures may include the subcortical white matter, optic nerves, and cerebellum 1-3.
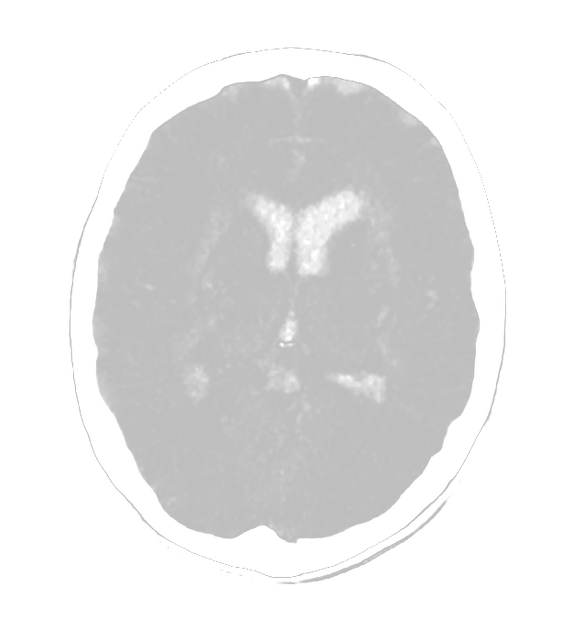
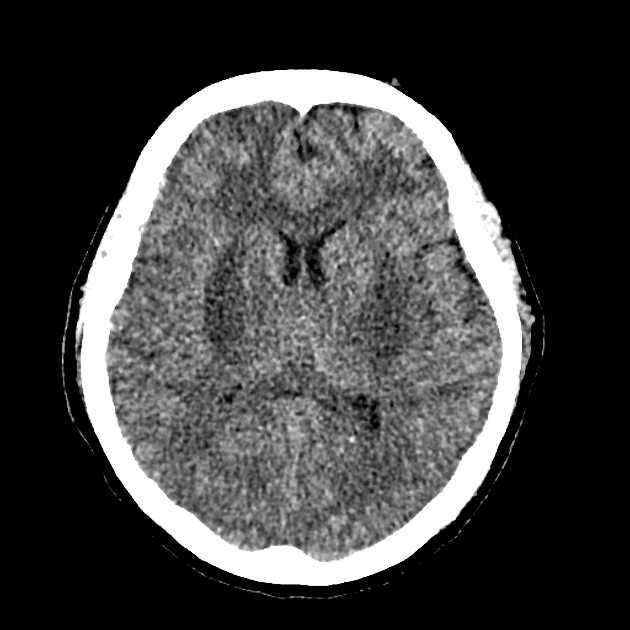
CT
Classically seen as hypo-attenuation bilaterally in the putamen, reflective of putaminal necrosis 1. Hemorrhagic necrosis appears as an area of hyperattenuation 7.
Other features include diffuse hypo-attenuation in cerebral white matter and hemorrhages 1.
MRI
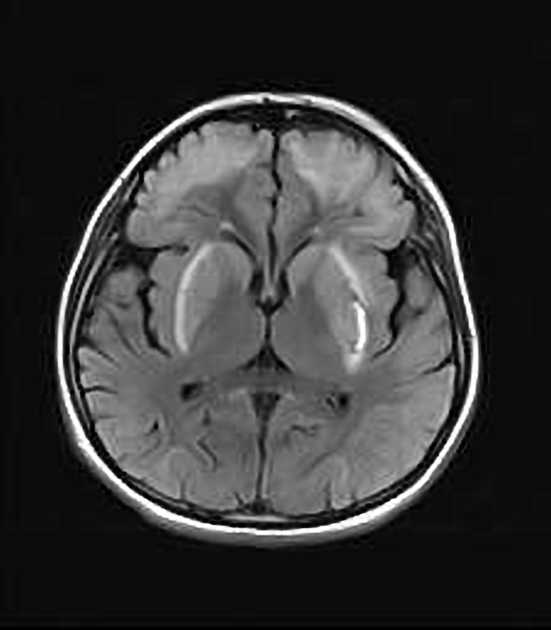
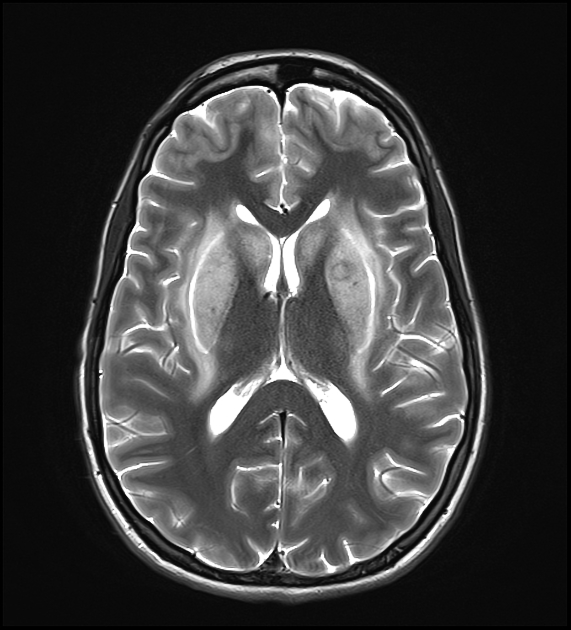
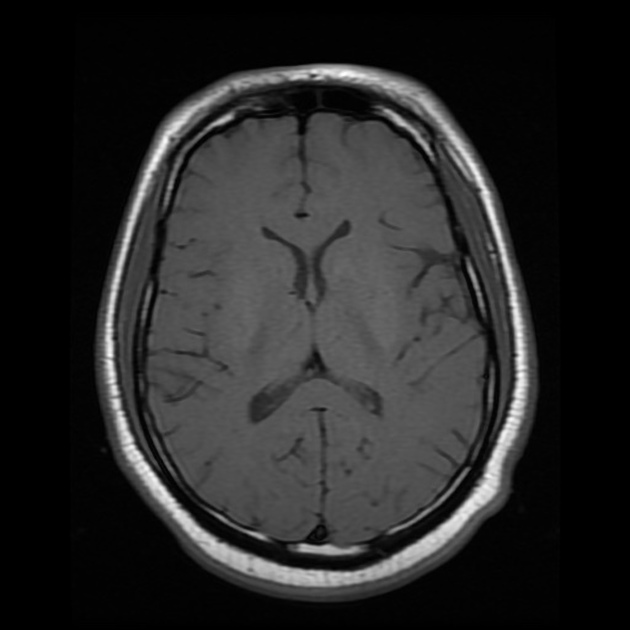
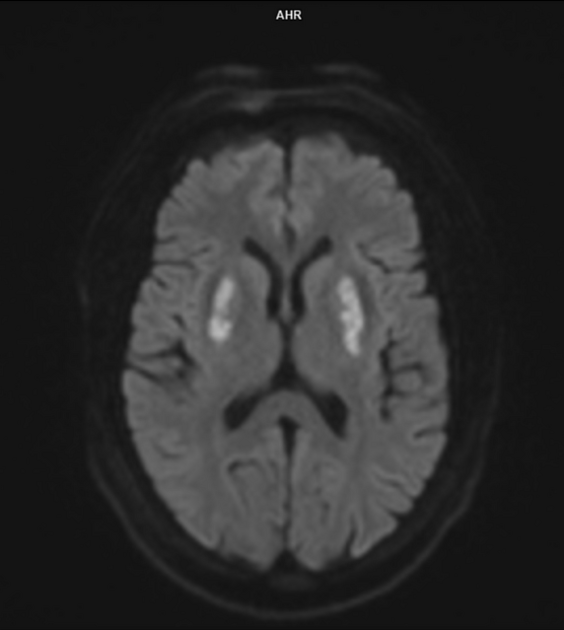
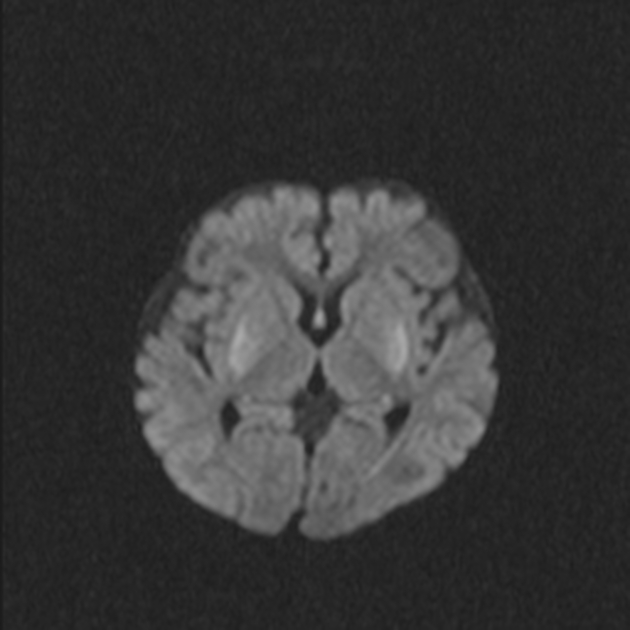
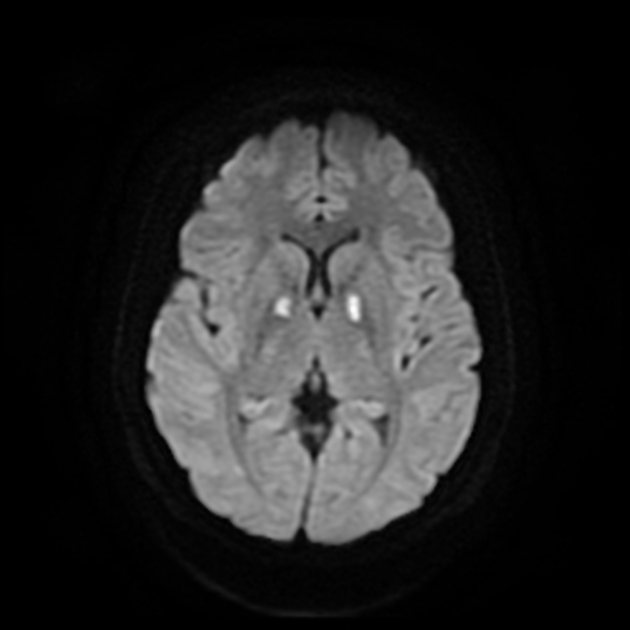
Regions of involvement are identical to those involved on CT. Signal characteristics of the characteristic putaminal necrosis in the acute setting include:
T1: variable signal depending on the presence of hemorrhage (high signal if present, otherwise low signal) 1,2
T2/FLAIR: high signal 1,2
DWI: affected areas show increased diffusion signal in the acute phase 3
T1 C+ (Gd): enhancement is variable 2
Furthermore, similar acute signal changes secondary to tissue necrosis may be noted in the optic nerves (also due to demyelination), subcortical white matter, and cerebellum 1,2,9. For example, in the optic nerves, there may be bilateral high T2 signal and contrast enhancement 9.
MR spectroscopy
Magnetic resonance spectroscopy may demonstrate an elevated lactate peak with a diminished N-acetylaspartate peak 7. In the chronic phase, cystic cavities may develop in the putamen 2.
Treatment and prognosis
Asymptomatic patients presenting with a potentially significant methanol exposure are typically administered fomepizole or ethanol while awaiting a confirmatory serum methanol level; these agents prevent the metabolism of methanol, and thereby the production of formic acid, by inhibiting alcohol dehydrogenase 4.
Patients who are symptomatic or acidotic require more aggressive management including 4:
-
serum alkalinisation with intravenous sodium bicarbonate
favors formate dissociation, which binds less avidly to cytochrome oxidase
-
administration of intravenous folinic acid
enhances formate metabolism to formyltetrahydrofolate
-
extracorporeal removal with intermittent hemodialysis
elimination of methanol and formate, restoration of acid-base status
Differential diagnosis
For involvement in and around the putamen or basal ganglia, consider:
-
other toxic encephalopathies
-
metabolic disorders










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.