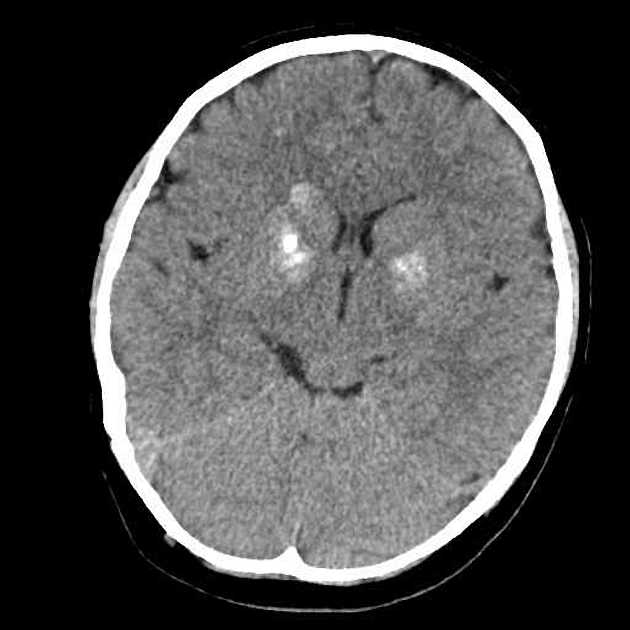
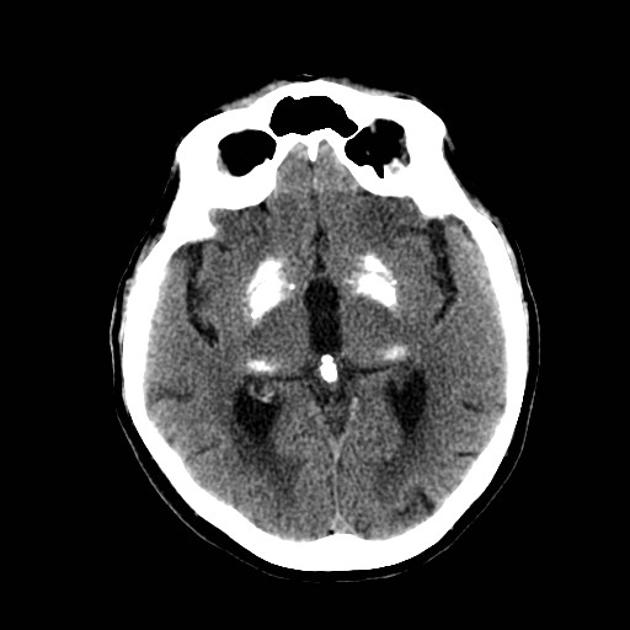
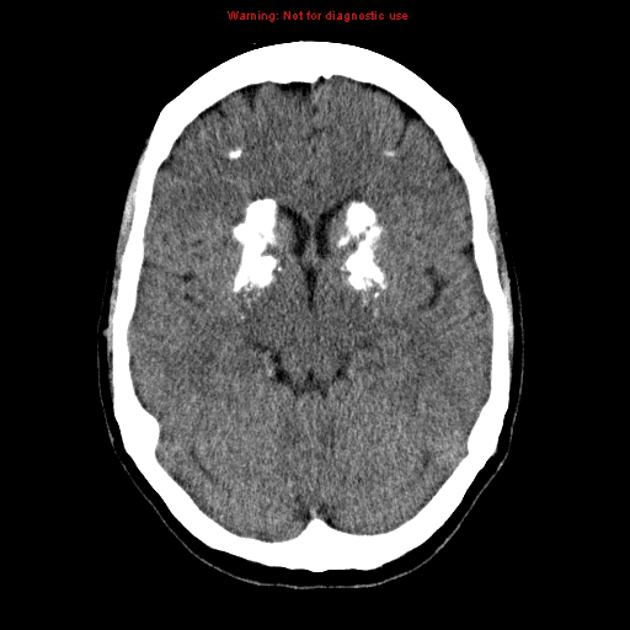
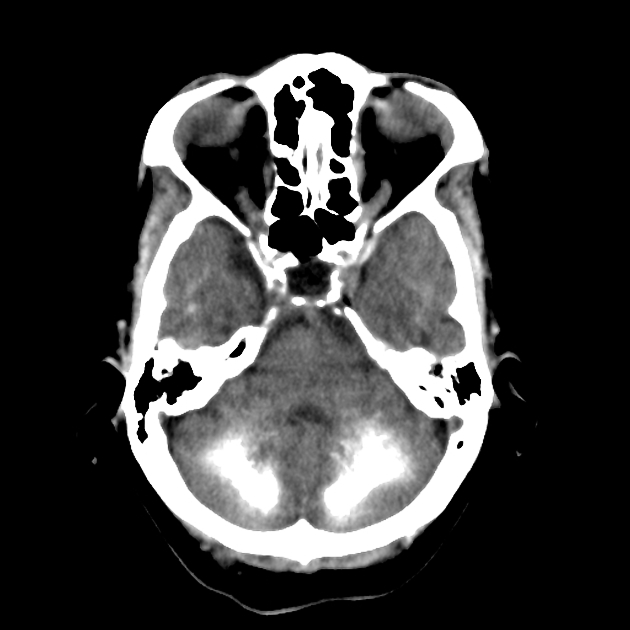
Fahr syndrome, also known as bilateral striatopallidodentate calcinosis, is characterized by abnormal vascular calcium deposition, particularly in the basal ganglia, cerebellar dentate nuclei, and white matter, with subsequent atrophy.
It can be either primary (usually autosomal dominant) or secondary to a large number of underlying illnesses or metabolic disturbances.
On this page:
Terminology
There is confusion in the literature as to whether Fahr disease and Fahr syndrome are synonymous or not. Generally, the terms are used interchangeably, further divided into:
primary: equivalent to familial cerebral ferrocalcinosis or primary familial brain calcification (now the preferred term), with no underlying other cause, and
secondary: due to an underlying metabolic, infective or other cause
It has been argued, however, that the term Fahr disease should be reserved for – and, in fact, perhaps replaced by – primary familial brain calcification, whereas Fahr syndrome should be used only for secondary causes 6. This distinction has merit as it serves to clarify an otherwise confusing topic, and is also in line with similar usage in other conditions (e.g. Cushing disease vs syndrome, moyamoya disease vs syndrome).
The term idiopathic basal ganglia calcification is best avoided.
As the imaging features are similar, both Fahr disease (primary) and syndrome (secondary) are discussed in the remainder of this article.
Epidemiology
Calcification of basal ganglia is very common, and age dependent, with small amounts of calcification confined to the globus pallidus, considered a "normal" finding in the elderly.
Symptomatic onset for primary familial brain calcification (Fahr disease) tends to be between age 40 and 60 years 5. Incidence is unknown.
Clinical presentation
The clinical presentation is variable, with many individuals remaining asymptomatic. Severe forms can later present with parkinsonism, other movement disorders (e.g. chorea, dystonia), headache, seizures and epilepsy, psychosis, depression, and progressive cognitive impairment 6,9.
Pathology
Fahr disease is characterized by deposition of calcium in the walls of the capillaries and larger arteries and veins. Other compounds, such as mucopolysaccharides, and elements, including magnesium, zinc, aluminum, and iron, have also been found deposited in the vessels.
Calcification can be found in the globus pallidus, putamen, caudate, thalamus, cerebellum (especially in the dentate nucleus), corona radiata, and subcortical white matter.
Genetics
Fahr disease (primary familial brain calcification) is due to a variety of mutations, accounting for the majority (~60%) of diagnosed cases 5,7. These are inherited in an autosomal dominant pattern, although other mutations with a recessive mode of inheritance are likely to be present in the remaining, 'idiopathic' group.
Known mutations include 5,7,9,11:
-
phosphate metabolism
-
SLC20A2: encodes sodium-dependent phosphate transporter 2 (PiT2)
most commonly implicated mutation
XPR1: encodes for a retroviral receptor with phosphate export function
-
-
blood brain barrier integrity/pericyte maintenance
PDGFB: encodes for platelet-derived growth factor beta (PDGF-b)
PDGFRB: encodes for platelet-derived growth factor receptor beta (PDGFR-b)
-
recessive genes
MYORG: encodes for a protein in astrocytes
JAM2: encodes for a protein regulating endothelial cell adhesion
Primary familial brain calcification (Fahr disease)
In patients with supporting imaging findings (see radiographic features below) and in most cases some of the aforementioned clinical features, suggested diagnostic criteria for Fahr disease are 6:
genetic abnormality detected (see above): autosomal dominant or autosomal recessive inheritance with a positive family history
typically presents 40 to 60 years of age
typical distribution calcification with progression
causes of Fahr syndrome (secondary) are excluded (see below)
Fahr syndrome (secondary)
Fahr syndrome is typically diagnosed in younger individuals when a secondary cause is identified with appropriate intracranial imaging features. It should be noted that not all of the following causes result in typical patterns of calcification, so care must be taken not to overcall Fahr syndrome.
Causes include 5-7,10:
-
endocrinopathies
hypoparathyroidism (primary or secondary)
-
infections
congenital infections
Epstein-Barr virus (EBV)
-
other inherited disorders
radiation
chemotherapy
medications (e.g. bisphosphonates)
Radiographic features
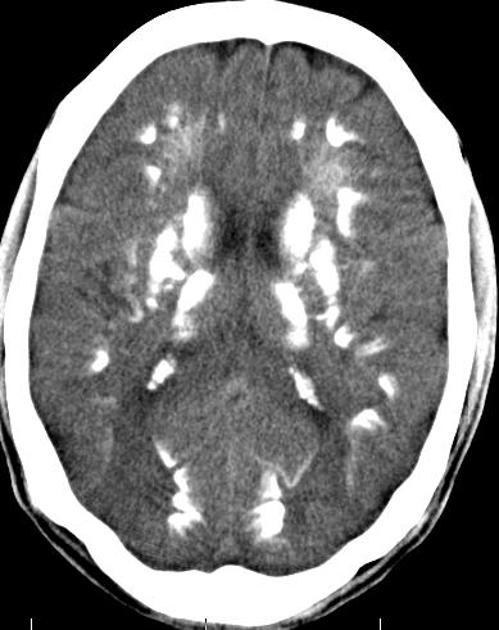
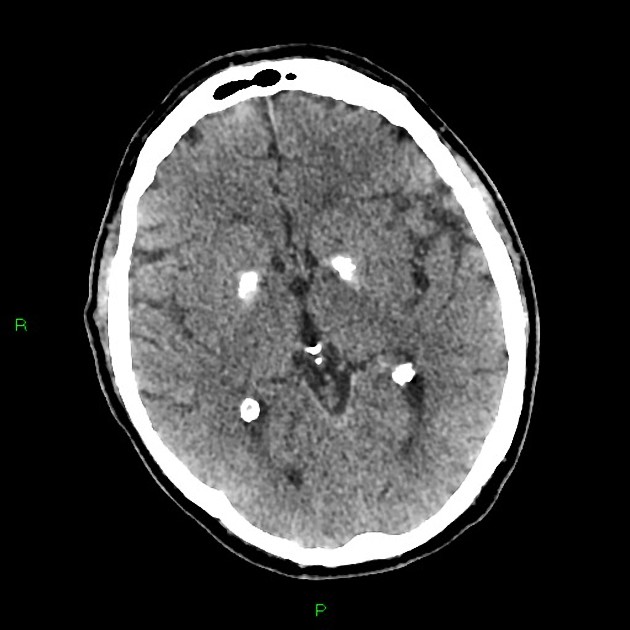
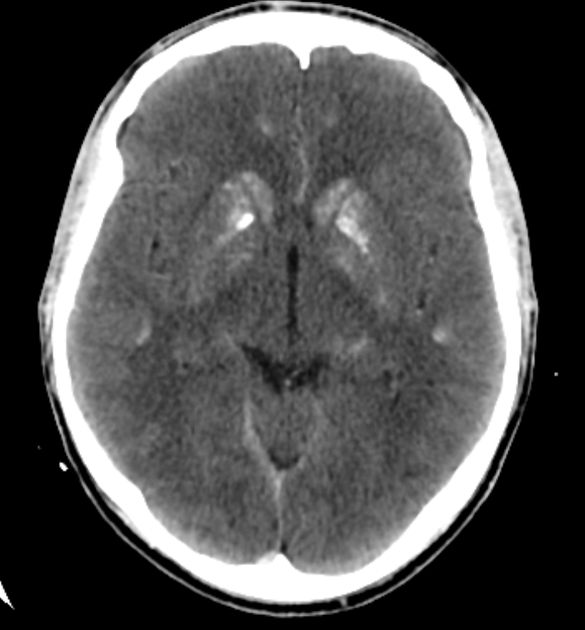
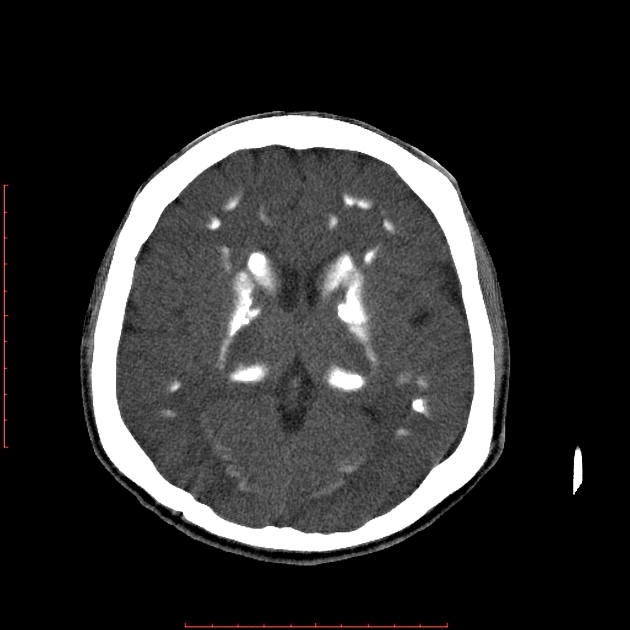
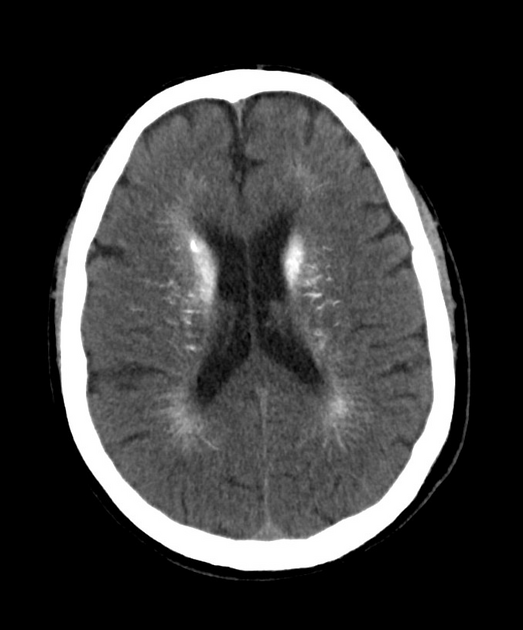
CT
Calcification is extensive and has a relatively typical distribution 3:
-
basal ganglia and thalami
symmetric involvement of caudate, lentiform nucleus, thalamus, and dentate nuclei
globus pallidus affected first
subcortical white matter
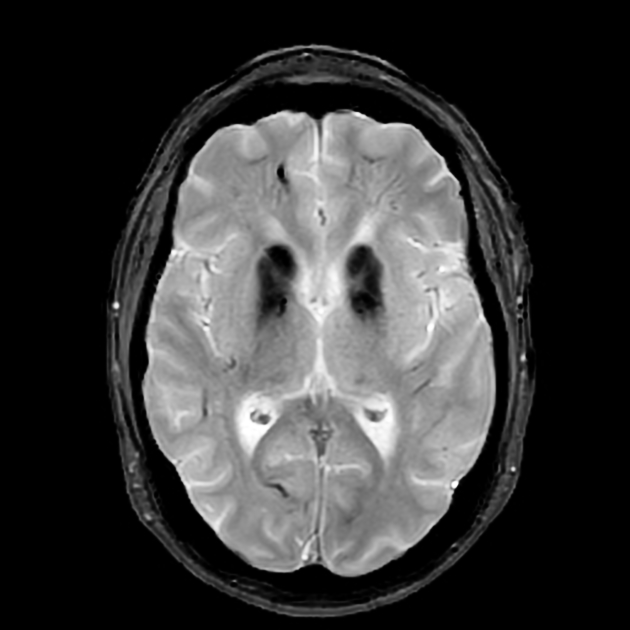
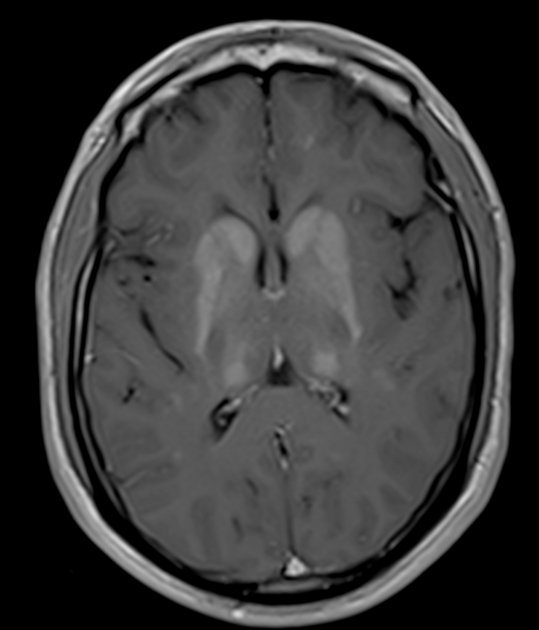
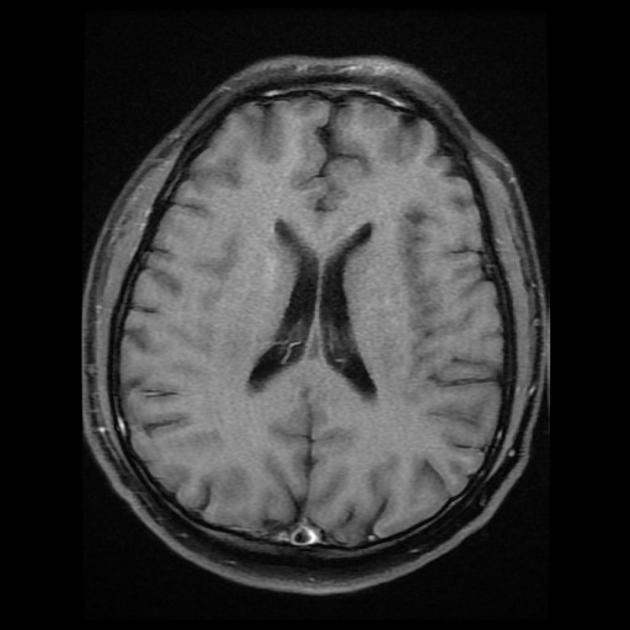
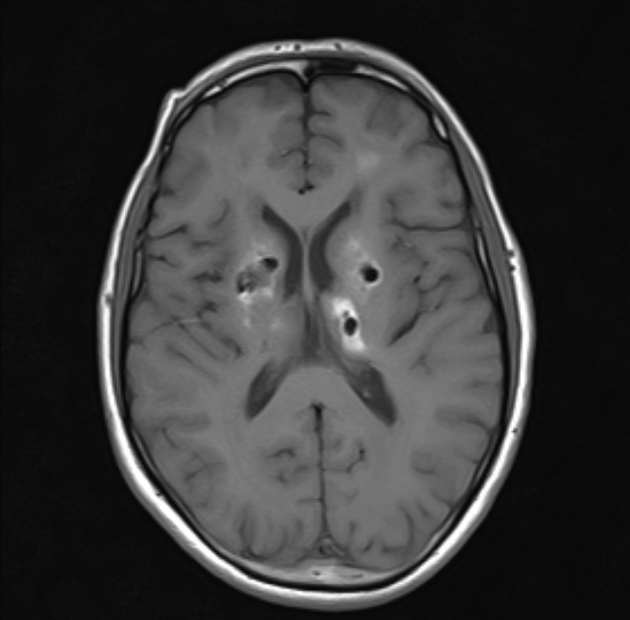
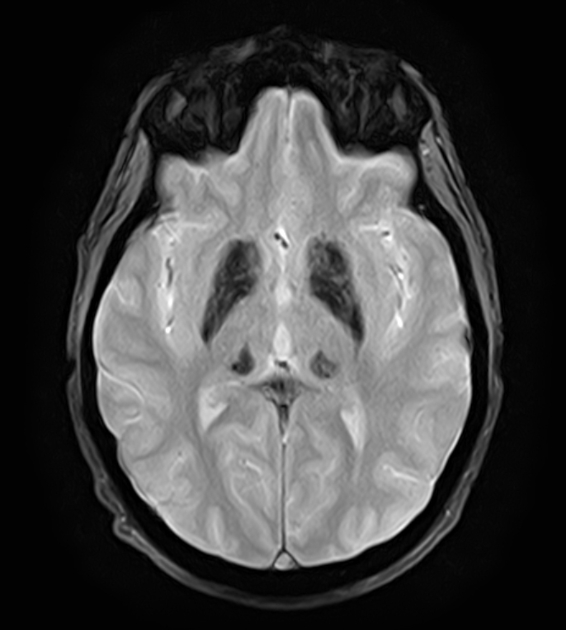
MRI
The MRI appearance varies depending on the degree of calcification and the stage of the disease and can be remarkably normal in appearance even when CT changes are profound, unless susceptibility weighted imaging is obtained 8.
T1: calcified areas are of increased signal; this is attributed to the surface area effect of the calcium crystals 4
-
T2
calcified areas demonstrate low to isointense signal
high signal regions may be identified in the basal ganglia, white matter and internal capsule which are not in the areas of calcification 4
SWI: signal loss 8
FDG-PET
May show decreased 18F-FDG uptake, particularly in the basal ganglia.
Treatment and prognosis
Primary familial brain calcification (Fahr disease) progresses steadily, and there is no known cure or specific treatment, thus management is supportive depending on the clinical manifestations. There is a correlation between the extent of brain calcification and the symptom severity 11.
In Fahr syndrome, treatment should be aimed at the underlying secondary condition.
History and etymology
It was first noted in 1930 by Karl Theodor Fahr (1877-1945), a German pathologist.
Differential diagnosis
The differential for primary familial brain calcification (Fahr disease) is that of Fahr syndrome (see above). Also, refer to the article basal ganglia calcification.















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.