Esophageal stricture refers to any persistent intrinsic narrowing of the esophagus.
On this page:
Terminology
The term peptic stricture refers specifically to those benign esophageal strictures caused by chronic acid reflux, although some - incorrectly - use it more loosely to refer to any benign esophageal narrowing. The qualifying word "esophageal" is usually omitted as strictures due to acid elsewhere in the gut are very rare 5,6.
Epidemiology
Associations
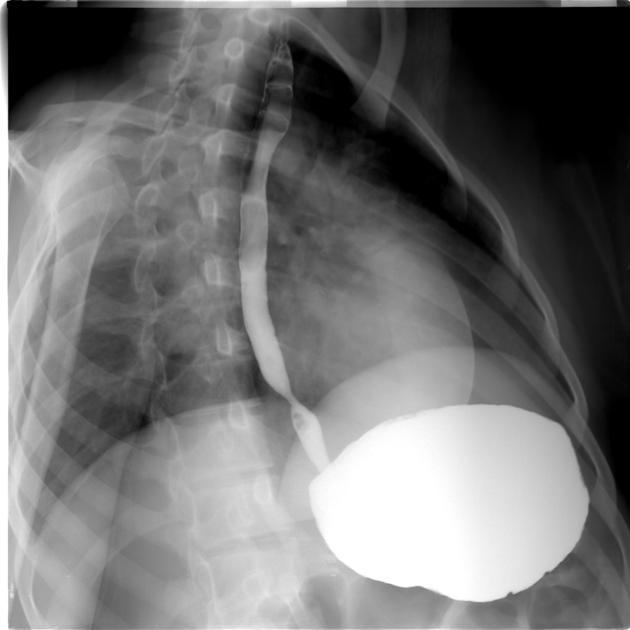
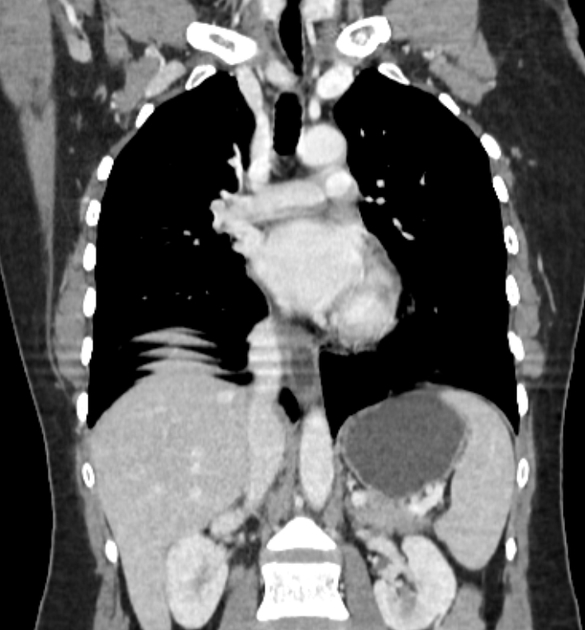
Esophageal strictures are often associated with a hiatal hernia.
Pathology
Etiology
The most common causes are fibrosis induced by inflammatory and neoplastic processes. Because radiographic findings are not reliable in differentiating benign from malignant strictures, all should be evaluated endoscopically.
Upper and middle esophageal strictures
These most commonly result from:
mediastinal radiation
-
skin diseases associated with mucosal ulceration, such as
pemphigoid
erythema multiforme
epidermolysis bullosa dystrophica
Distal esophageal strictures
These are typically caused by gastro-esophageal reflux disease (GERD), either as a separate entity or in the setting of:
prolonged nasogastric intubation
Zollinger-Ellison syndrome: high acidity reflux
-
post partial or total gastrectomy: alkaline reflux
performing the Roux-en-Y procedure may avoid this, by diverting the pancreatic secretions and bile away from the gastric remnant
As stated earlier if reflux disease has been a significant contributor to the development of the stricture then using the term "peptic stricture" is appropriate.
Radiographic features
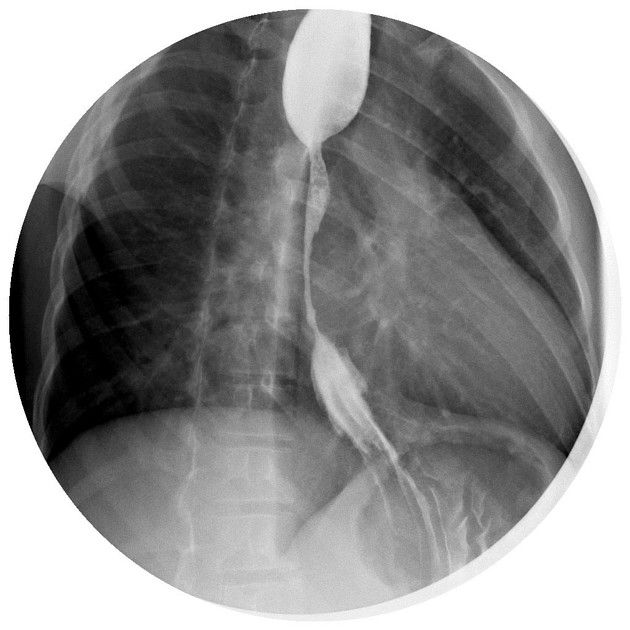
Benign strictures characteristically:
smoothly tapering
typically concentric narrowing, but may affect only one side of the esophagus (asymmetric wall rigidity)
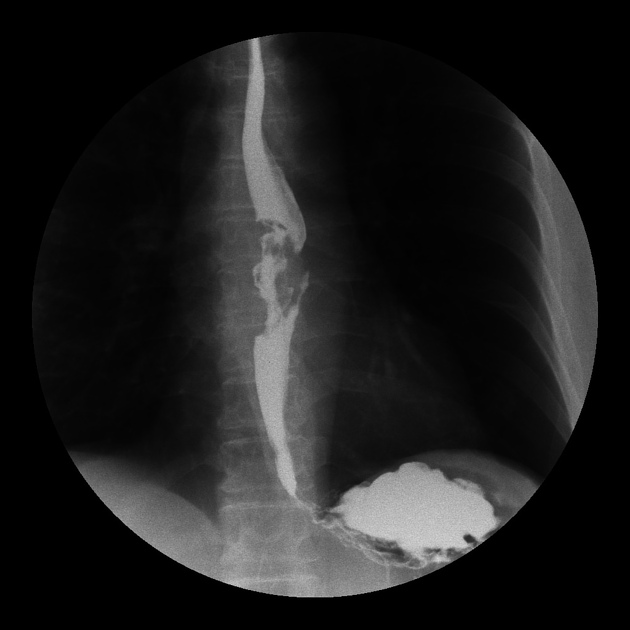
Malignant strictures are characteristically:
abrupt
asymmetric
eccentric with irregular, nodular mucosa
Tapered margins may occur with malignant lesions because of the ease of submucosal spread of a tumor.
Treatment and prognosis
The risk of Barrett esophagus in stricture is 20-40% and strictures should be evaluated endoscopically.
Benign esophageal strictures are typically treated with dilation, which provides symptomatic relief; however, recurrent strictures do occur. Complex strictures (length >2 cm, tortuous) are more likely to be recurrent. Treatment of malignant strictures involves treating the underlying cause. In palliative strictures, stent placement and brachytherapy play a role 4.



















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.