Paget disease of the bone is a common, chronic metabolic bone disorder characterized by excessive abnormal bone remodeling. The classically described radiological appearances are expanded bone with a coarsened trabecular pattern. The pelvis, spine, skull, and proximal long bones are most frequently affected.
On this page:
Terminology
Paget disease of the bone is the most common formal name for the condition 24. Synonymous terms such as osteitis deformans, which was the name given by Paget himself to the disease, are of historical interest only.
Epidemiology
Paget disease of the bone is relatively common and can affect up to 4% of individuals over 40 years and up to 11% over the age of 80 years 1. There may be a slight male predilection for Paget disease. Incidence may be considerably higher in the United Kingdom than in other countries 8. It is also common in Australia, New Zealand, Western Europe, and the United States.
Over the last two to three decades a dramatic fall in incidence and severity of Paget disease has been observed 28, 37.
Clinical presentation
The majority (approximately three-quarters) of patients are asymptomatic at the time of diagnosis, the diagnosis being an incidental finding on imaging 23. Presenting symptoms include:
localized pain and tenderness (most common symptom 24)
increased focal temperature due to bony hypervascularity (not fever)
increased bone size: historically, changing hat size was a giveaway
decreased range of motion
signs and symptoms relating to complications (see below)
Polyostotic disease is more prevalent than monostotic type 1. The most frequent sites of involvement are:
spine
pelvis (often asymmetric)
skull
proximal long bones
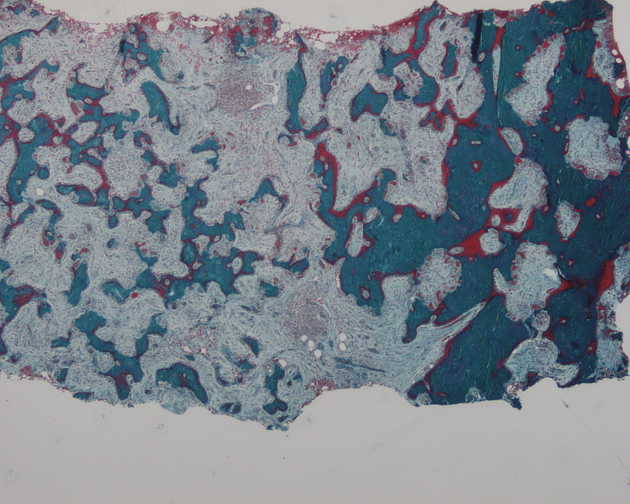
Pathology
The etiology is not entirely established, but it is a disease of osteoclasts. Environmental exposures, such as viral infection (paramyxovirus) 6, 28 in association with a genetic susceptibility (SQSTM1) 29 has been postulated.
There are three classically described stages, which are part of a continuous spectrum 22:
early destructive stage (incipient active, lytic): predominated by osteoclastic activity
intermediate stage (active, mixed): osteoblastic as well as osteoclastic activity
late stage (inactive, sclerotic/blastic)
These stages correlate well with the imaging findings.
Involvement of multiple bones (polyostotic) is more common than single or monostotic disease. If untreated, active lesions are estimated to progress at a rate of 1–2 cm per year 28, 34.
Genetics
Genetic factors are linked to the pathogenesis of Paget disease.
The most common mutation affects the sequestosome 1 gene (SQSTM1) and has been described in approximately 25%–40% of familial cases and in up to 10%–15% sporadic cases 29, 30, 31. Disease develops at an earlier age and is more severe in these individuals 32.
The decline in prevalence and incomplete penetrance of the disease among family members suggests that a gene-environment interaction may play a role in the pathophysiology 28, 33.
Markers
elevated serum alkaline phosphatase
normal calcium and phosphorus levels
increased urine hydroxyproline
Radiographic features
Signs
There are many Paget disease-related signs, listed here and described in the modality-specific sections below 25:
* pathognomonic signs 25
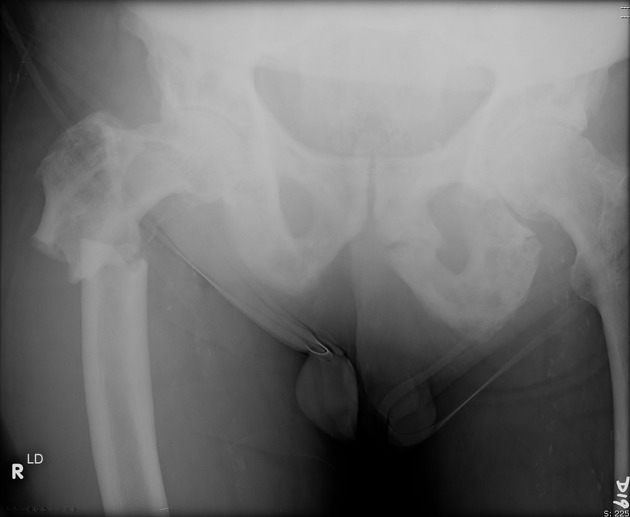
Plain radiograph/CT
Plain radiographic and CT features will depend upon the phase of the disease.
The early phase features osteolytic (lucent) regions which are later followed by coarsened trabeculae and bony enlargement. Sclerotic changes occur much later in the disease process.
Additional destructive features may become apparent if malignant transformation occurs.
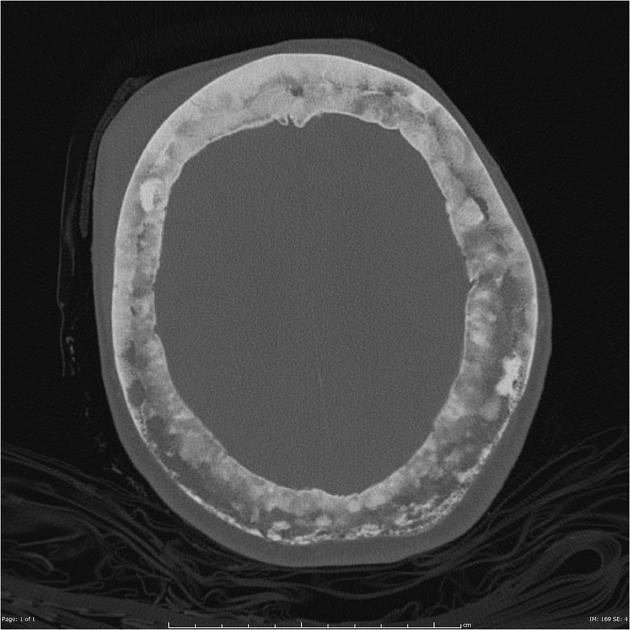
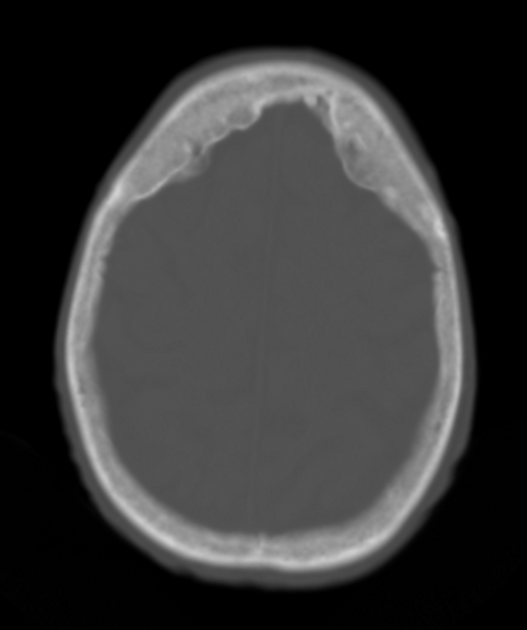
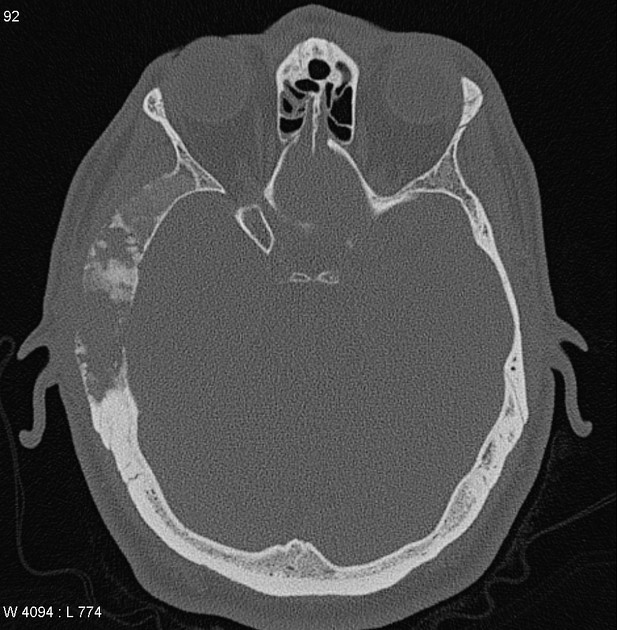
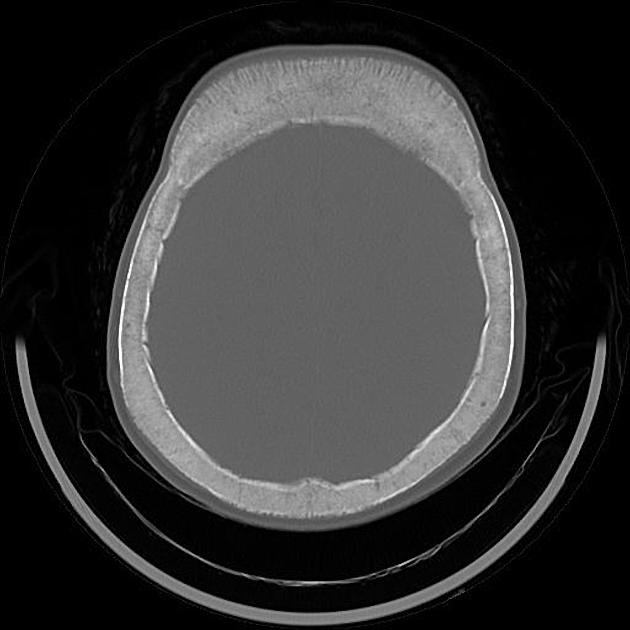
Skull
osteoporosis circumscripta: large, well-defined lytic lesions involving the inner aspect of the outer table of the skull (stage one) with a preserved inner table.
cotton wool appearance: mixed lytic and sclerotic lesions of the skull.
diploic widening: both inner and outer calvarial tables are involved, with the former usually more extensively affected
Tam o' Shanter sign: platybasia and basilar invagination with the appearance of the skull falling over the facial bones, like a Tam o' Shanter hat; this is said to be a pathognomonic appearance 25
Spine
-
picture frame sign: Paget disease of the spine frequently manifests with cortical thickening and sclerosis encasing the vertebral margins, which gives rise to this appearance on radiographs in mixed-phase disease
this is said to be a pathognomonic appearance 25
squaring of vertebrae: on lateral radiographs, flattening of the normal concavity of the anterior margin of the vertebral body also adds to the rectangular appearance
vertical trabecular thickening: coarser than the more delicate pattern seen in intraosseous hemangiomas with which it may be confused
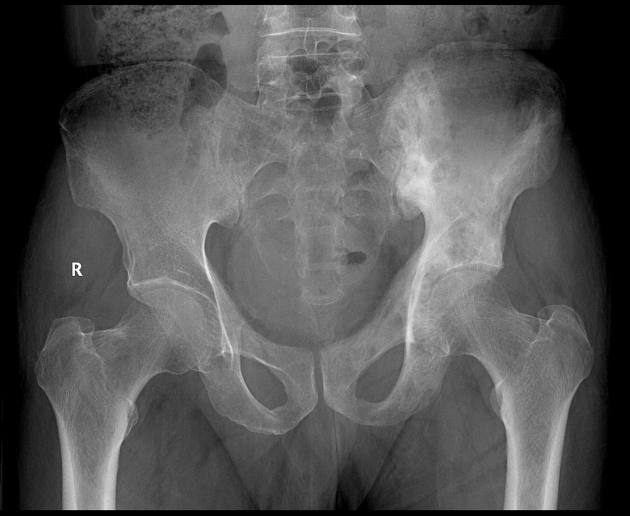
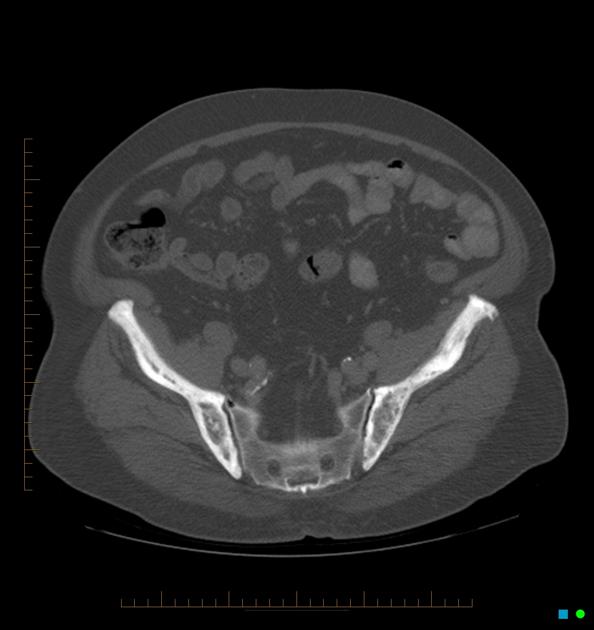
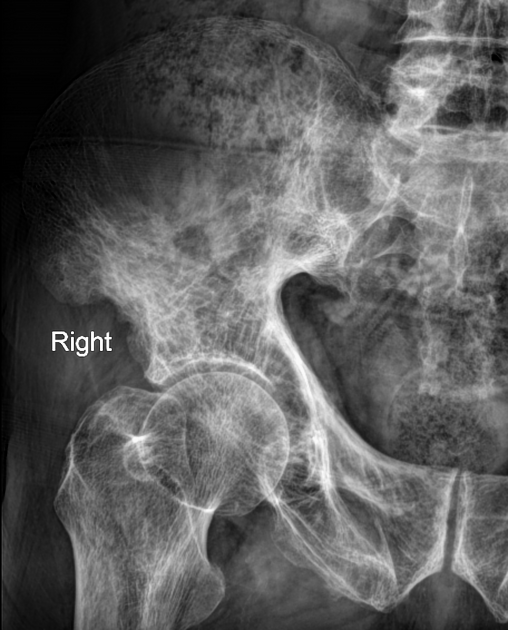
Pelvis
cortical thickening and sclerosis of the iliopectineal and ischiopubic lines results in the pelvic brim sign and leads to obliteration of Köhler's teardrop
enlargement of the pubic rami and ischium
These findings are often asymmetric, and for some reason, are more commonly seen on the right side.
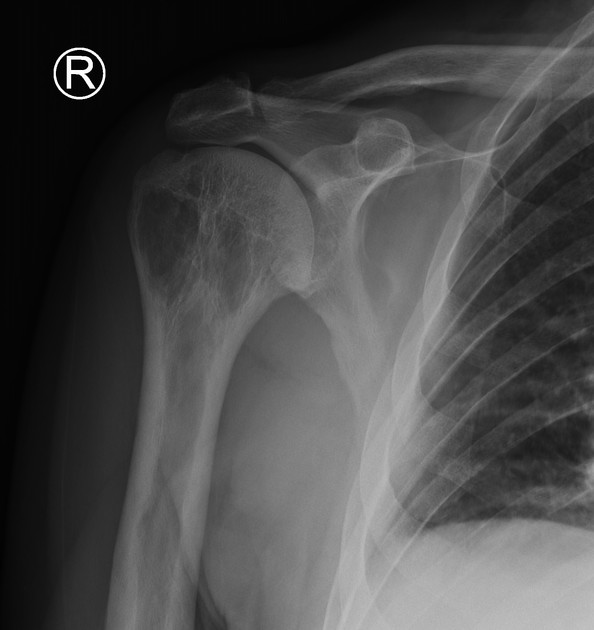
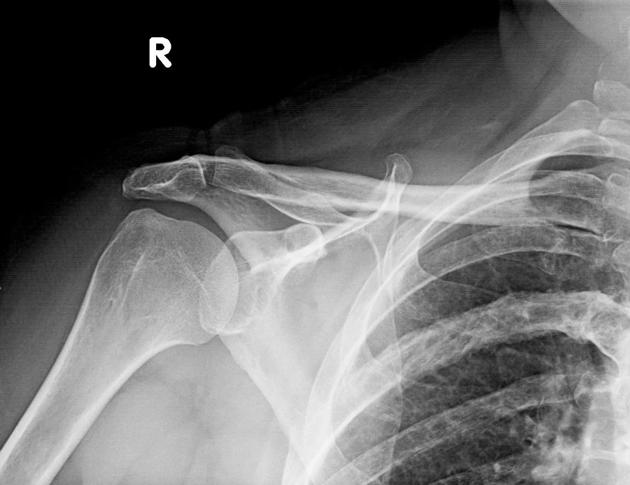
Long bones
-
blade of grass or candle flame sign: begins as a subchondral area of lucency with advancing tip of V-shaped osteolysis, extending towards the diaphysis
in rare cases, the disease is isolated to the diaphysis, most commonly in the tibia, rather than subchondral bone, which can cause diagnostic confusion.
lateral curvature (bowing) of the femur
anterior curvature of the tibia
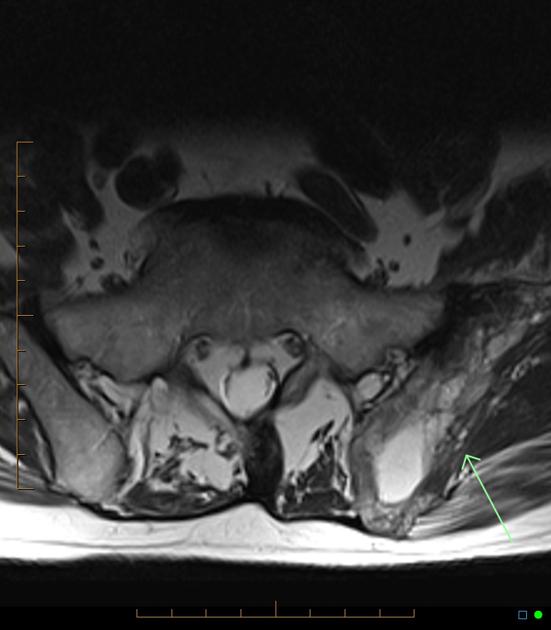
MRI
The overall signal characteristics are variable, likely reflecting the natural course of the disease process in different phases.
Several major patterns of involvement have been described 8,16:
dominant signal intensity in Pagetic bone similar to that of fat; most common pattern and probably corresponds to longstanding disease
relatively low T1 and high T2 signal alteration (also referred as a “speckled” appearance); second most common pattern: probably corresponds to granulation tissue, hypervascularity, and edema seen in early mixed active disease
low signal intensity on both T1 and T2 images; suggesting the presence of compact bone or fibrous tissue; least common pattern: seen in late sclerotic stage
Fatty marrow signal is usually preserved in all sequences unless there is a complication 10.
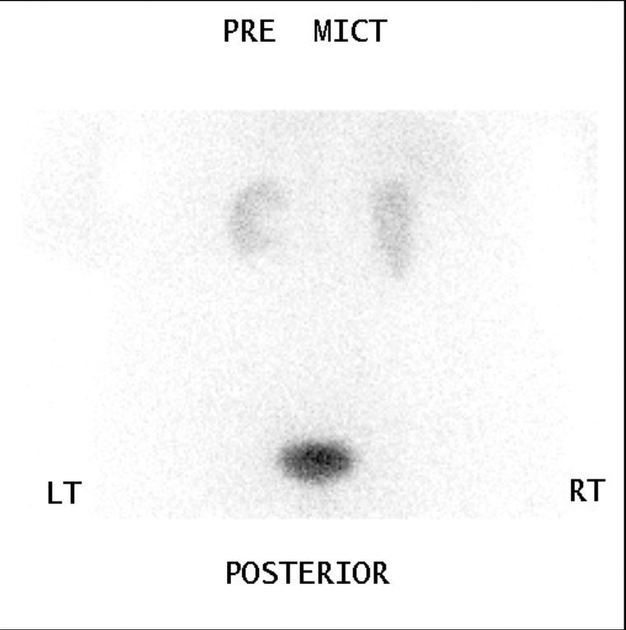
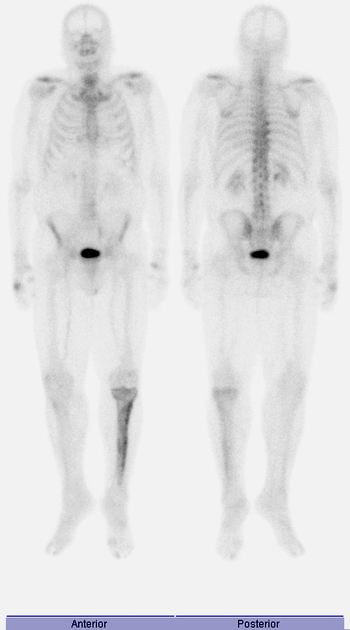
Bone scintigraphy
Tc-99m-MDP is highly sensitive but not specific. It is useful to define the overall extent and distribution of disease.
marked increased uptake in all phases of the disease, although in the burnt-out sclerotic quiescent phase uptake may be normal 1
Mickey Mouse sign: uptake in the vertebral body and posterior elements forming an inverted triangular pattern on posterior planar imaging resembling the Mickey Mouse silhouette 17,18; also known as the "heart" or "clover" sign 19 and "T" or "champagne glass" sign 20
Lincoln sign: diffuse mandibular uptake forming a bearded appearance 21
Treatment and prognosis
Treatment with bisphosphonates (e.g. IV zoledronic acid) has been shown to prevent or slow disease progression 32, reduce complications 34 and induce life long remission 28, 35, 37.
Bisphosphonate therapy aims to restore normal lamellar bone in place of the woven bone characteristic of Paget disease, reduce the bone turnover, promote healing of osteolytic lesions and improve bone pain 36.
Analgesics and non-hormonal anti-inflammatory drugs are also prescribed for pain management.
The prognosis and evolution of pagetic lesions was established by studies from the pre-bisphosphonate era. If left untreated, active lytic lesions were estimated to progress at a rate of 1–2 cm per year 28, 34. Associated complications became more likely as the disease progressed.
Some propose bisphosphonate treatment prior to surgery on a pagetic bone 34, 37.
Guidelines
International opinion differs regarding which patient cohort to treat.
Given the long-term efficacy and safety of current therapeutic regimens, and disease progression in untreated patients, some guidelines 34, 37 suggest that all patients, including asymptomatic ones, should receive treatment.
Others suggest treating only those with active disease (based on biochemical markers of bone remodeling), specific symptoms (i.e., bone pain) or asymptomatic cases with a greater risk of complications (e.g., involvement of weight bearing bones or immobilization) 36.
Complications
osseous weakening resulting in deformity and pathological fractures
increased risk of osteoarthritis 12
-
hearing loss
-
compression of the vestibulocochlear nerve in the internal auditory canal 14
loss of bone mineral density of the cochlear capsule 15
-
fixation of the middle ear ossicles 14
-
-
neural compression
cranial nerve paresis may occur
basilar invagination may occur in advanced cases with hydrocephalus or brainstem compression
secondary development of tumors (e.g. osteosarcoma: ~1% of cases, more common in polyostotic form, which is often highly resistant to treatment; giant cell tumor in the skull)
-
high output congestive cardiac failure (extremely rare 24)
when bone involvement >15%
rapid bone formation/resorption can lead to left-to-right shunting and decreased peripheral resistance 13
hyperparathyroidism (~10%)
post-operative loosening of a prosthesis 36
History and etymology
Sir James Paget (1814-1899) 27 first described it in 1877 in a case report of a patient he had observed over some twenty years 5.
The condition was initially named by Paget "osteitis deformans", implying an inflammatory etiology. The term "osteodystrophica deformans" is now preferred.
Differential diagnosis
For skull lesions consider ref:
hyperostosis frontalis interna: thickening of the internal table of the frontal bone
-
different age group (typically younger)
fibrous dysplasia usually affects the outer table more prominently
For spinal lesions consider 26:
vertebral hemangioma: usually finer trabecular markings in hemangioma than Paget related changes
Modic type 2 endplate change
Consider other fat-containing lesions 26:
Rare, familial forms of Paget disease of the bone have also been described 27:


























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.