Parathyroid adenomas are benign tumors of the parathyroid glands and are the most common cause of primary hyperparathyroidism.
On this page:
Epidemiology
Associations
There is an association with multiple endocrine neoplasia types I (MEN1) and IV (MEN4).
Clinical presentation
Patients typically present with primary hyperparathyroidism: elevated serum calcium levels and elevated serum parathyroid hormone levels. This results in multisystem effects including osteoporosis, renal calculi, constipation, peptic ulcers, mental changes, fatigue, and depression.
Rarely, parathyroid adenomas present with spontaneous hemorrhage, which can be large and potentially narrow the airway 21.
Pathology
They are usually oval or bean-shaped, but larger adenomas can be multilobulated. The vast majority (up to 87% 2) of adenomas occur as solitary lesions.
Location
The majority of parathyroid adenomas are juxtathyroid and located immediately posterior or inferior to the thyroid gland. Superior gland parathyroid adenomas may lie posteriorly in the tracheo-esophageal groove, paraesophageal location, or even as inferior as the mediastinum 12.
Up to 5% of parathyroid adenomas can occur in ectopic locations. Common ectopic locations include 1,12:
mediastinum
retropharyngeal
carotid sheath
intrathyroidal
Variants
Markers
Parathyroid hormone levels are usually elevated (normal range 1.6-6.9 pmol/L or 10-55 pg/mL). Anticipated size of parathyroid adenoma is usually proportionate to the elevated parathyroid hormone level ref.
Radiographic features
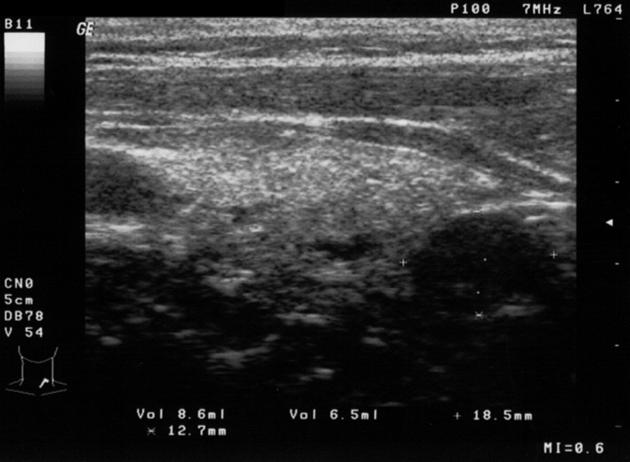
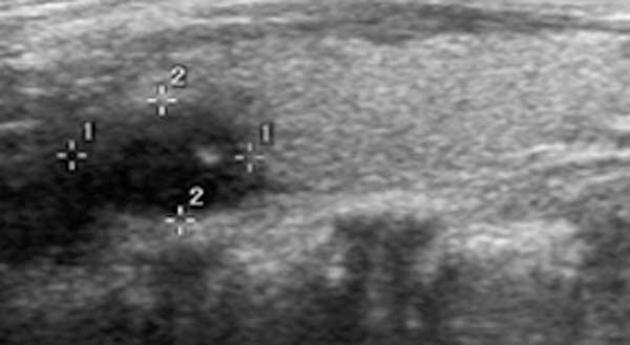
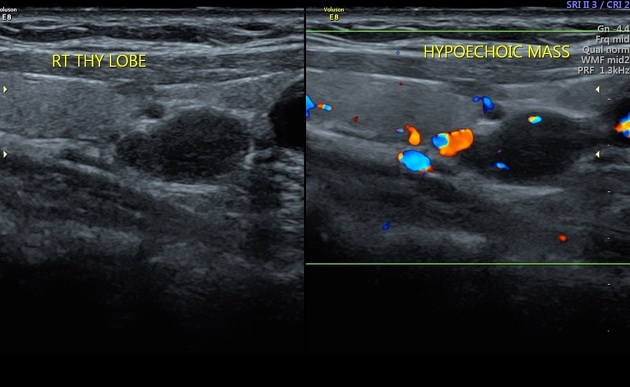
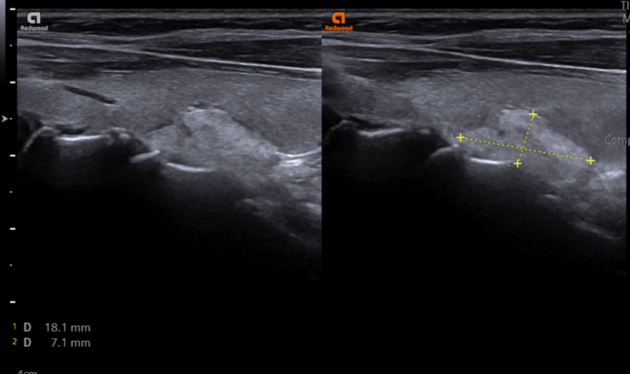
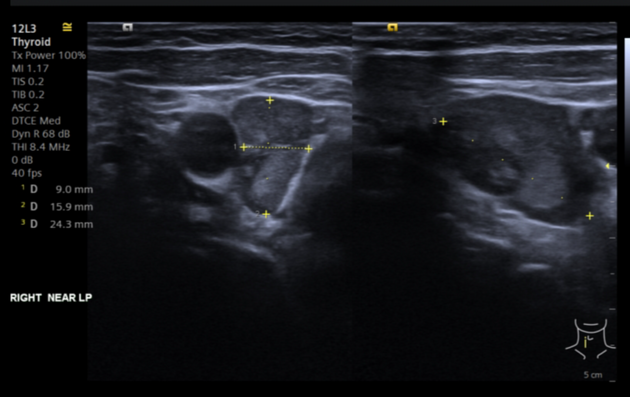
Ultrasound
Ultrasound is one of the most commonly used initial imaging modalities.
Greyscale
most nodules need to be >1 cm to be confidently seen on ultrasound ref
parathyroid adenomas tend to be homogeneously hypoechoic compared to the overlying thyroid gland ref
an echogenic thyroid capsule separating the thyroid from the parathyroid may be seen: some of the nodule may appear as fairly well-defined with no appreciable capsule ref
-
atypical features include 27
cystic degeneration: can range from minimal cystic change to mostly cystic (>50%) or cystic (~5%)
calcification (~1.5%)
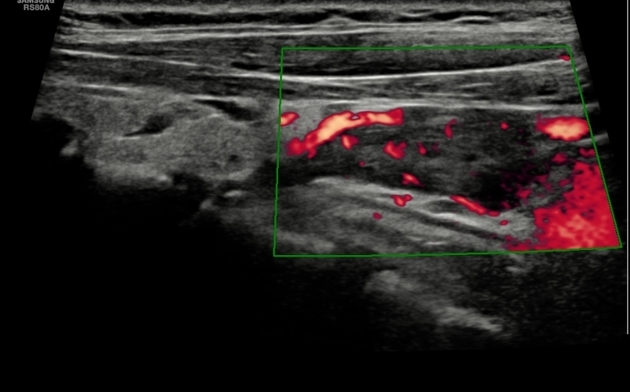
Doppler
Color Doppler signal can be seen in ~90% (range 85-97%) 29-31 of parathyroid adenomas in primary hyperparathyroidism, with a lower rate (~65%) in secondary hyperparathyroidism 29. A variable pattern of color Doppler signal can be seen with combined patterns sometimes present 33:
-
variable central/internal color Doppler signal that can indicate small to abundant blood flow 6,31-33
low resistive index, which decreases as serum PTH increase 6,32
-
polar/feeding vessel sign
extrathyroidal arterial feeder (usually a branch of the inferior thyroidal artery) at one of the parathyroid poles 1,6
present in ~80% (range 70-97.6%) of parathyroid adenomas 31,33 with smaller parathyroid adenomas less likely to have this sign 31
can help differentiate from lymph nodes (central/hilar vascularity) and thyroid nodules (vascularity not seen) 32,33
arc or rim of color Doppler signal 29,30
no color Doppler signal 31
Usually, parathyroid adenomas appear more vascularized than thyroid parenchyma 33. The overlying ipsilateral thyroid gland commonly (~85%) shows asymmetric hypervascularity 32.
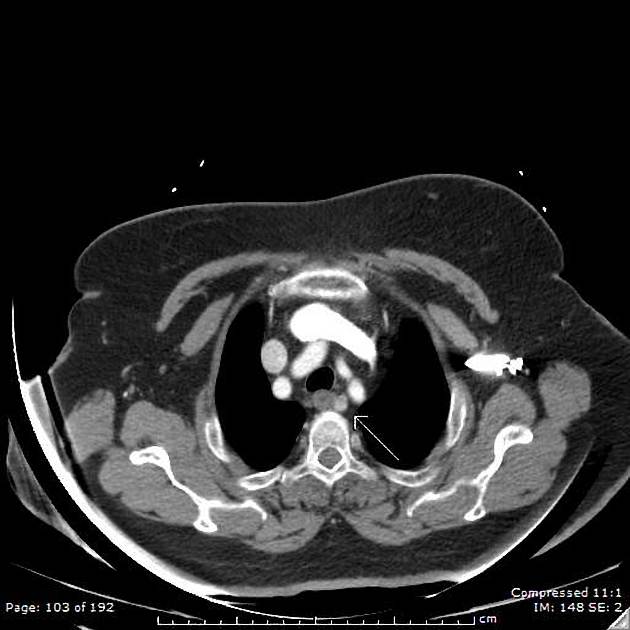
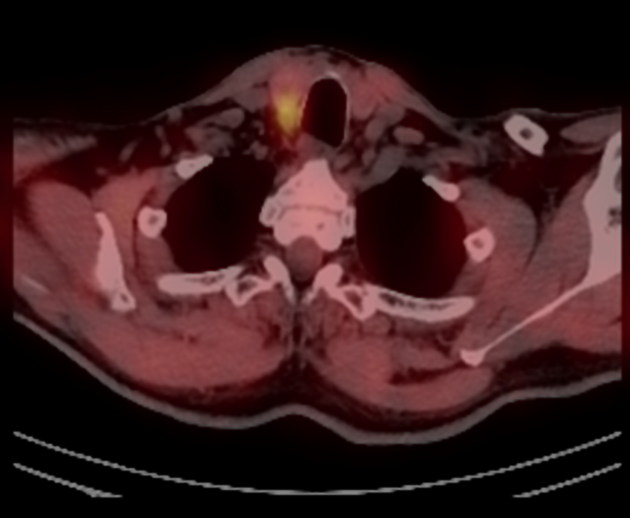
CT
CT can detect suspected ectopic glands (often mediastinal), such as in the case of failed parathyroidectomy 6. 4D parathyroid CT is a valuable modality in the era of minimally-invasive parathyroidectomy to precisely localize adenomas preoperatively. 4D CT has been shown to be more sensitive than sonography and scintigraphy for preoperative localization of parathyroid adenomas 13,15.
See the separate article on 4D parathyroid CT for an approach to interpretation and the imaging appearance of parathyroid lesions. The classic pattern of parathyroid adenomas, with intense enhancement on arterial phase, washout of contrast on delayed phase, and low attenuation on non-contrast imaging 12, is present in only a minority of cases 19.
Several morphologic features can support the diagnosis of an abnormal parathyroid gland 14:
-
polar vessel sign
an enlarged feeding artery or draining vein leading to the end of a hypervascular parathyroid
most neuroendocrine tumors are hypervascular
larger lesion: single adenomas tend to be larger than multiglandular disease and size increases diagnostic confidence
on non-contrast imaging parathyroid adenomas are less dense than the thyroid as they are iodine-deplete
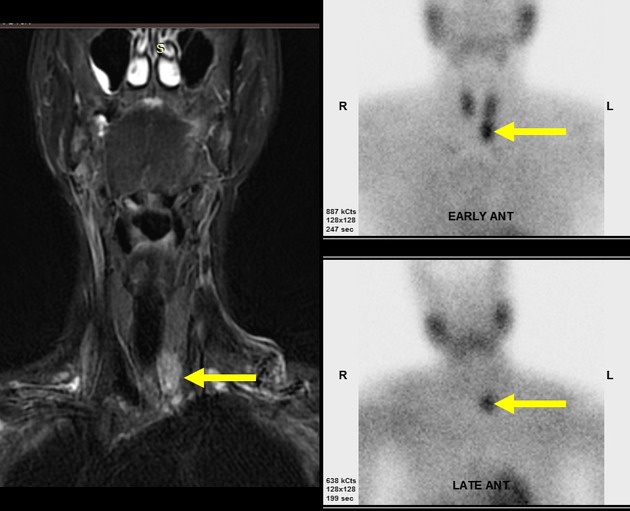
MRI
MRI is infrequently utilized in initial workup because of lower spatial resolution and artifacts. Adenomas can show variable signal intensity on MRI. Reported signal characteristics include:
-
T1
typically intermediate to low signal
subacute hemorrhage can cause high signal intensity 6
fibrosis or old hemorrhage can cause low signal intensity 6
-
T2
typically hyperintense
subacute hemorrhage can cause high signal intensity 6
fibrosis or old hemorrhage can cause low signal intensity 6
Since most lesions demonstrate high T2 signal intensity, the addition of contrast for MRI does not significantly increase detection.
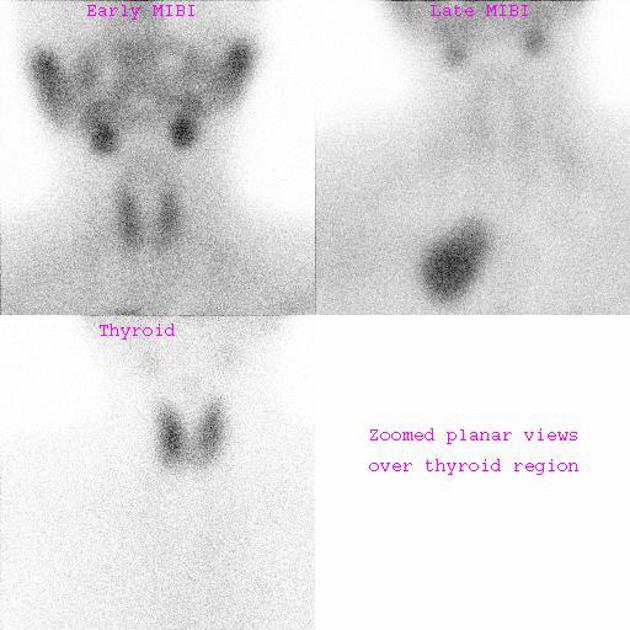
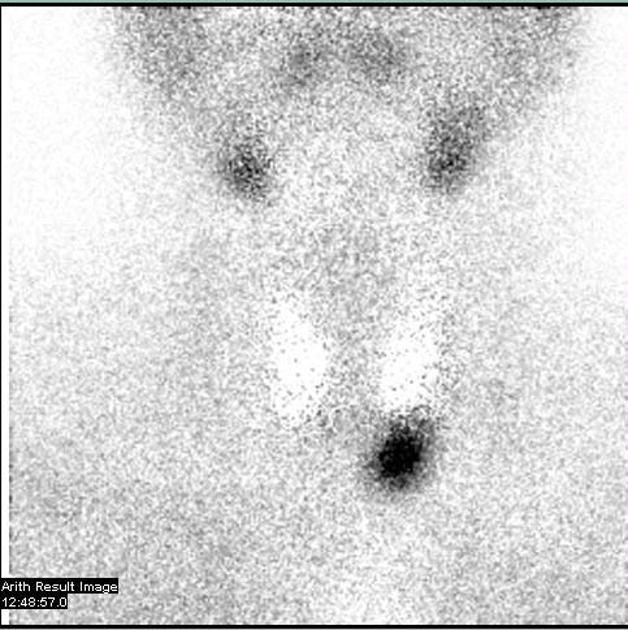
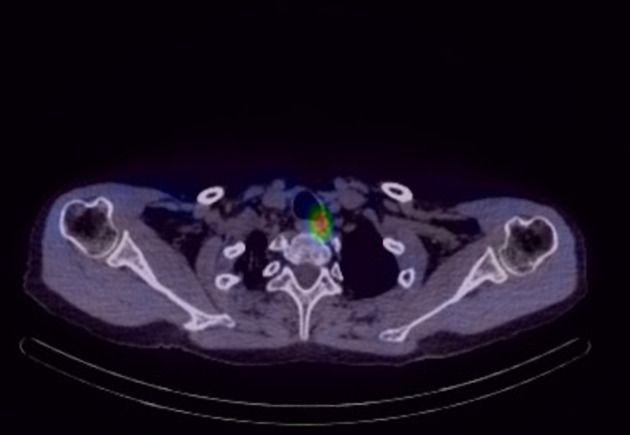
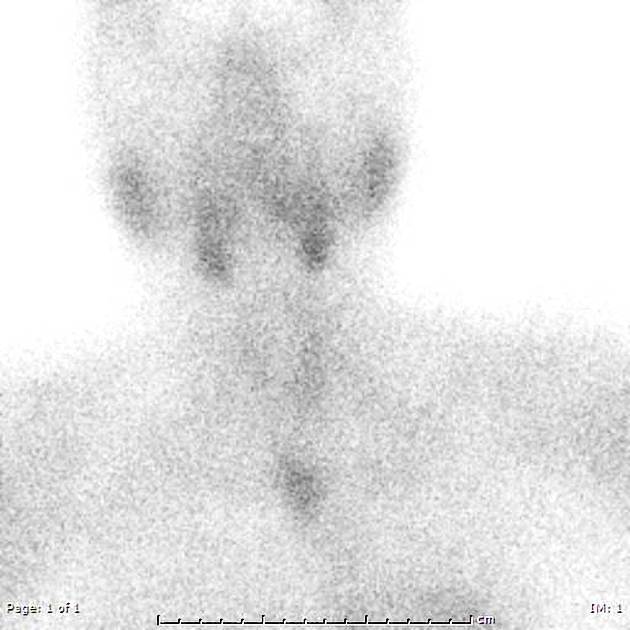
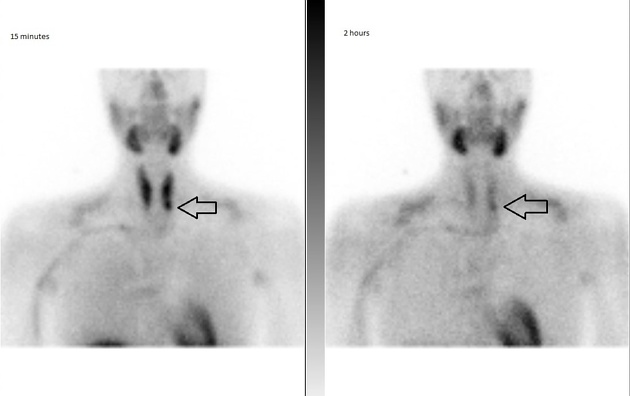
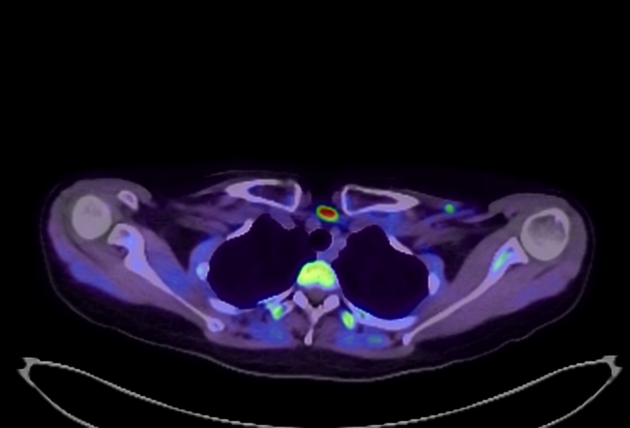
Nuclear medicine
SPECT and planar scintigraphy using Tc-99m sestamibi (most common) or Tc-99m tetrofosmin can help localize parathyroid lesions, which show high radiotracer uptake and persistent activity on delayed (2 hour) images 6. Fusion SPECT-CT can further aid anatomic localization.
18F-fluorocholine PET-CT is an emerging modality (c. 2021) with reported localization rates similar to sestamibi 18,20.
Treatment and prognosis
Surgical treatment is reserved for symptomatic patients. Surgery is successful in treating primary hyperparathyroidism caused by parathyroid adenomas in 95-98% of cases 17. Ethanol ablation is an additional alternative treatment 28.
Differential diagnosis
For a non-ectopic adenoma on ultrasound, consider:
eccentric thyroid nodule
blood vessel














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.