Pneumomediastinum is the presence of extraluminal gas within the mediastinum. Gas may originate from the lungs, trachea, central bronchi, esophagus, and peritoneal cavity and track from the mediastinum to the neck or abdomen. Tension pneumomediastinum is potentially fatal.
On this page:
Terminology
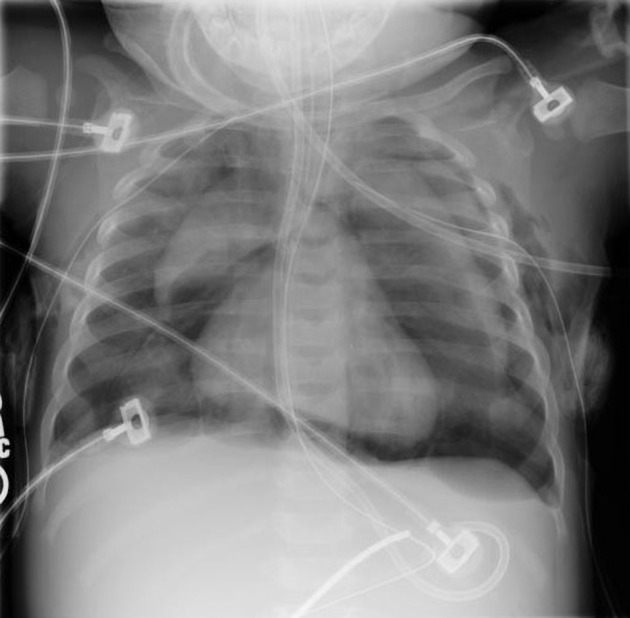
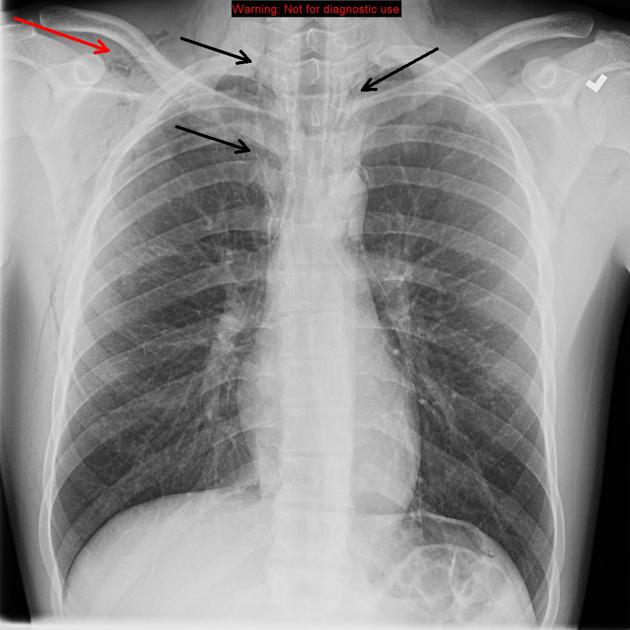
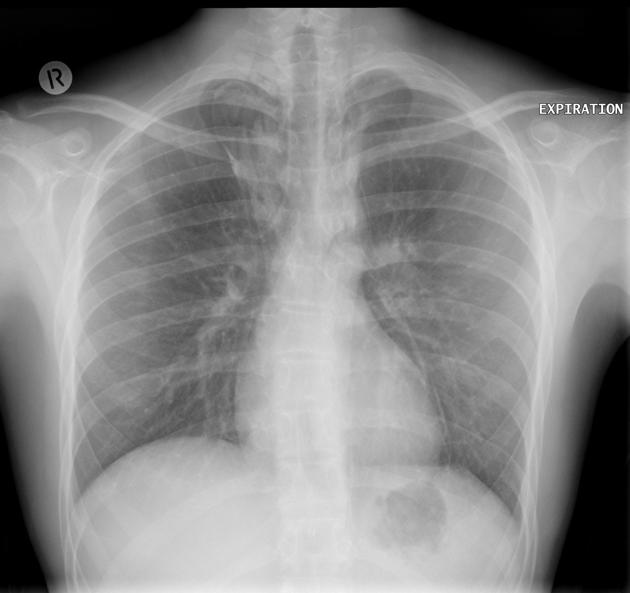
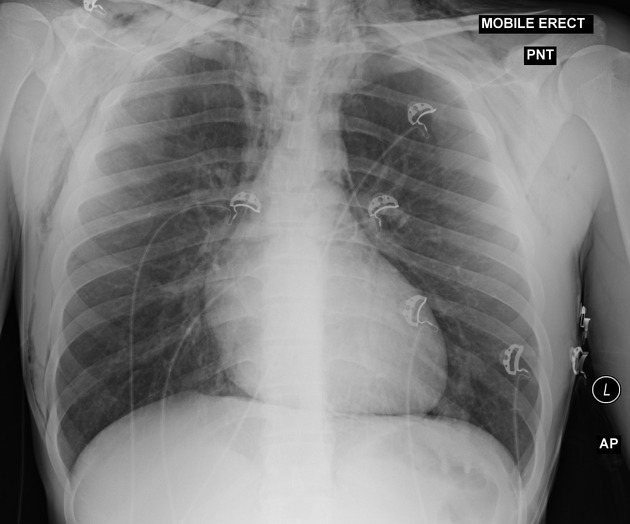
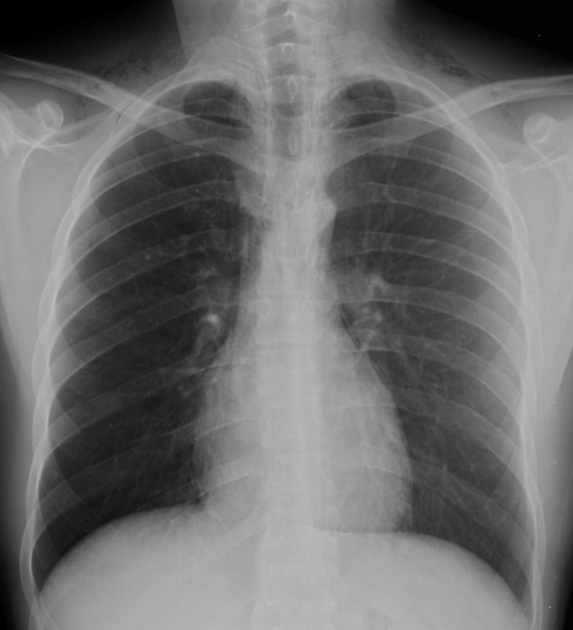
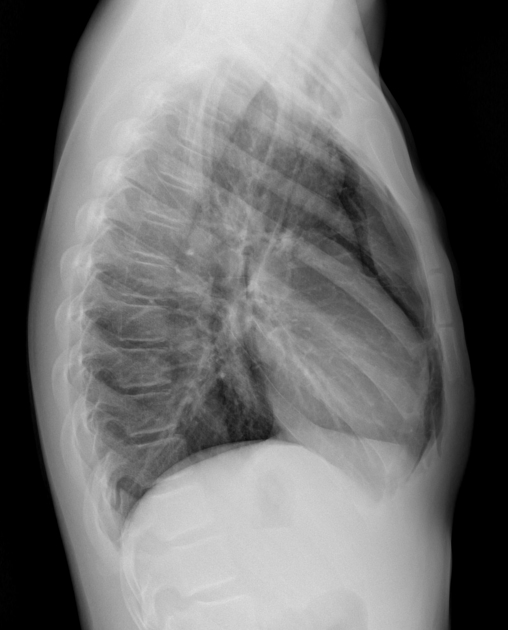
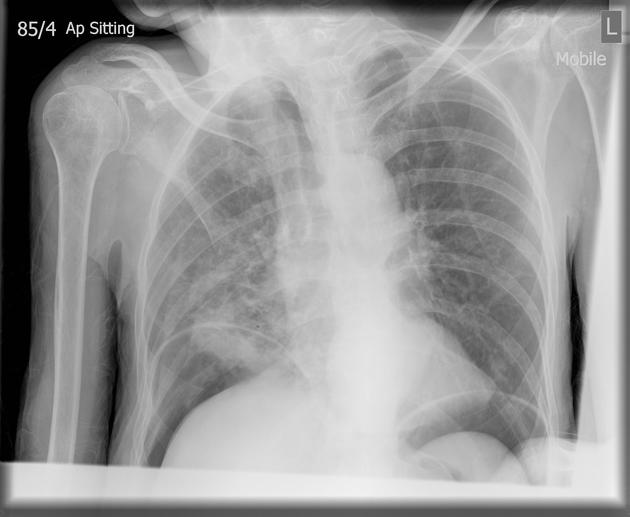
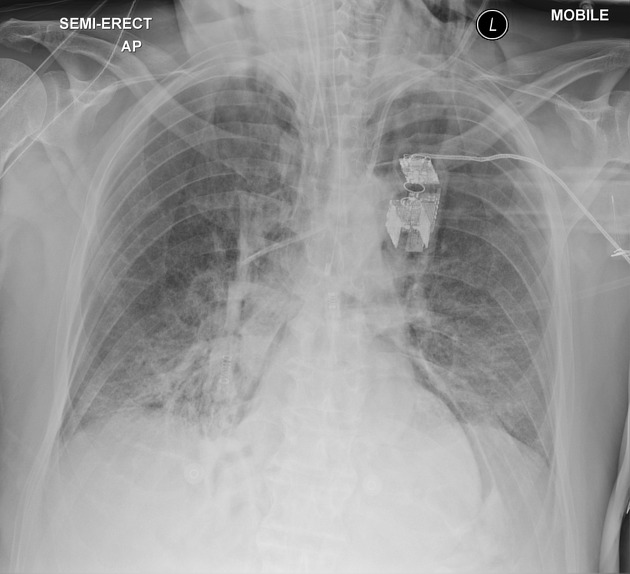
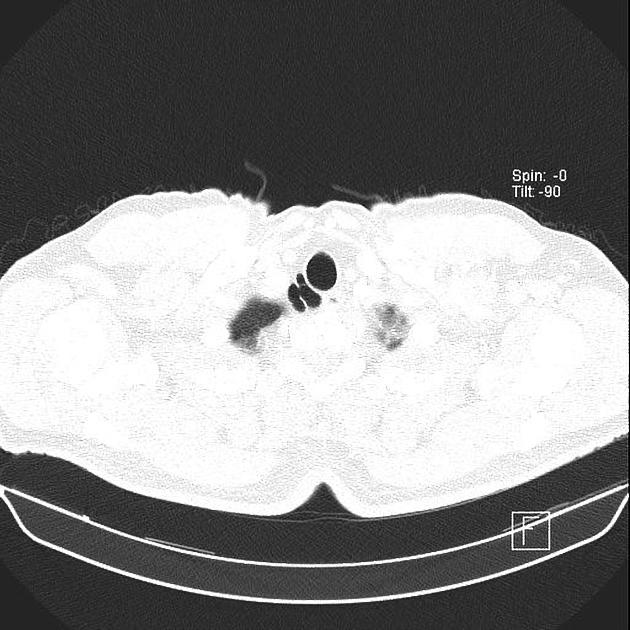
In the setting of trauma, if pneumomediastinum is visible on chest x-ray it is termed overt pneumomediastinum whereas if it is only visible on CT then it is termed occult pneumomediastinum 8.
Pathology
Etiology
blunt or penetrating chest trauma
secondary to neck, thoracic, or retroperitoneal surgery
-
endoscopic intervention
-
tracheobronchial perforation
laceration
bronchoscopy
tracheostomy
laryngeal fracture
-
vigorous exercise (see: pulmonary interstitial emphysema)
childbirth (see: Hamman syndrome)
weightlifting 16
asthma 16
-
barotrauma 16
diving
ventilator: most commonly secondary to ARDS with positive pressure ventilation
inhaled substance use 18
-
infection
cavitating tuberculosis or pneumatoceles
dental or retropharyngeal infection
-
connective tissue disorders 11
polymyositis/dermatomyositis, uncertain if related to vasculopathy or associated interstitial lung disease 12
idiopathic
Although it is rare, pneumomediastinum can occur spontaneously (spontaneous pneumomediastinum). This is considered benign and generally affects young adult males 9,10.
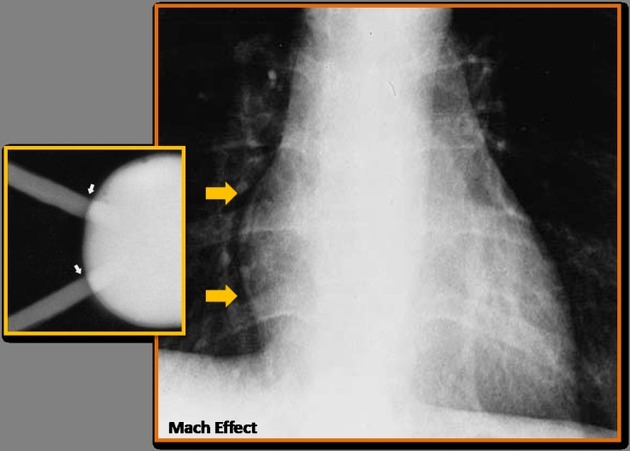
Tension pneumomediastinum is a life-threatening condition which compromises venous return to the heart by selectively compressing the lower pressure right heart chambers (tamponade). The trachea and bronchi can also be compressed and this can affect speech. Gas typically also spreads into the chest wall (and beyond), decreasing compliance and restricting lung ventilation. Any tracheobronchial injury can cause this phenomenon. Alternatively, alveolar rupture with a pressure gradient causing dissection of gas along the peribronchovascular interstitium to the mediastinum (Macklin effect) can cause tension pneumomediastinum. The pressure gradient is increased by coughing, asthma or mechanical ventilation. Tension pneumomediastinum can be fatal, causing cardiovascular collapse 17.
Radiographic features
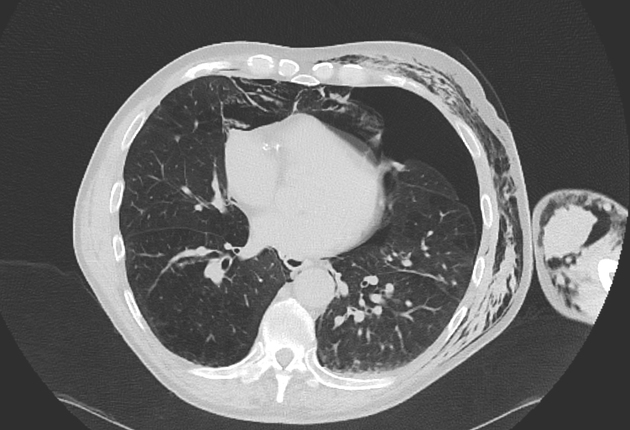
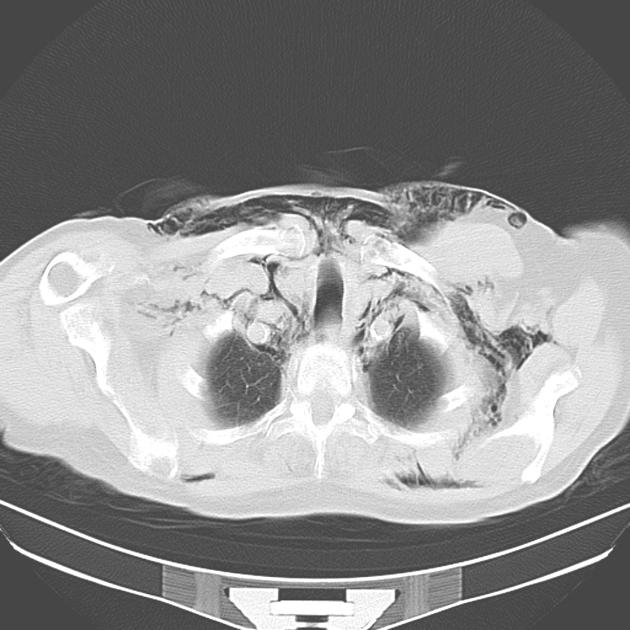
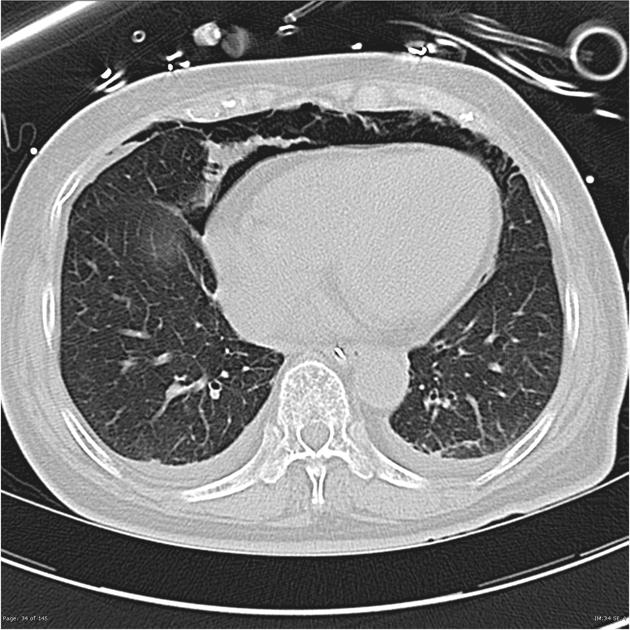
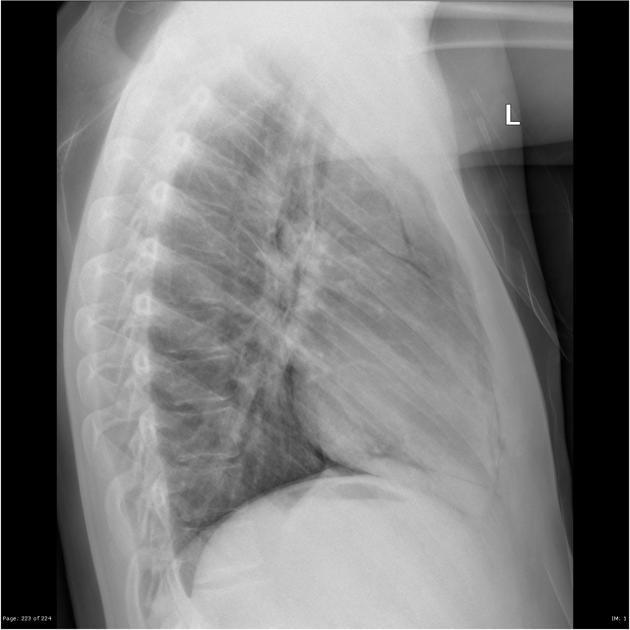
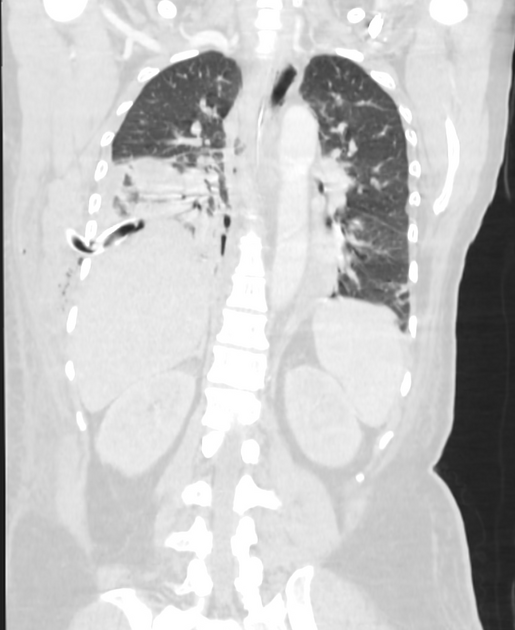
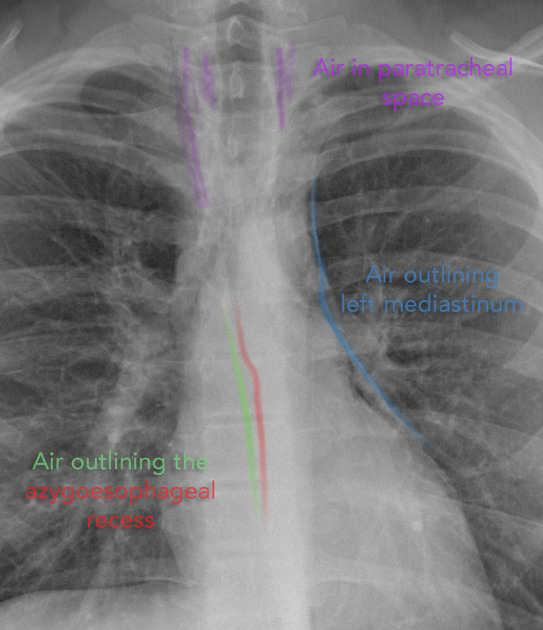
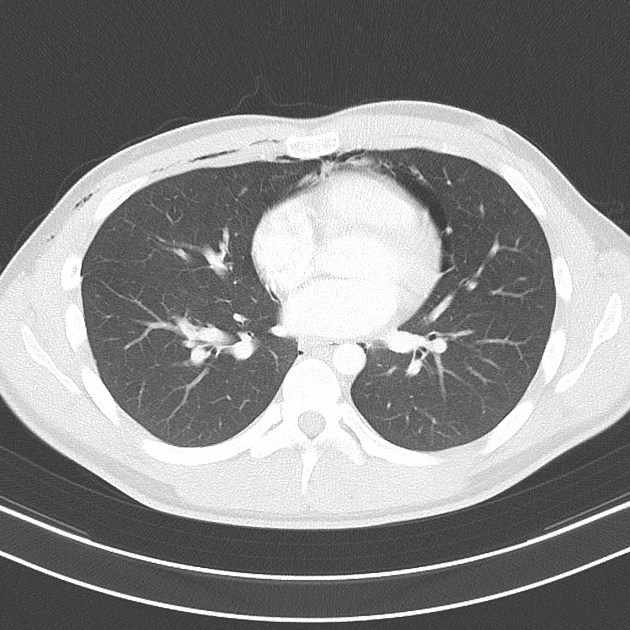
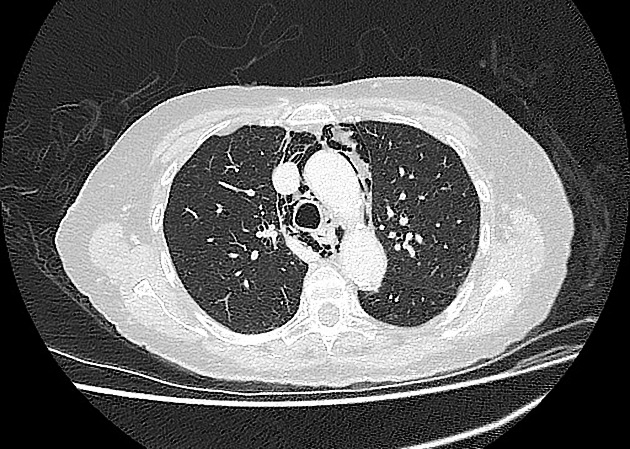
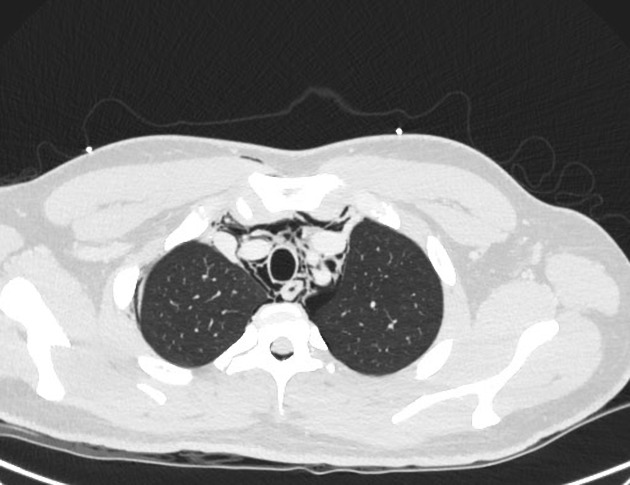
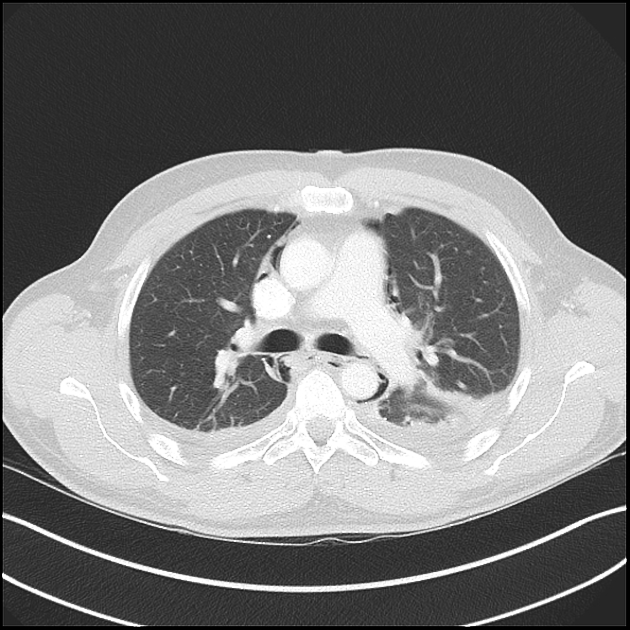
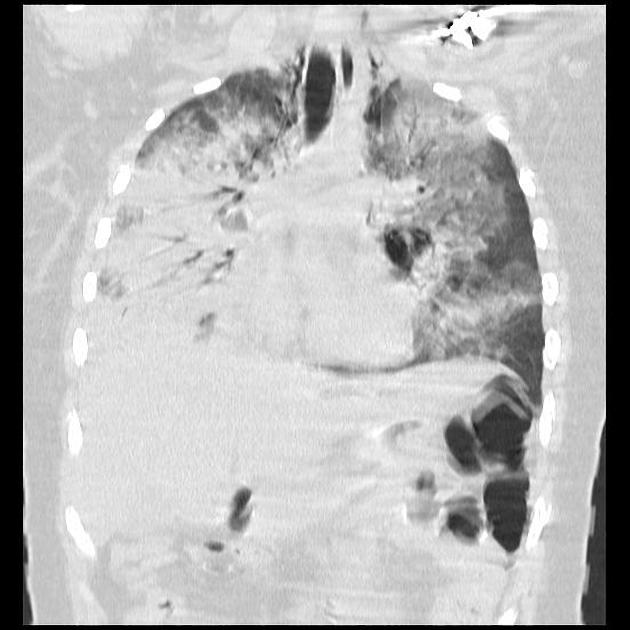
Small amounts of gas appear as linear or curvilinear lucencies outlining mediastinal contours such as:
subcutaneous emphysema
gas anterior to pericardium: pneumopericardium
gas around pulmonary artery and main branches: ring around artery sign
gas outlining major aortic branches: tubular artery sign
gas outlining bronchial wall: double bronchial wall sign
continuous diaphragm sign: due to gas trapped posterior to pericardium
gas between parietal pleura and diaphragm: extrapleural air sign
gas in pulmonary ligament
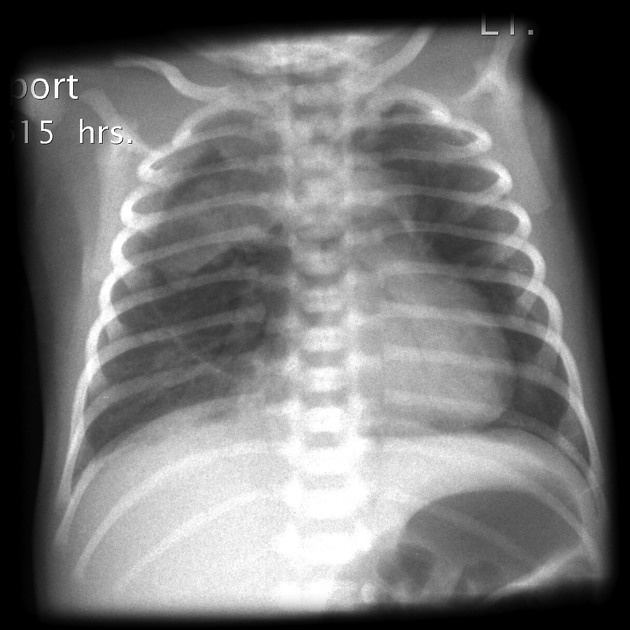
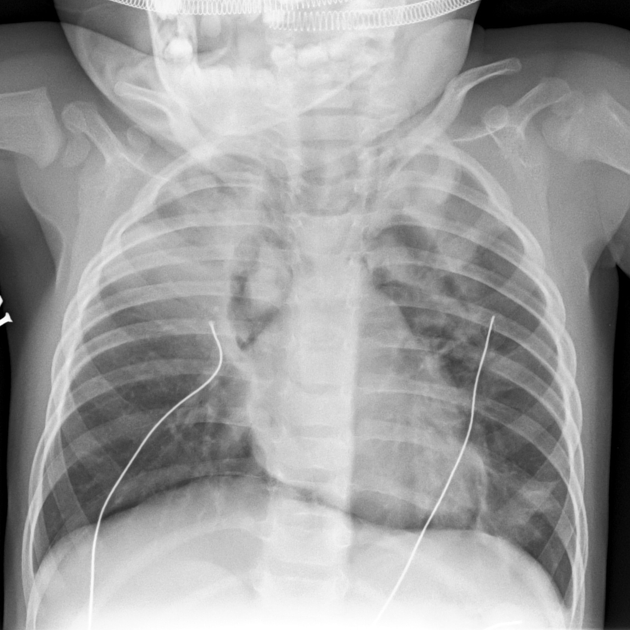
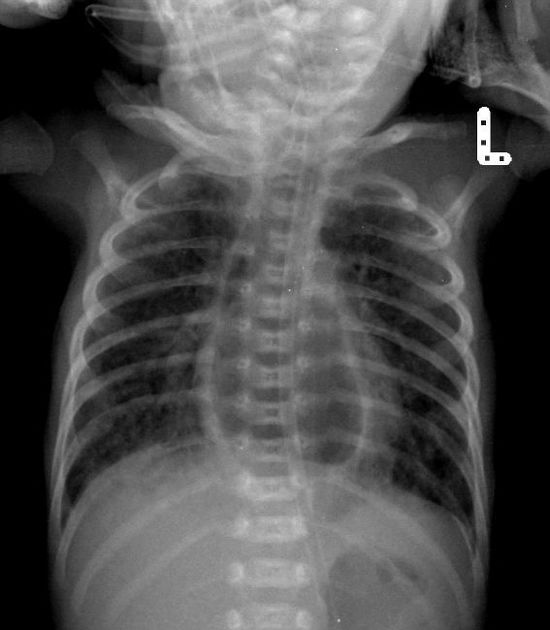
Pediatric pneumomediastinum may have slightly different appearances:
elevated thymus: thymic wing sign
gas crossing the superior mediastinum: haystack sign (the heart appears like a haystack in a Monet painting)
Ultrasound
Sonography is not a diagnostic modality of choice but is often used in the initial workup of undifferentiated trauma patients, or in differentiating causes of dyspnea or chest pain. Sonographic features which may appear in pneumomediastinum include 14:
-
cervical subcutaneous emphysema
anterior cervical ultrasonography demonstrates hyperechoic foci with "dirty" posterior acoustic shadowing
typically found anterior or lateral to the thyroid and medial to the internal jugular vein
-
loss of the parasternal and apical views when performing transthoracic echocardiography
with preservation of the subxiphoid window
-
the air gap sign
originally described using M-mode, describes systolic obscuration of cardiac structures as viewed from a parasternal long axis view 15
cyclic appearance of a dense band of horizontal reverberation artifacts which were discontinuous in the far field
Treatment and prognosis
Most pneumomediastinum requires no treatment, with the air being gradually absorbed on the following days.
Tension pneumomediastinum can cause fatal cardiac tamponade and may require urgent decompression through mediastinal drains 15.
Differential diagnosis
Must be distinguished most importantly from:
medial pneumothorax
For small gas collections on a CT scan, also consider 3:














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.